Cholesterol (Serum Cholesterol)
Serum Cholesterol
What sample is needed for Serum Cholesterol?
- The best sample is obtained after 12 hours of fasting, which corresponds to the morning sample.
- The best sample is serum separated within 2 hours of the collection.
- This test may be performed on Serum or Plasma (EDTA), but not on oxalate, citrate, or fluoride.
- The serum is stable at 4 °C for 5 to 7 days and 3 months at -20 °C.
- Avoid freezing and thawing.
- The result with EDTA plasma is 3% lower than serum.
- Samples with Cholesterol above 500 mg/dL should be diluted.
What are the precautions for serum cholesterol?
- Try to separate serum or plasma from the cells within 2 hours.
- The best sample is after 12 to 14 hours of fasting.
- Pregnancy may give a high level.
- Drugs that may increase the level are anabolic steroids, corticosteroids, oral contraceptives, vitamin D, phenytoin, thiazide diuretics, and cyclosporin.
- Drugs that may decrease the level include captopril, colchicine, erythromycin, isoniazid (INH), lovastatin, neomycin, bile salt-binding agents, androgens, niacin, and nitrates.
What are the Indications for serum cholesterol?
- Cholesterol level is estimated to determine the coronary artery disease risk.
- This test may be needed to rule out hyperlipidemia.
How will you discuss the pathophysiology of serum cholesterol?
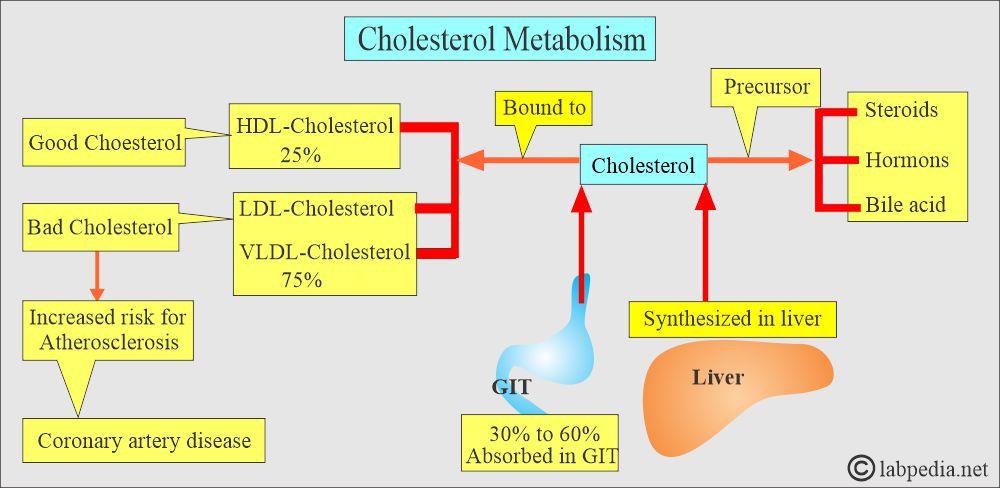
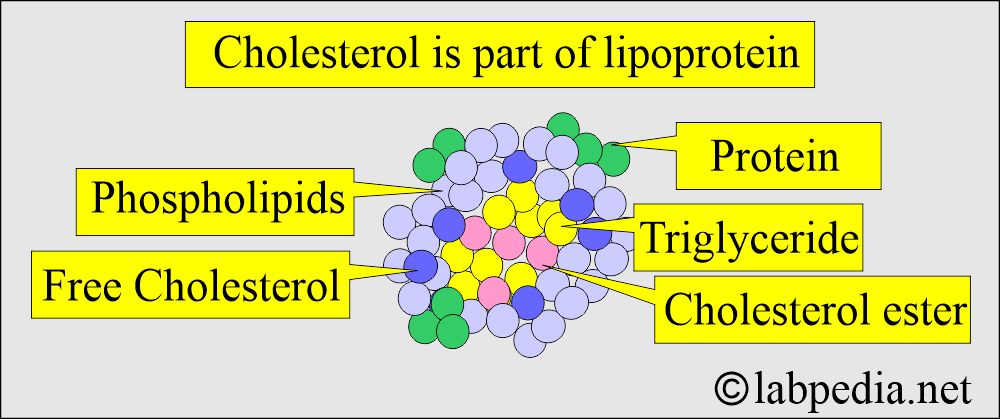
- Total serum cholesterol comprises all of the Cholesterol found in the various lipoproteins.
- Cholesterol is an organic molecule, a sterol or modified steroid, a type of lipid.
- This is an essential part of all cell membranes.
- Cholesterol is the major component of LDL and a minority part of VLDL and HDL.
- Cholesterol is the best-known steroid because of its association with atherosclerosis.
