White blood cells:- Part 1 – White Blood Cells (WBC) Development, Functions, and Interpretations
White Blood Cells (WBC)
What sample is needed for White Blood Cells?
- This is done on EDTA blood.
- The whole blood in EDTA is stable for 24 hours at 23° C and 48 hours at 4 °C.
- Don’t use heparin.
What are the indications for White Blood Cells?
- This is the routine test in CBC.
- TLC differentiates acute and chronic infections.
- TLC diagnoses leukemias.
- TLC is done as a follow-up test in patients on chemotherapy.
- This will help a patient with an allergy.
What are the Precautions for White Blood Cells?
- Physical activity and stress may cause an increase in WBCs and differential values.
- Pregnancy in the final months may cause an increase in WBC count.
- Patients with splenectomy have a persistent mild increase in the WBC count.
- Drugs that may increase the WBC county are:
- Aspirin.
- Allopurinol.
- Steroids.
- Quinine.
- Epinephrine.
- Adrenaline.
- Chloroform.
- Heparin.
- Drugs that will decrease the WBC count:
- Antibiotics.
- Anticonvulsant.
- Antimetabolites.
- Antithyroid drugs.
- Diuretics.
- Sulfonamides.
- Barbiturates.
- Chemotherapy.
How will you discuss the pathophysiology of White Blood Cells?
How will you define hematopoiesis?
- This is the dynamic process of blood cell production and development of the various blood cells.
- All these cells develop from the totipotent stem cells.
- The constant turnover of the blood cells characterizes this hematopoiesis.
- The normal hematopoietic system maintains a cell population of erythrocytes, white blood cells, and platelets through a complex network of tissues, stem cells, organs, and regulatory factors.
What are the functions of the hematopoietic components (cells)?
- It transports oxygen and excretes CO2 through RBCs.
- It fights infection by the WBCs.
- It performs the immune function (cellular and humoral immunity) through the lymphocytes.
- It maintains (hemostasis) the bleeding and the clotting process through the platelets.
How will you discuss the development of myeloid (myelopoiesis) /erythroid (erythropoiesis) cells?
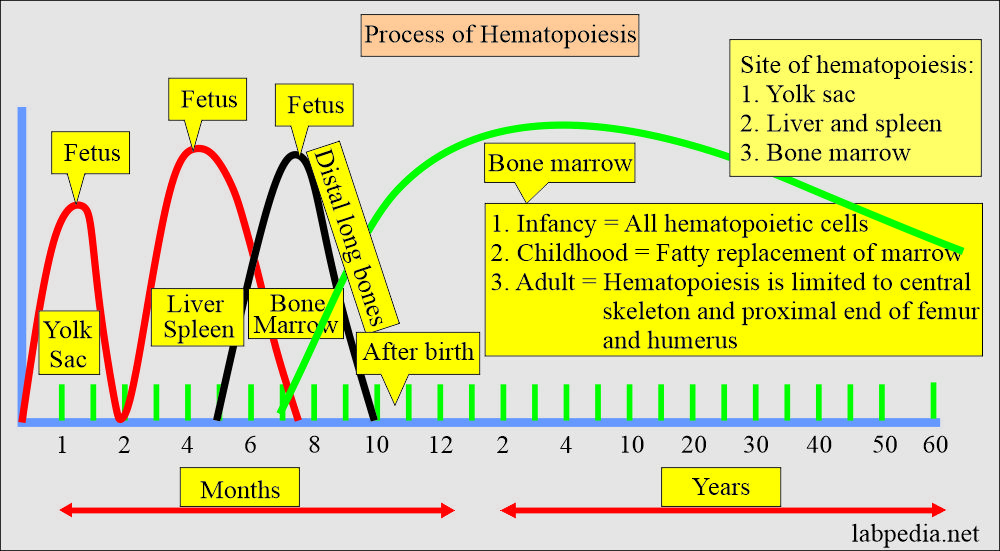
- In the first few weeks of gestation, the yolk sac (mesoderm) is the main site of hematopoiesis. The first stem cells for hemopoiesis are observed in the dorsal aorta, in a region called the aorta-gonads-mesonephros.
- These common precursors of endothelial and hematopoietic cells will seed the bone marrow, liver, and spleen from 6 weeks until 7 months of fetal life.
- The liver and spleen are the major hematopoietic organs and blood cells are produced until around two weeks after birth.
- Marrow is the only source of new blood cells during childhood and adulthood.
- In adult life, the marrow consists of approximately 50% of the fats.
- After 4 years of age, fat cells start appearing in the long bones.
- 18 to 20 years, hematopoiesis is only found in the sternum, ribs, pelvis, vertebra, and skull.
- After 40 years, the sternum, ribs, vertebra, and pelvis comprise 50% fat and 50% hematopoietic tissue.
How will you discuss the bone marrow activity?
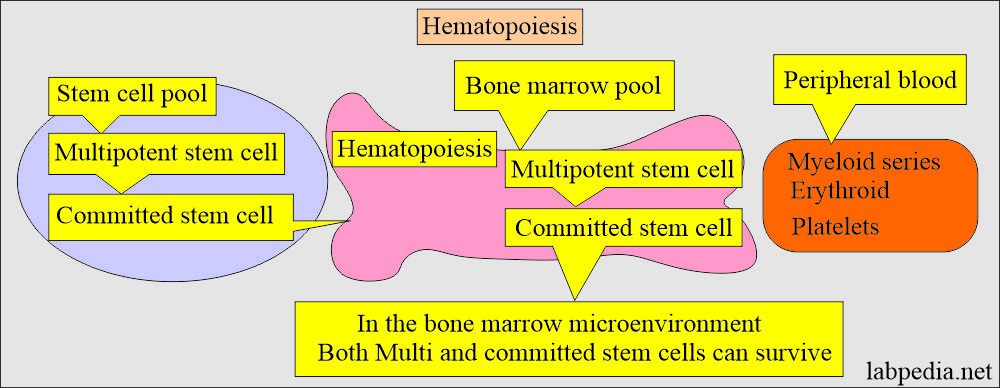
- Bone marrow hematopoietic activity is divided into two pools:
- Stem cells pool.
- Bone marrow pool.
- Eventually, these cells mature and are released into the peripheral blood.
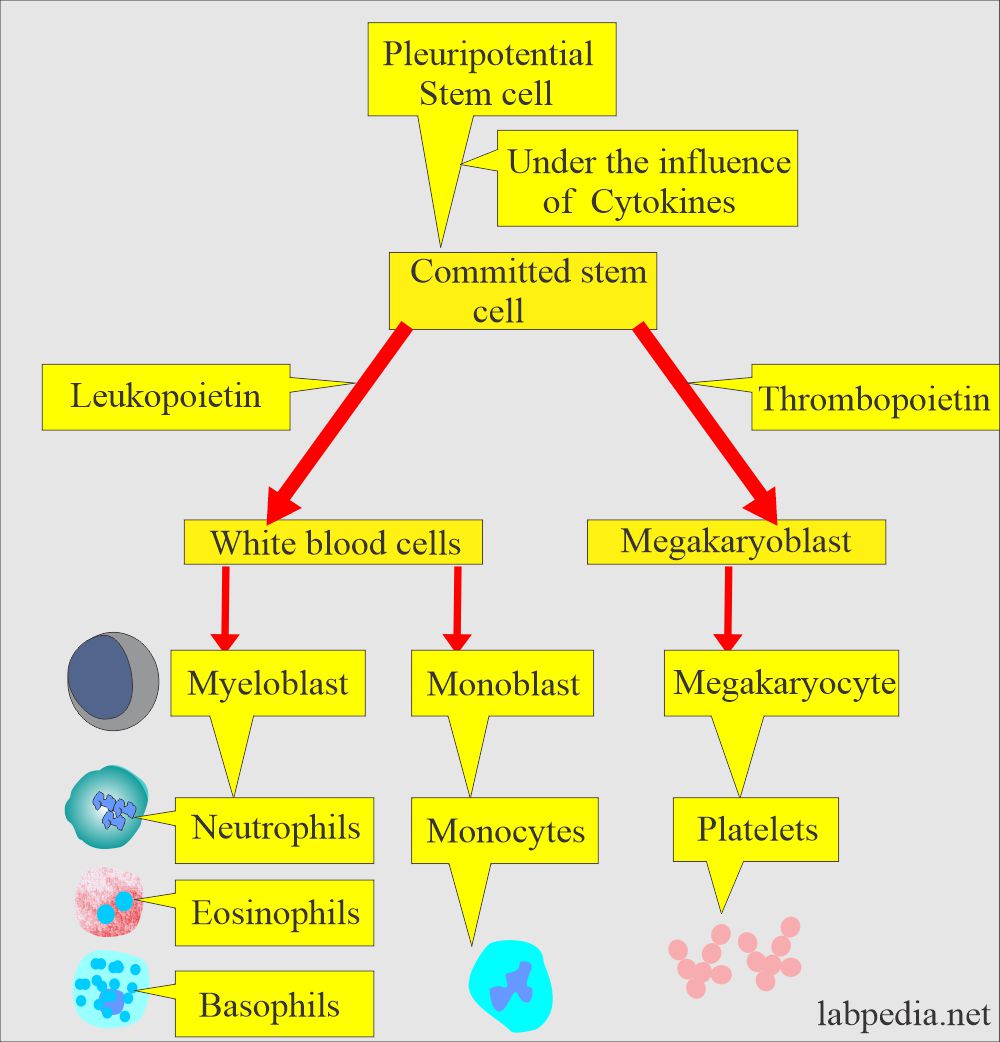
Hematopoiesis:
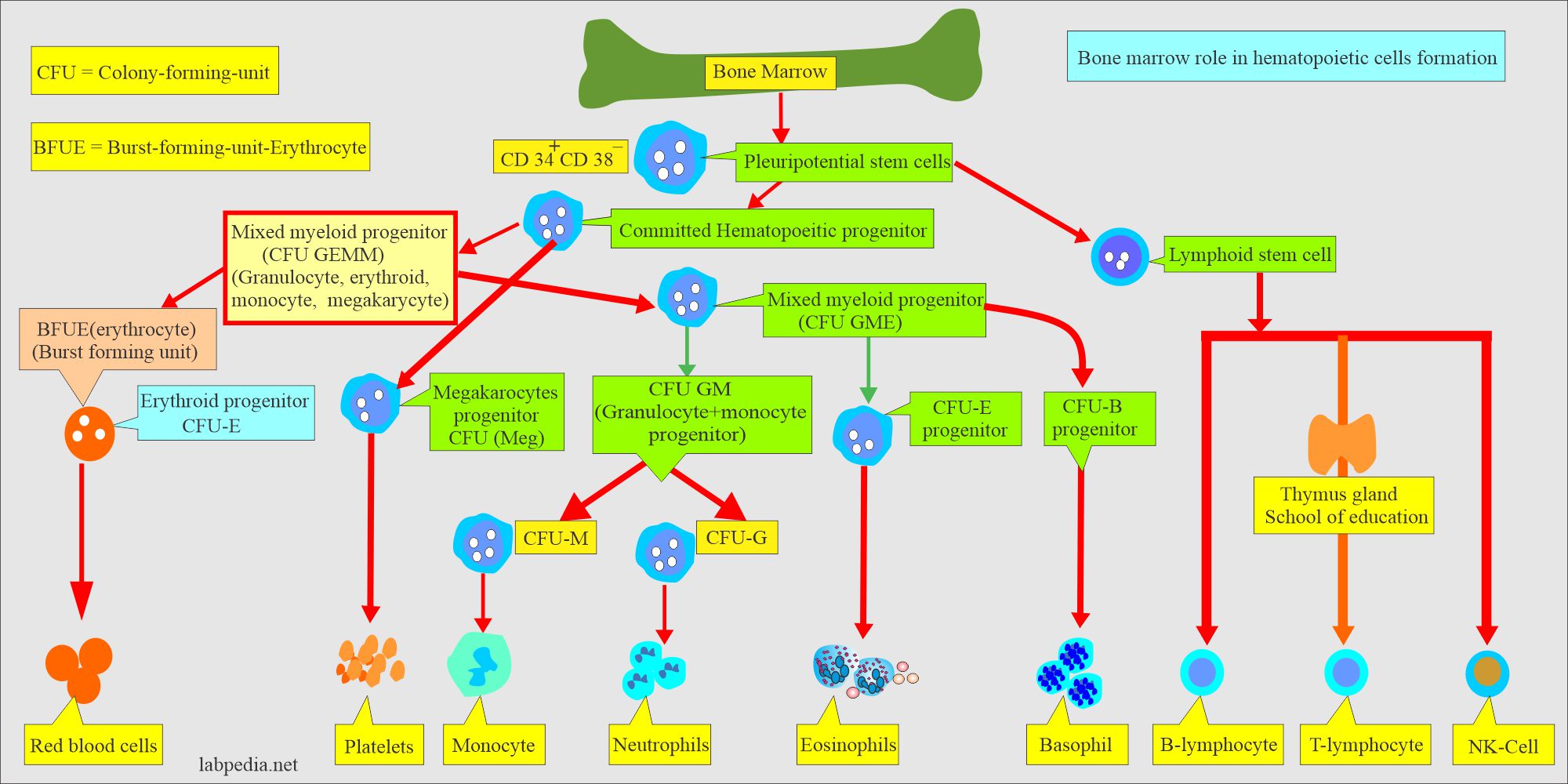
- Hematopoiesis starts from the pluripotential stem cells.