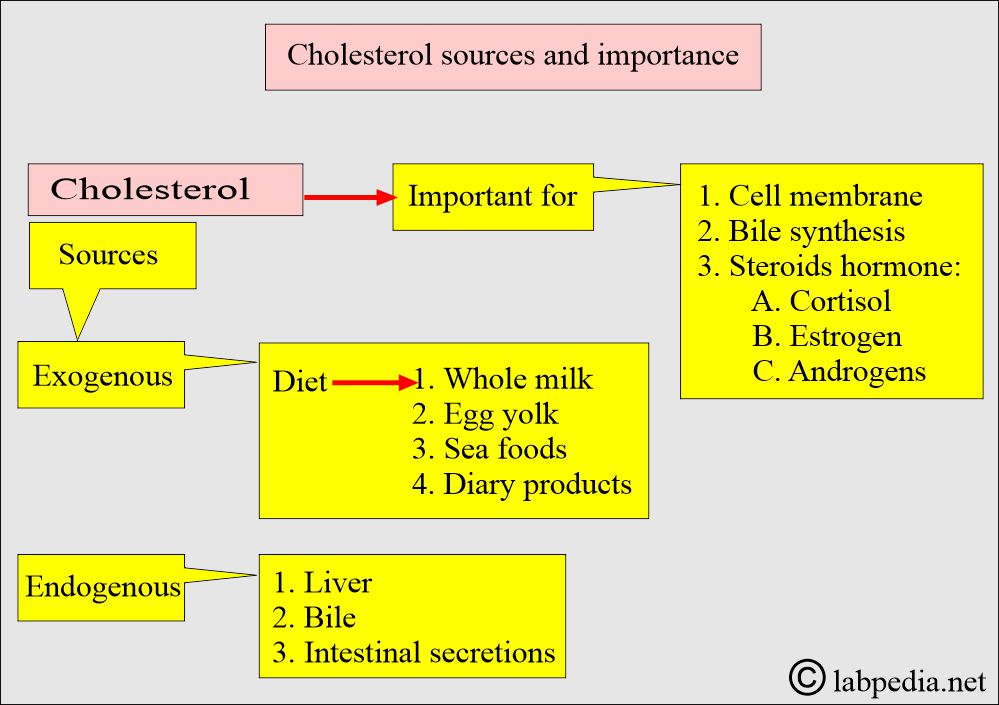
- Cholesterol has biochemical significance because it is the precursor for important steroids, including bile acids, adrenocortical hormones, sex hormones, Vitamin D, cardiac glycosides, sitosterol found in the plant kingdom, and some alkaloids.
- Cholesterol is a steroid alcohol with 27 carbon atoms.
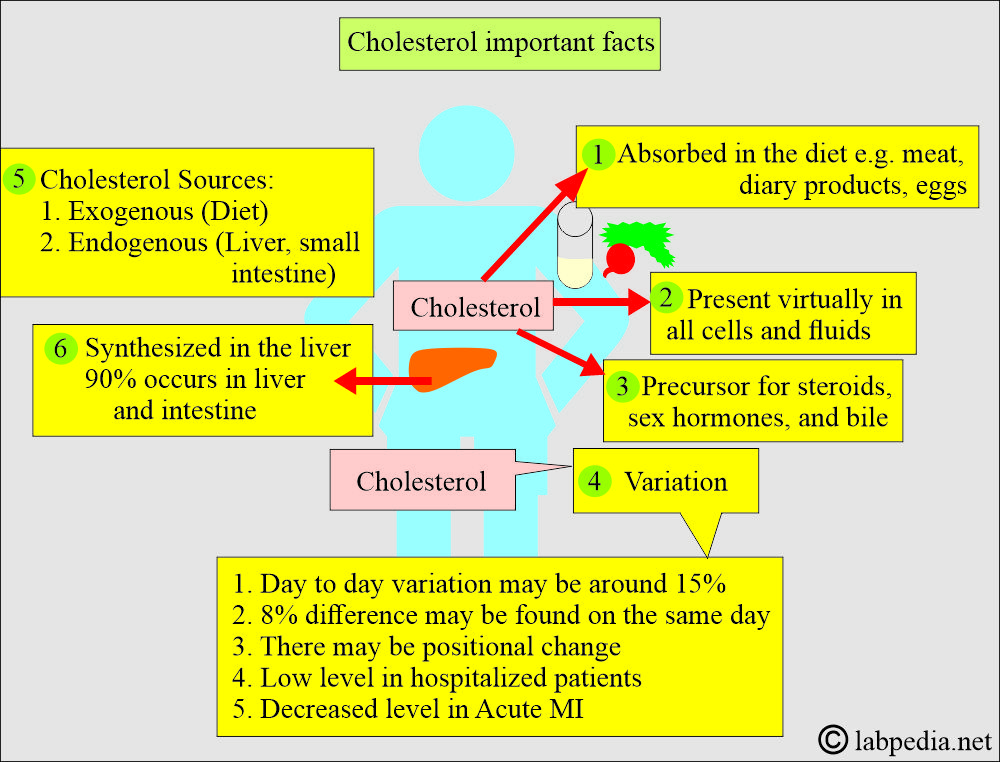
- Cholesterol is present virtually in all cells and body fluids.
- Cholesterol is absorbed in the diet and synthesized in the liver and gut.
- It is a precursor of steroid hormones, bile acids, sex hormones, and cellular membranes.
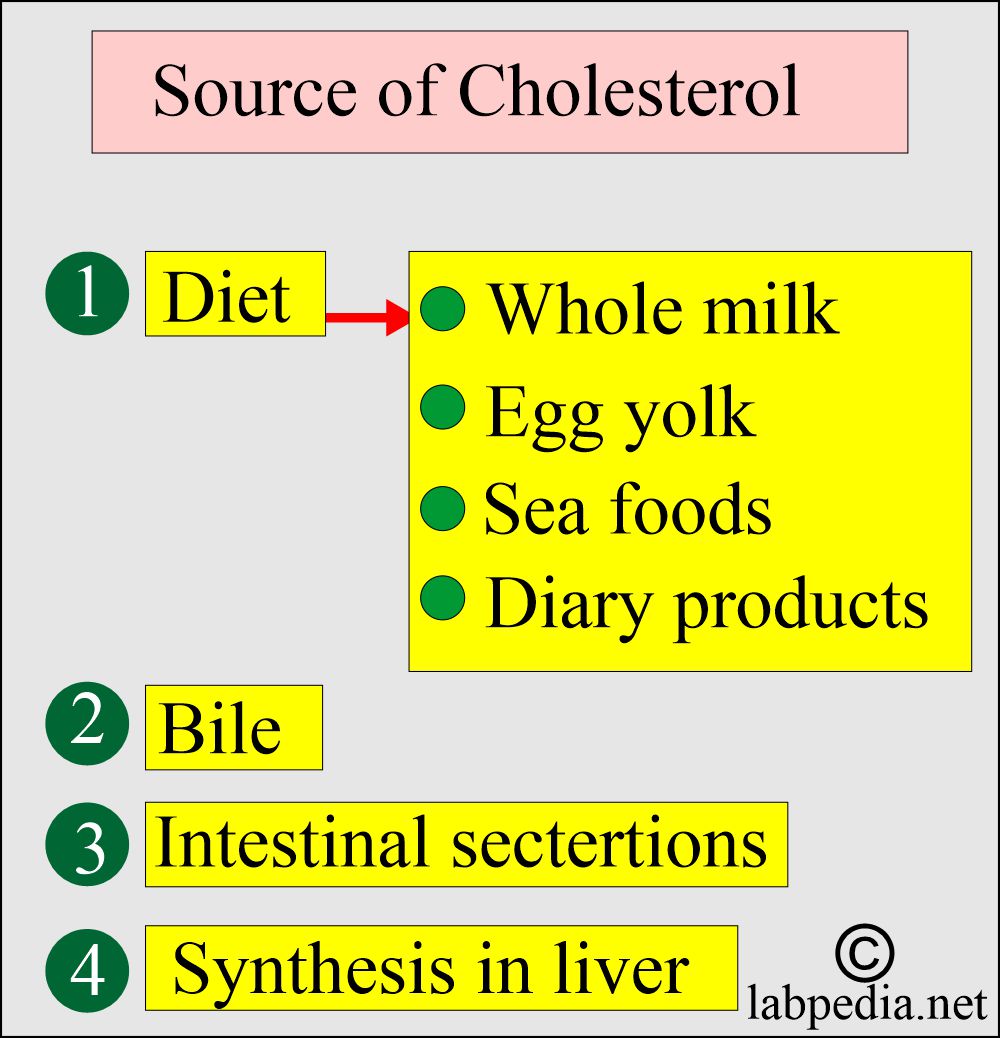
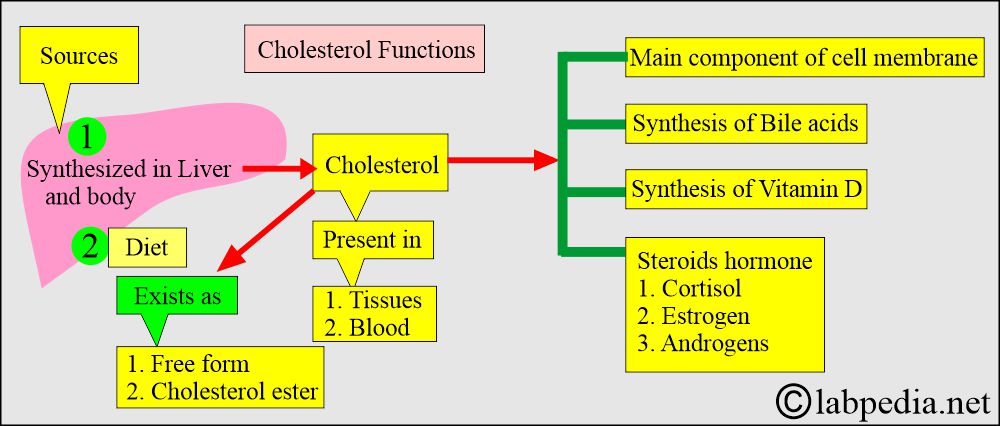
What are the sources of Cholesterol?
- Cholesterol sources:
- Exogenous sources are present in the diet, mainly from animal sources, and absorbed by the gastrointestinal tract.
- Endogenous sources are like the liver and other tissues.
- All cells can synthesize Cholesterol, with 90% of the process occurring in the liver and intestines.
- Malnutrition will result in low cholesterol formation.
What is the cholesterol in the body, and how is it calculated from the LDL-cholesterol formula?