- Hematopoietic stem cells are rare; these are 1 in every 20 million nucleated cells.
- There is self-renewal of the stem cells. So, the bone marrow cellularity remains constant in a normal, healthy person.
- There is an amplification of the stem cells, and one stem cell can produce about 106 mature blood cells after 20 subdivisions.
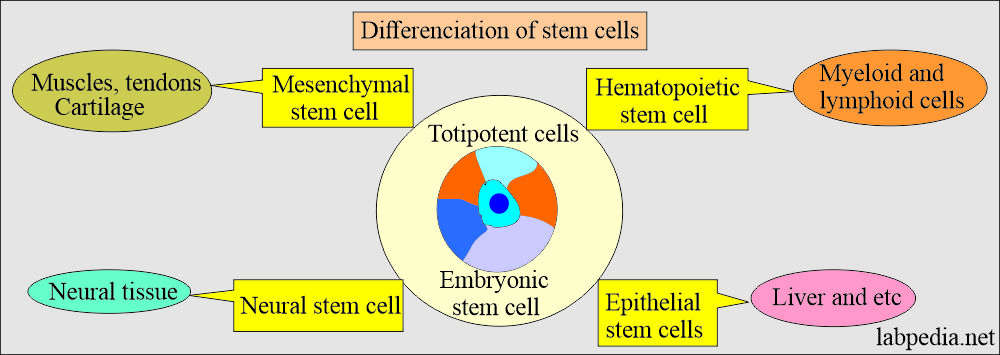
- There are various types of stem cells that develop from the totipotent cells.
- Totipotent cells:
- These are called embryonic stem cells and gave rise to:
- Hematopoietic stem cells give rise to myeloid and lymphoid cells.
- Epithelial stem cells give rise to organs like the liver, etc.
- Mesenchymal stem cells give rise to muscles, tendons, and cartilage.
- Neural stem cells give rise to neural tissue.
- These parent stem cells have CD34+ and CD38– and have the appearance of small, medium-sized lymphocytes.
- These stem cells give rise to committed stem cells, which occur under the influence of CFU (colony-forming unit).
- This whole process is shown in the following diagram.
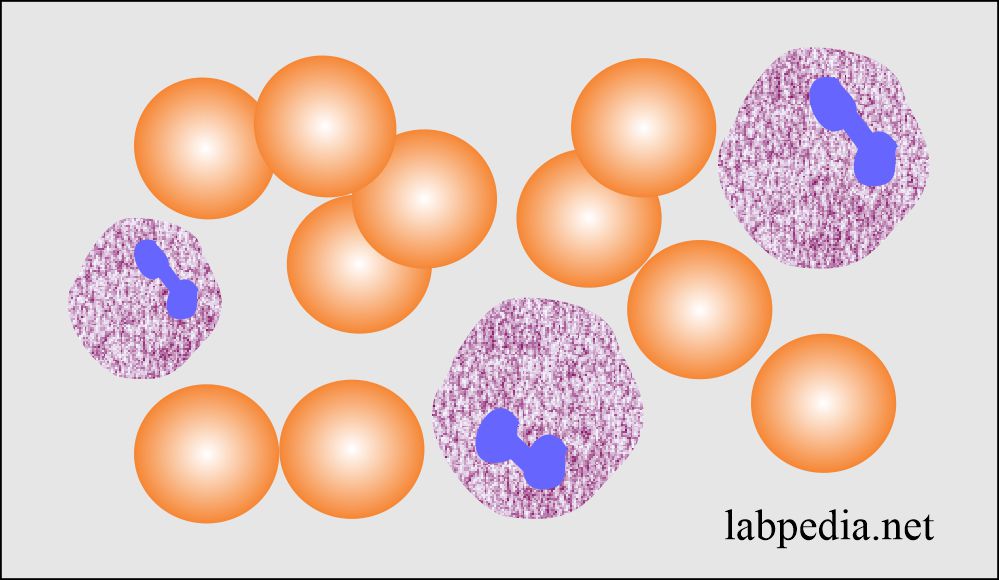
How will you divide White blood cells?
- Granulocytic series:
- These cells contain granules in their cytoplasm. Because of a multilobate nucleus, these are also called polymorphonuclear leukocytes (Polys or PMN). These are of the following types:
- Neutrophils.
- Eosinophils.
- Basophils.
- Agranulocytic series:
- These are without any granules in their cytoplasm. These are also called mononuclear cells. These are :
- Lymphocytes.
- Monocytes.
- Platelets.
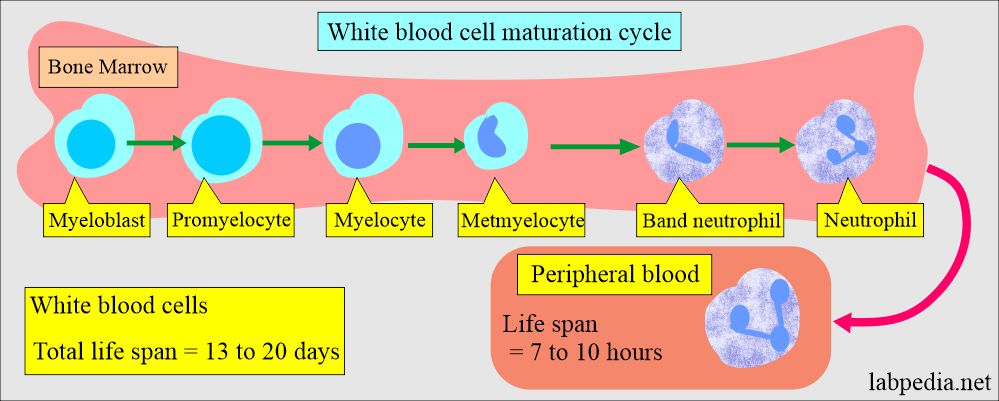
White blood cell maturation
Can you divide White blood cells in another way?
- Phagocytic cells:
- Neutrophils (polymorphonuclear leucocytes, PMN).