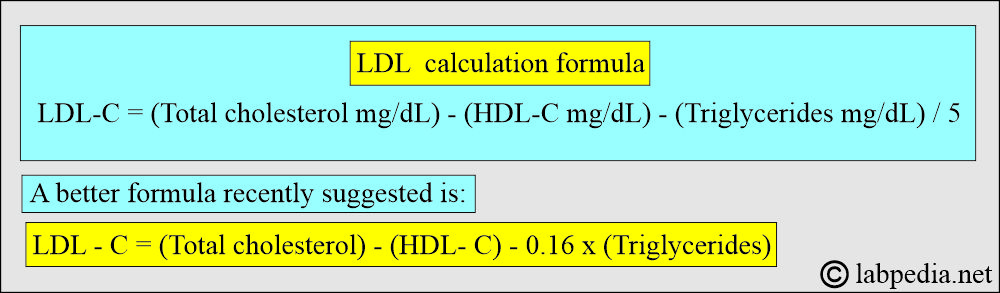
- Three different lipoproteins carry Cholesterol in the fasting serum. So, the total cholesterol sum equals the sum of these three components.
- Total cholesterol = HDL-cholesterol + VLDL-cholesterol + LDL-cholesterol
- The amount of Cholesterol in the HDL fraction can be found by precipitating from the serum.
- The level of Cholesterol in VLDL = Triglycerides/5
- This formula works in the fasting sample and when:
- The triglycerides are <400 mg/dL.
- No chylomicrons are seen.
- Does not work in type III dyslipidemia (β-VLDL).
- LDL – Cholesterol = The separation of LDL from the lipoproteins is very difficult, so the Friedewald equation is used, which is:
- LDL-cholesterol = (Total cholesterol mg/dL) – (HDL-cholesterol mg/dL) – (triglycerides mg/dl)/5.
What are the causes of changes in cholesterol levels? changes in the body and its distribution along with other lipoproteins:
- There is a day-to-day variation in the cholesterol level.
- This day-to-day variation may be seen in persons around 15%.
- An 8% difference can be found on the same day.
- There is a positional change in the level.
- The level may be decreased by as much as 15% in the recumbent position.
- There is a low level in the hospitalized patient.
- Because of these variations, two samples must be tested for heart disease risk.
- There is a decrease in cholesterol level in acute MI, as much as 50% for 6 to 8 weeks.
How will you summarize the Cholesterol distribution in the lipoproteins?
| Type of lipoprotein | Cholesterol | Triglycerides | Phospholipids | Proteins |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
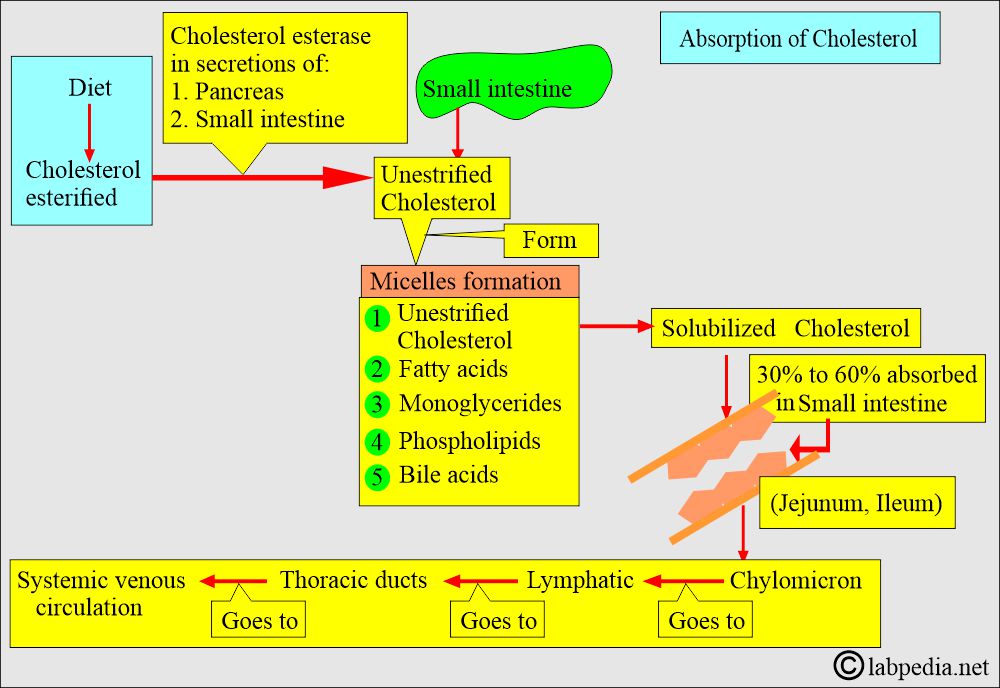
What is the mechanism of Cholesterol absorption?
- The primary source of Cholesterol is diet. Another source is endogenous.
- Cholesterol is an important constituent in the assembly of the cell membrane.
- Cholesterol is the basic part of synthesizing bile acids and steroid hormones (cortisol, estrogen, androgen).
- In the normal biological process, Cholesterol undergoes changes like synthesis, recycling, and degradation.
- Cholesterol enters the intestine from the following sources:
- For foods like egg yolks, meat, dairy products, and seafood, the average amount is 400 to 700 mg/day.
- Plant sterols (200 to 300 mg) are ingested daily. These are poorly absorbed.
- Bile provides another fraction of Cholesterol.
- Intestinal secretions and turnover of the intestinal mucosal cells are other sources.
- Bile acids are detergents and are the most critical factor affecting micelle formation.
- Without bile acids, the digestion and absorption of Cholesterol and triglycerides are severely affected.