- Eosinophils.
- Basophils.
- Monocytes.
- Immunocytic cells:
- Lymphocytes.
- Lymphocytes precursors.
- The Polys and lymphocytes comprise 75% to 90% of the total WBC count.
How will you discuss Polymorphonuclear leukocytes (PMN)?
- The neutrophils develop from the myeloblast, transforming into promyelocytes, myelocytes, metamyelocytes, band forms, and neutrophils delivered into the peripheral blood.
How will you discuss the development of the neutrophils?
- These are also called segmented neutrophils or polymorphonuclear neutrophils (PMN).
- The neutrophils are of two types:
- Segmented neutrophils are found in the peripheral blood.
- The cytoplasm stains light blue and has a fine lattice-like structure.
- Granules vary in number and stain, which will be red to blue.
- These cells have large, round, or oval nuclei with coarse chromatin.
- Nucleoli are conspicuous and stain light blue.
- Tissue neutrophils have ample cytoplasm, irregular, blunt pseudopodia that are often multi-pointed, and may have hazy cytoplasmic streamers.
- These cells are not phagocytic and seldom have cytoplasmic vacuoles.
What are the cytokines involved in these phagocytic cells?
| Growth factors/cytokines | Target cells |
|
|
|
|
|
The precursor of:
|
|
|
|
|
What is the life span of white blood cells?
- The leukocytes’ total lifespan is 13 to 20 days, and they are produced in 7 to 14 days from the myeloblastic cells.
- Their life in the peripheral blood is just 7 to 10 hours, and they migrate to the tissue and are replenished by other cells released from the marrow.
- The polys have a dense nucleus consisting of 2 to 5 lobes and pale cytoplasm, with many fine pink-blue (azurophilic granules) or grey-blue granules present in the lysosomes.
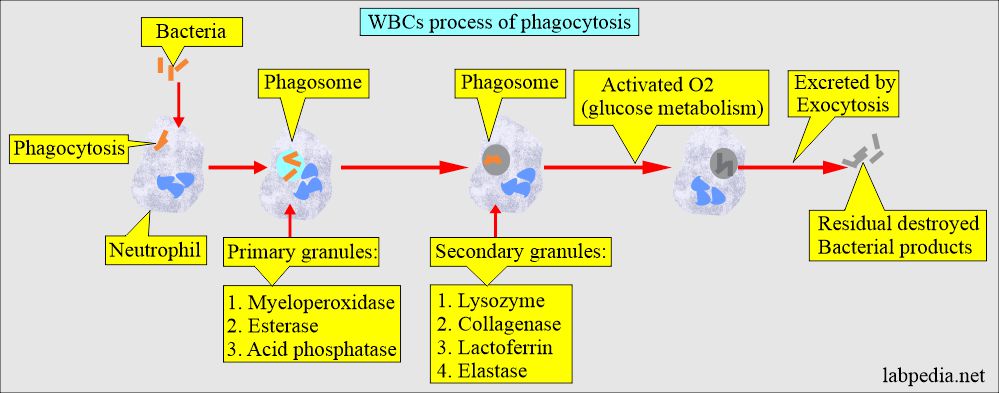
How would you divide White blood cell granules?
- Primary granules appear at the promyelocytic stage.
- These contain myeloperoxidase, acid phosphatase, and other hydrolases.
- Secondary (specific) granules appear at the myelocytic stage and predominate in the mature neutrophils.
- These granules contain collagenase, lactoferrin, and lysozyme.
What is the role of the lysosomal enzyme in destroying the bacteria by the neutrophils?
- Bacteria are phagocytosed into cells and fuse with the primary lysosomes to form a phagosome.
- Primary granules attack the bacteria.
- Secondary granules fuse with the phagosomes, and secondary enzymes attack the bacteria.
- Activated oxygen generated by glucose metabolism will kill the bacteria.
- Undigested, killed residual bacterial products are excreted by exocytosis.
What are the functions of Poly (PMN)?
- The poly (PMN) gives immunity by fighting against infections and reacting against foreign bodies by various methods:
- Phagocytosis is the killing and digestion of bacteria.
- Eosinophils are involved in allergic reactions.
- Eosinophils have a role in parasitic infestation.
- Basophils of the peripheral blood are also rich in histamine granules; they play a role in allergic reactions.
- Monocytic cells have the property of phagocytosis. They can kill bacteria and remove debris.
- Monocytes produced interferon.
- They have a longer life than neutrophils.
How will you summarize the difference between various granulocytic series (neutrophils) cell types?
| Characteristics | Myeloblast | Promyelocyte | Myelocyte | Metamyelocyte | Band form | Neutrophil |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
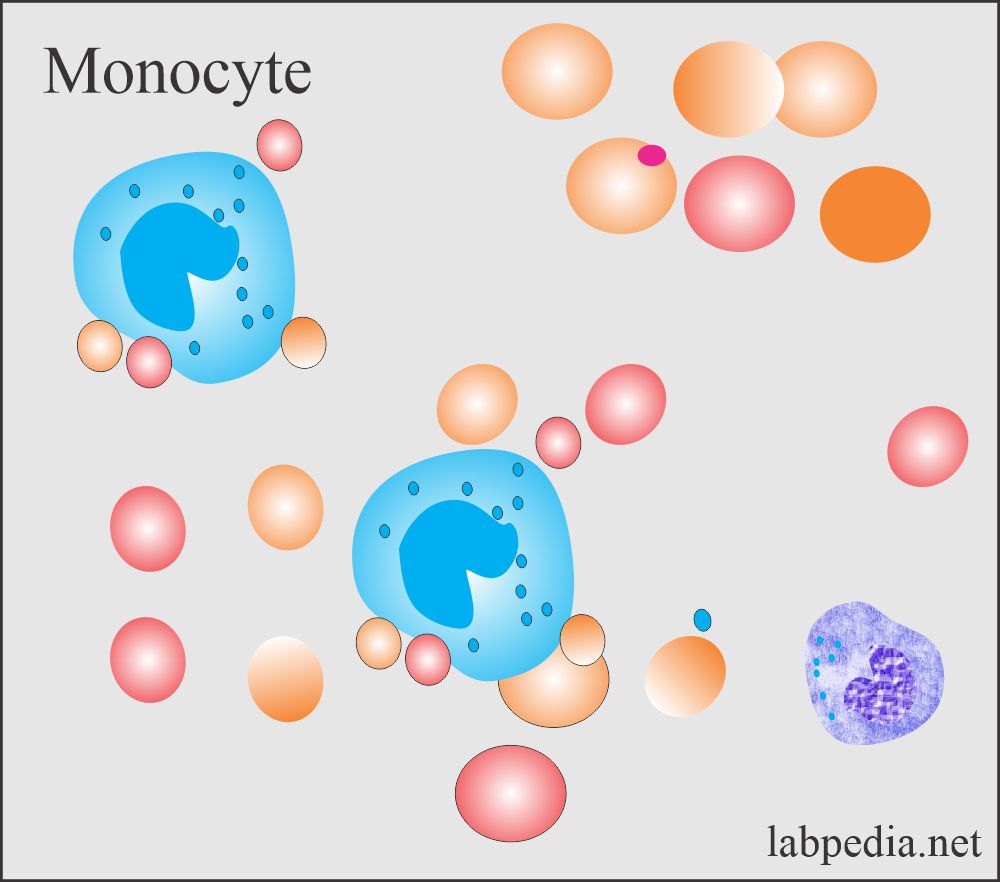
Monocytes:
How will you define monocytes?
- Monocytes develop from the monoblast in the bone marrow.
- These macrophagic cells measure 25 to 80 µm with round or reniform nuclei and contain one or two nucleoli.
- There is clumped chromatin, abundant cytoplasm with vacuoles, and numerous azurophilic granules.
- These monocytes enter the circulation for a short time, then migrate to the tissue and transform into macrophagic cells.
- Monocytes are also called histiocytes, meaning histio = tissue and cyte= = cells.
What are the various forms of monocytes?
- When these monocytes are mature, they become too large to pass readily through the capillaries, so these settle in the tissue and convert into tissue macrophages in many organs like:
- In the lungs, they are called pulmonary alveolar macrophages.
- In the peritoneum are called peritoneal macrophages.
- In the spleen are called splenic macrophages.
- In the liver are called Kupffer’s cells.
- In the connective tissue are called tissue macrophages.
- These are also phagocytic cells.
- Monocytes don’t enter the circulation but can return to circulation in case of inflammation.
- What are the functions of monocytes?
- Their function as phagocytosis is similar to neutrophils.
- Monocytes can produce more rapidly than neutrophils and spend longer than neutrophils.