- Most cholesterol absorption takes place in the jejunum and ileum.
- When Cholesterol enters the intestinal cells, it is packaged with triglycerides, phospholipids, and apolipoproteins into large lipoproteins called chylomicrons.
- An increased amount of fat in the diet, particularly triglycerides 98%, will result in more micelle formation, allowing more Cholesterol to be solubilized and absorbed.
- Approximately 60% of the total Cholesterol in the male plasma is carried by LDL 22%, HDL 13%, and Chylomicrons 5%.
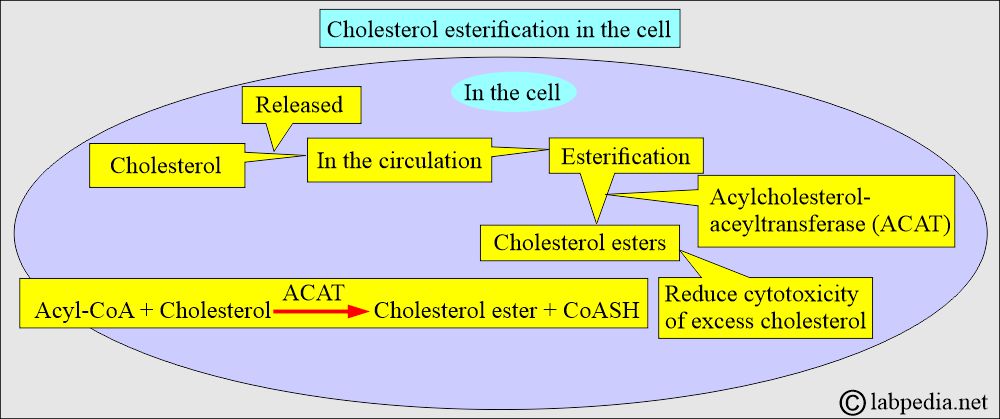
How will the esterification of Cholesterol take place?
- Cholesterol is esterified to fatty acids to form a cholesterol ester by two enzymes:
- In the cells:
- In the cells, excess cholesterol is esterified by acyl-cholesterol acyltransferase (ACAT), forming cholesteryl ester.
- This process will help to prevent the toxicity of excess cholesterol.
- Cholesteryl esters are stored in the cells as lipid droplets.
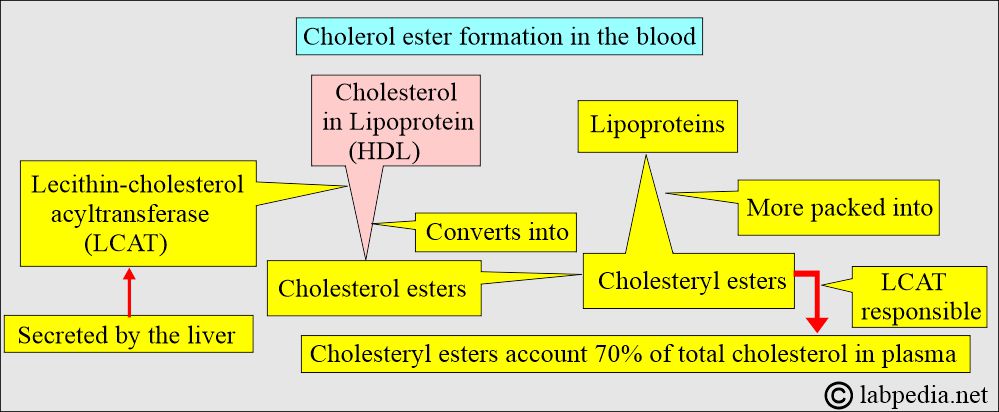
- In blood circulation:
- Cholesteryl esters also form by the action of lecithin cholesterol acyltransferase (LCAT) on cholesterol in lipoproteins, particularly High-density lipoprotein (HDL).
- LCAT is responsible for the conversion of cholesterol into ester.
- LCAT is secreted by the liver into the blood circulation and activated by the apolipoprotein A-1, the main component protein of HDL.