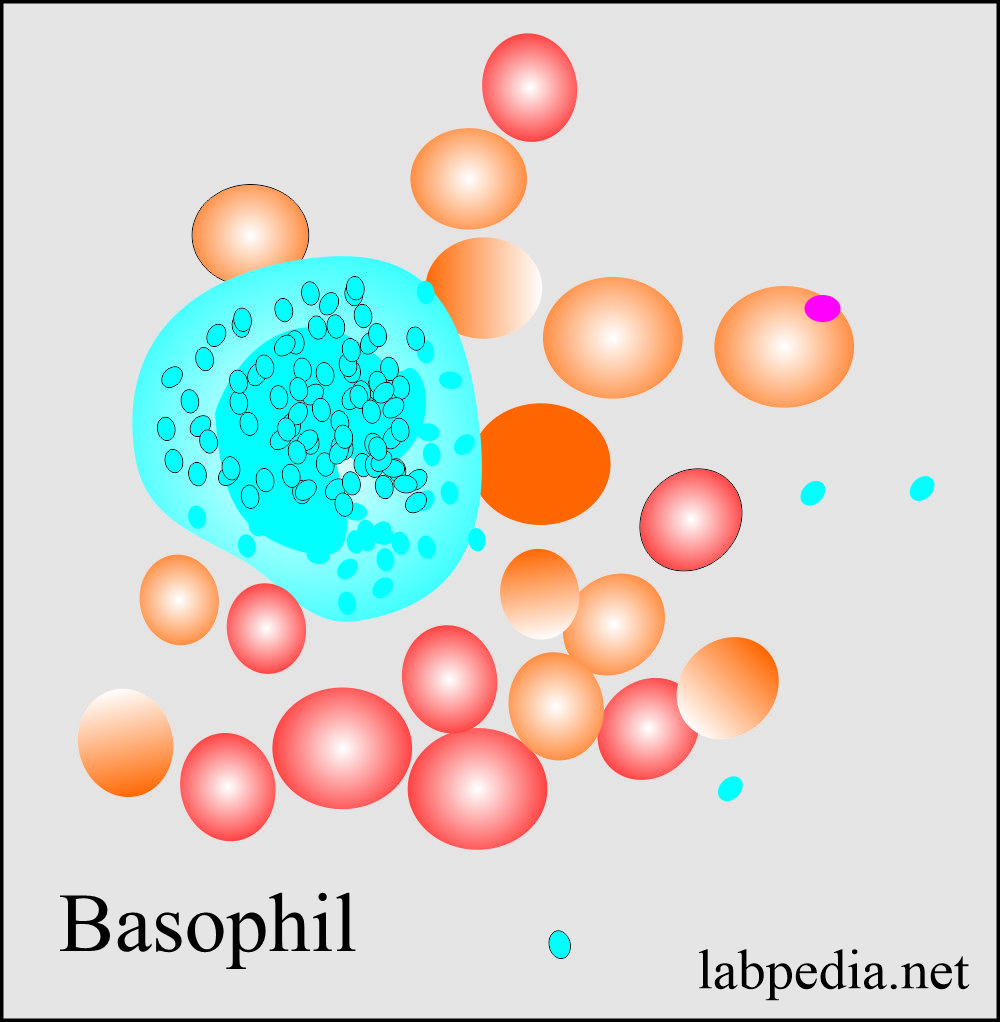
Basophils:
How will you define basophils?
- These cells all pass through the same stages as the neutrophils.
- These are also called mast cells when present in the tissue.
- The cells have large basophilic granules.
- The maturation of the basophils in the bone marrow takes more than 7 days.
- Basophils circulate in the peripheral blood for a few hours, then migrate to the tissue, skin, mucosa, and serosal surfaces.
Eosinophils:
How will you define eosinophils?
- Eosinophils develop 3 to 6 days in the bone marrow before appearing in the peripheral blood.
- These are stored in the bone marrow and released to the peripheral blood circulation when needed.
- The mean time in the circulation is about 8 hours.
- Eosinophils migrate from blood to bronchial mucosa, skin, GI tract, and vagina in about 12 days.
- Eosinophils can migrate back to blood and bone marrow.
- Eosinophils are motile and can migrate between the endothelial cells into tissue or areas of inflammation.
What are the granules of the eosinophils?
- It contains hydrolytic enzymes like:
- Peroxidase.
- Acid phosphatase.
- Aryl sulfatase.
- β-glucuronidase.
- Phospholipase.
- Cathepsin.
- Ribonuclease.
- But eosinophils lack the enzymes like:
- Alkaline phosphatase.
- Lysosomes.
- Cationic proteins.
- There are tissue eosinophils, and these have prominent nucleoli.
Immunocytes:
How will you define lymphocytes?
Lymphocytes are of two types:
- B – lymphocytes give rise to antibody-dependent immunity.
- T – lymphocytes give cell-mediated immunity; their subtypes are:
- T – cytotoxic cell. (T – killer).
- T – suppressor cell.
- T – helper cell.
- T cells’ primary function is to fight chronic bacterial and viral infections.
What is the normal Total leucocyte count?
Source 2
- Adult /child = 5000 to 10,000 /cmm
- Child ≤2 years = 6200 to 17000 /cmm.
- Newborn = 9000 to 30,000 /cmm
Other sources
- Adult and child = 5000 to 10,000/cmm.
- Child under 2 years = 6200 to 17,000/cmm.
- Newborn = 9000 to 30,000/cmm.
What is the differential count of peripheral blood?
| Type of the cells | % | Absolute count |
|
|
|
|
|
|
|
|
|
|
|
|
What are the causes of increased TLC (Leucocytosis)?
- The TLC is >11000/cmm.
- Mostly in the case of infections that may be bacterial or viral.
- Localized infections are:
- Meningitis.
- Pneumonia.
- Abscess.
- Tonsillitis.
- Generalized infections:
- Septicemia.
- Acute rheumatic fever.
- Cholera.
- Localized infections are:
- In the case of leukemias.
- After the strenuous exercise.
- Pain and anorexia.
- Epileptic seizures.
- Emotional reaction.
- Mild leucocytosis in pregnancy.
- Acute hemorrhage.
- Intoxications like:
- Poisoning by drugs, chemicals, and venoms (black widow spider).
- Metabolic diseases include uremia, acidosis, eclampsia, and acute gout.
- Parenteral proteins and vaccines.
- Acute hemolysis of red blood cells.
- Myeloproliferative diseases.
- Tissue necrosis:
- Burns.
- Gangrene.
- Necrosis of the tumor.
- Acute myocardial infarction.
- Necrosis due to bacteria.
- Physiologic conditions are:
- Emotional stress.
- Exercise.
- Obstetrical labor.
- Menstruation.
What are the causes of decreased leucocytosis (neutropenia)?
- The TLC is <4000/cmm.
- This may be seen in fever, malaise, and chills.
- Bacterial Infections:
- Bacterial.
- Septicemia.
- Miliary tuberculosis.
- Typhoid fever.
- Paratyphoid fever.
- Tularemia.
- Brucellosis.
- Viral infections are:
- Hepatitis.
- Influenza.
- Infectious mononucleosis.
- Psittacosis.
- Rubella.
- Measles.
- Hematological diseases:
- Aleukemic leukemia.
- Pernicious anemia.
- Gaucher’s disease.
- Felty’s syndrome.
- Aplastic anemia.
- Deficiency of vitamin B12.
- Drugs and chemicals:
- Antibiotics.
- Analgesics.
- Sulphonamides.
- Antithyroid drugs.
- Arsenicals.
- Marrow depressant.
- Malignant infiltration of the bone marrow.
- Bone marrow aplasia.
- Bone marrow depression by radiations.
- Autoimmune diseases like SLE.
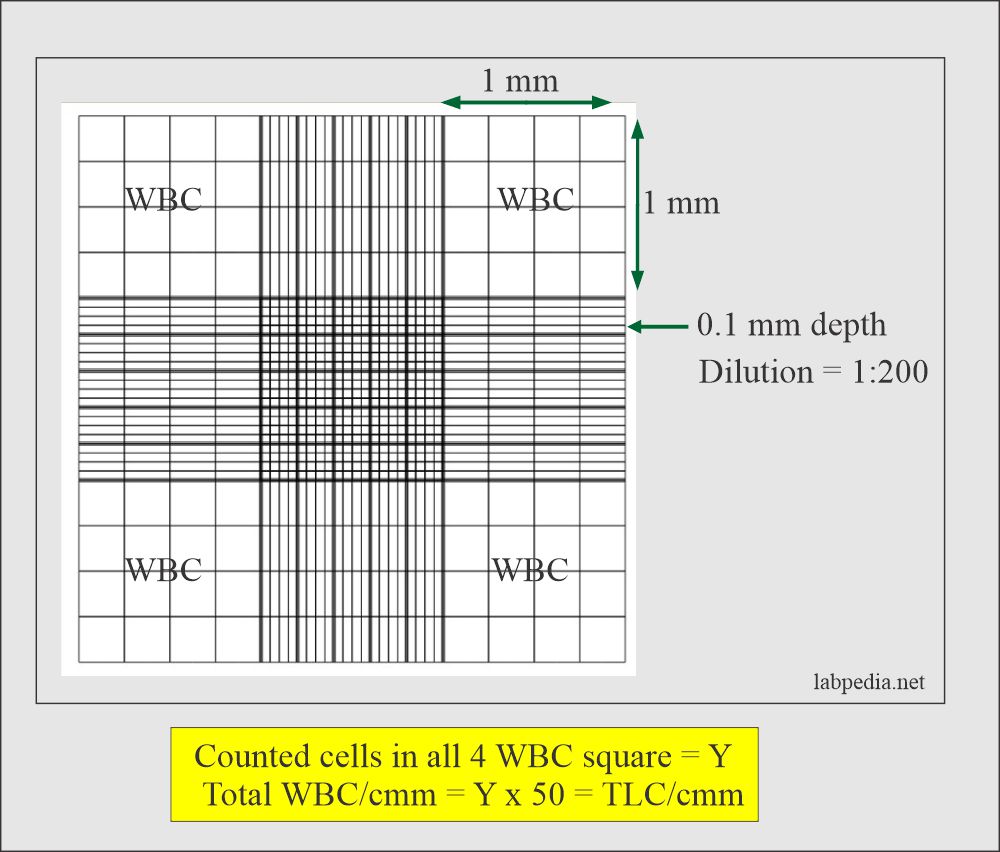
TLC counted in Neubauer chamber:
- Please always correlate TLC with the freshly prepared peripheral blood slide.
- Critical value = <2500 or >30,000 /cmm.
Questions and answers:
Question 1: Is there an effect of exercise on TLC?
Question 2: What is the target organ of IL-3?
- Please see more details in CBC part 1.