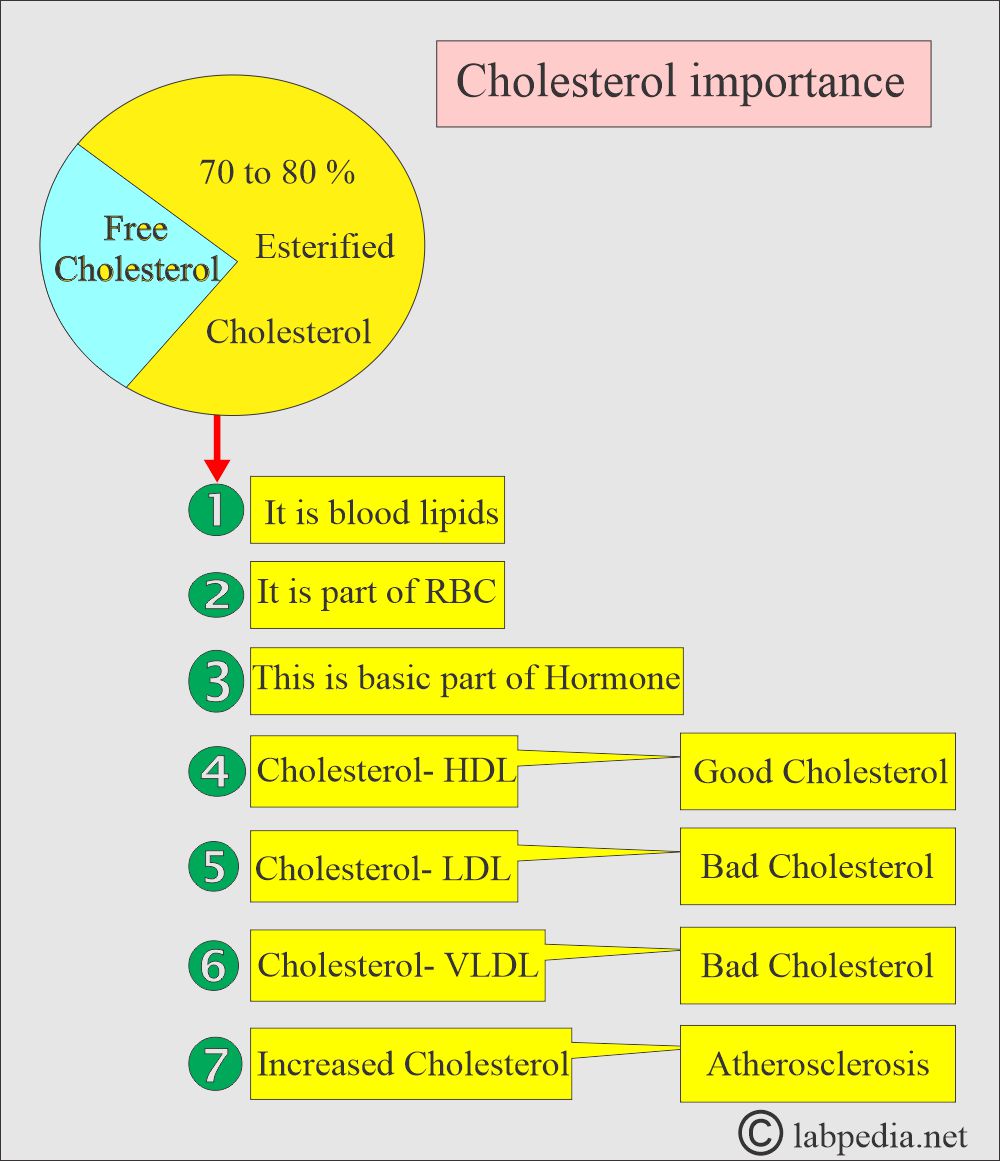
- Cholesterol esters account for approximately 70% of the total cholesterol in the blood.
- Cholesterol, once formed, enters the blood circulation.
- Cholesterol is esterified and combined with apoprotein and apolipoprotein and ultimately carried as a lipoprotein.
- Cholesterol esterification helps in the packing of Cholesterol into lipoproteins.
- Both dietary and synthesized Cholesterol are converted into cholesteryl esters, which can be easily packed into lipoproteins.
- Esterification increases the lipid-carrying capacity of the lipoproteins in plasma and prevents the toxic effects of Cholesterol.
- 75% bound to LDL.
- 25% bound to HDL.
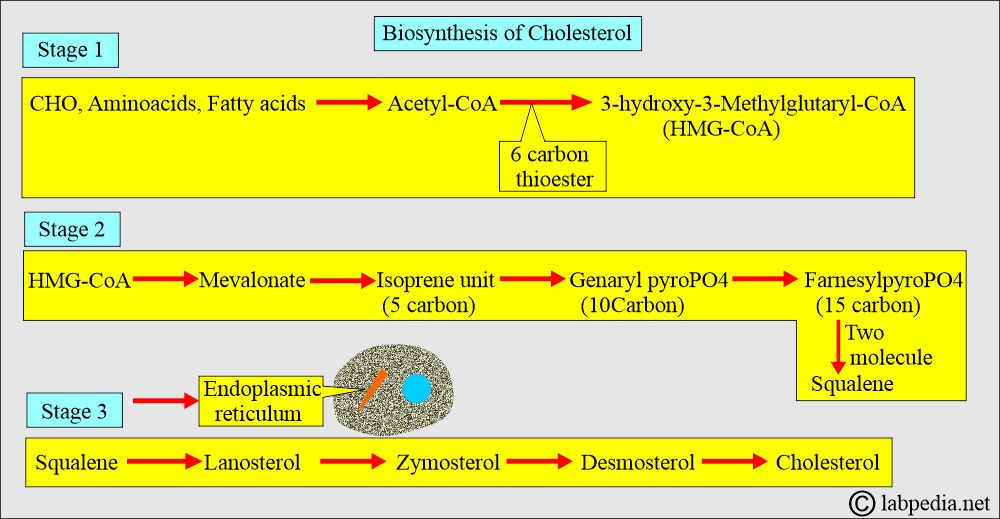
How will you discuss the Biosynthesis of Cholesterol?
- 90% of cholesterol synthesis takes place in the liver and gut.
- Cholesterol synthesis takes place in three stages.
- The starting molecule is acetate.
- All body cells have the ability to synthesize Cholesterol from acetyl-CoA.
- Knowing the endogenous synthesis of Cholesterol, drugs have been developed that lower the cholesterol level, such as mevastatin, lovastatin, simvastatin, pravastatin, and atorvastatin, which suppress the HMG-CoA reductase.
What are the forms of Cholesterol?
- Free Cholesterol.
- Esterified Cholesterol.
- 75% to 85% of the total Cholesterol is in the form of esterified Cholesterol.
- Cholesterol can be derived from dietary sources, such as meat, eggs, butter, and plants.
- 30% to 60% of dietary Cholesterol is absorbed.
- Once Cholesterol is absorbed into the mucosal cells, it becomes part of the large micelle called Chylomicron.
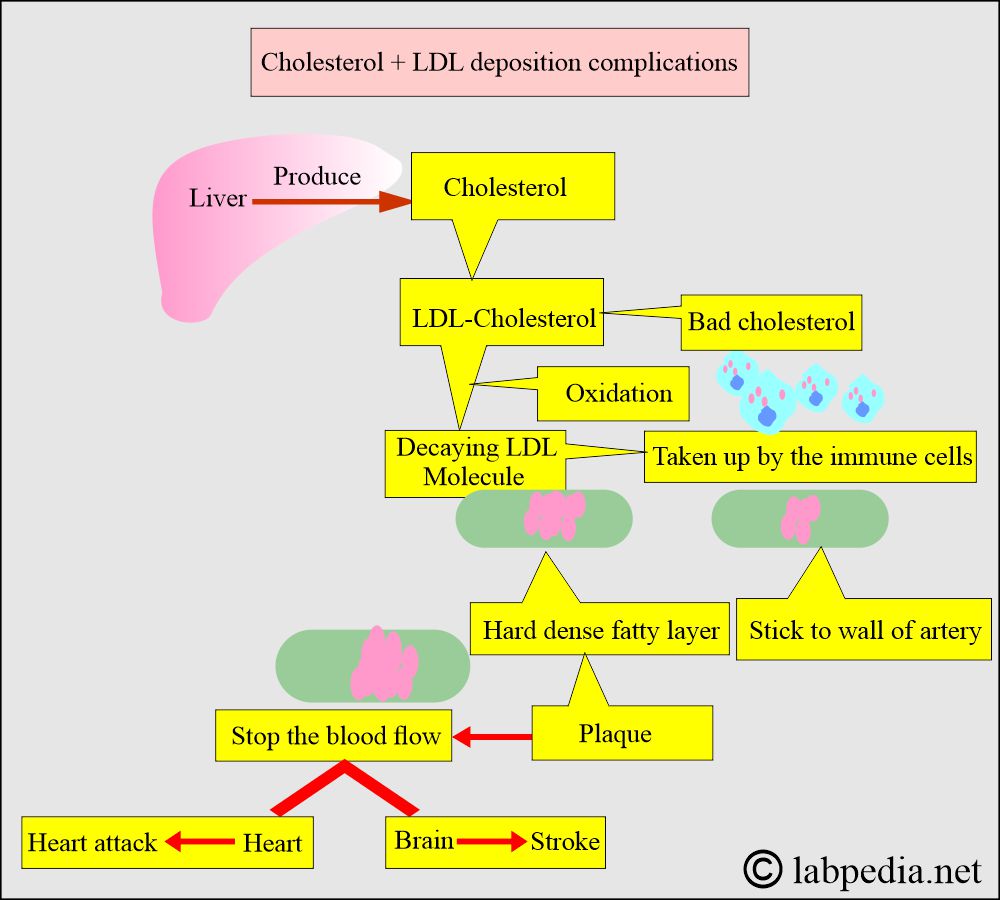
What are the complications due to Cholesterol?
- Cholesterol’s main complication is atherosclerosis, which leads to heart disease and stroke.
What is the distribution of the lipids?
| Cholesterol is found in: | Cholesterol % in other lipids |
|
|
|
|
|
|
|
|
What are the functions of Cholesterol?
- Cholesterol is a blood lipid (fat).
- Cholesterol is a normal part of RBC.
- Cholesterol, when increased, leads to atherosclerosis and is the main lipid.
- A total raised level of Cholesterol is associated with an increased risk of cardiovascular disease.
- Its subtypes, LDL-C and HDL-C, are more important than the total Cholesterol.
- Cholesterol is the basic unit of a hormone produced by the adrenal glands, ovaries, and testes.
- Cholesterol is needed for bile acids and cellular membranes.
- Cholesterol is transported in circulation by carrier proteins.
- Cholesterol bound to high-density lipoprotein (HDL-cholesterol) is known as good Cholesterol.
- HDL will prevent atherosclerosis.
- Cholesterol bound to low-density protein (LDL-cholesterol) is known as bad Cholesterol.
- It increases the chances of atherosclerosis.
- Additionally, the same is true for Cholesterol bound to very low-density lipoprotein (VLDL), which is considered bad Cholesterol.
- Increased Cholesterol level is associated with atherosclerosis and coronary vascular disease.
- It is needed to form steroids, sex hormones, and bile acids.
- This is part of the cellular membranes.
- It increases the risk of heart disease.
What is the normal level of Cholesterol?
Source 1
Adult
- The desired level to prevent coronary disease is < 200 mg/dl
- Moderate risk is 200-239 mg/dl
- High risk is > 240 mg/dl
- CSF <0.5 mg/dl
Source 2
| Sample | Male mg /dL | Female mg /dL |
| Cord blood | 44 to 103 | 50 to 108 |
| 0 to 4 years | 114 to 203 | 112 to 200 |
| 5 to 9 years | 121 to 203 | 126 to 205 |
| 10 to 14 years | 119 to 202 | 124 to 201 |
| 20 to 24 years | 124 to 218 | 122 to 216 |
| 30 to 34 years | 138 to 254 | 130 to 230 |
| 40 to 44 years | 151 to 268 | 147 to 252 |
| 50 to 54 years | 158 to 277 | 162 to 285 |
| 60 to 64 years | 159 to 276 | 172 to 297 |
| >70 years | 144 to 265 | 173 to 280 |
- To convert into SI unit x 0.0259 = mmol/L
What is the relation between Cholesterol and heart disease?
- Desirable level is = <170 mg/dl
- Moderate risk is = 170-199 mg/dl
- High risk is = > 200 mg/dl
- Above 240 mg/dL = requires treatment.
- Nowadays, the Cardiology Association recommends the level to be around 160 mg/dl.
| Cholesterol mg/dL | Risk |
|
|
|
|
|
|
|
|
|
|
- According to the latest NHS research study, there is no relation between total cholesterol and heart disease risk.
What is the recommendation of the ATP III (Adult Treatment Panel) for blood lipids?
| Chemical substance (Lipid) | Clinical effects on the people |
|
|
|
|
|
|
What is the recommendation of the ATP III (Adult Treatment Panel) for the LDL target level in patients with coronary vascular disease?
| Risk factors | Details of risk factors | The target LDL level required ( This level is mandatory) |
|
CHD heart disease risk factors are:
|
|
|
Major risk factors include:
|
|
|
|
How will you apply the Framingham formula calculations (Risk score counting)?
| Risk factors | Points for the calculation for women | Points for the calculation for men |
|
|
|
|
Cholesterol 20 to 39 years = <160 mg/dL
Cholesterol 40 to 49 years = <160 mg/dL
Cholesterol 50 to 59 years = <160 mg/dL
Cholesterol 60 to 69 years = <160 mg/dL
Cholesterol 70 to 79 years = <160 mg/dL
|
Age 20 to 29 years
Age 40 to 49 years
Age 50 to 59 years
Age 60 to 69 years
Age 70 to 79 years
|
|
|
|
|
|
|
|
|
|
|
Not treated = -3 Treated = -1 Not treated = 2 Treated = 2
|
Not treated = -2 Treated = 0 |
What is the 10-year risk for cardiovascular diseases according to the Framingham risk in %?
| Total points | % Framingham score (risk) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the relationship of Total Cholesterol to coronary artery disease?
- Another source:
- Desirable level = <200 mg/dL
- Borderline level = 200 to 239 mg/dL
- High Risk level = >240 mg/dL
What is the risk of Cholesterol and triglycerides for coronary artery disease (NCEP expert panel and ATP III guideline)?
| Risk factors grades | Total cholesterol | Total triglycerides | Total cholesterol/HDL-C ratio | LDL/HDL ratio |
|
|
|
|
|
|
|
|
||
|
|
|
7.1 to 11.0 |
|
|
|
|
|
|
What are the optimal values for lipids (according to the ATP III guidelines)?
| Risk level | LDL-cholesterol | Total cholesterol | Triglycerides | HDL-cholesterol |
|
|
|
|
|
|
|
|||
|
|
|||
|
|
|||
|
|
What are the causes of increased Cholesterol (Hypercholesterolemia)?
- Familial combined hyperlipidemia.
- Hyperlipoproteinemia type IV, V.
- Intra- and extrahepatic cholestasis.
- Glomerulonephritis.
- Nephrotic syndrome and chronic renal failure.
- Malignant neoplasm of the pancreas and prostate.
- Hypothyroidism.
- Gout.
- Diabetes mellitus.
- Alcoholism.
- Glycogen storage disease type 1 (Von Gierke disease).
- Stress.
- Biliary cirrhosis.
What are the causes of decreased Cholesterol (Hypocholesterolemia)?
- alpha-Lipoprotein deficiency.
- Hepatocellular necrosis.
- Malignant neoplasm of the liver.
- Hyperthyroidism.
- Malabsorption and malnutrition (starvation).
- Severe acute illness.
- Extensive burns.
- Rheumatoid arthritis.
- Cholesterol-lowering medications.
What is the role of cholesterol in prevention, recommendations, and treatment?
|
|
|
|
|
|
What are the risk factors leading to heart disease?
- Cigarette smoking.
- Cerebrovascular disease.
- Diabetes mellitus.
- Hypertension.
- The family history of coronary heart disease.
- Sex is male.
- Overweight >30%
- peripheral occlusive vascular disease.
What is essential for Cholesterol?
- There is variation in the level of Cholesterol, so take at least two samples.
- Critical value = >500 mg/dL.
Chemical substance Panic value (critical value) - Cholesterol
- >240 mg/dL (>500 mg/dL)
- HDL-cholesterol
- <40 mg/dL
- LDL- cholesterol
- >160 mg/dL
- Triglycerides
- >500 mg/dL

I agree with you
Thanks
[…] the liver, cholesterol, and triglycerides are packed into another type of lipoprotein called Very low-density […]