Vitamin E (Alpha-Tocopherol)
Vitamin E (alpha-tocopherol)
What sample is needed for Vitamin E (α-Tocopherol)?
- The patient’s plasma is needed. For plasma, take a sample in heparin.
- A fasting sample is preferred.
- The sample is stable at 4 °C for 4 weeks and at -20 or -70 °C for one year.
- Protect from light.
What are the precautions for Vitamin E?
- Avoid the use of alcohol at least 24 hours before taking the blood sample.
- Protect the sample from light.
How will you define Vitamin E?
- Vitamin E is an antioxidant and free radical scavenger, especially in the cell membranes.
- It is a fat-soluble vitamin.
- It protects cells from oxidative stress.
- α-Tocopherol is only used by humans.
What is the history of Vitamin E?
- In 1920, vegetable oil was the factor that caused deficient resorption in deficient rats.
- Later on, the name tocopherol was given.
- Vitamin E has several biologically active isomers.
- The word tocopherol is a Greek-derived name.
- Its fertility role is still questionable.
- α-tocopherol is the most common biologically active isomer in the blood.
How will you discuss the pathophysiology of Vitamin E?
- This is a powerful antioxidant vitamin.
- Oxidants’ role is to cause disease, aging, and cleavage of fatty acids.
- Vitamin E is soluble in fat solvents and insoluble in water.
- Its generic name is tocopherol, and it includes several biologically active isomers.
- α-tocopherol is the predominant isomer and is the biologically active form.
- It is viscous oil at room temperature.
- Stable to heat in the absence of oxygen.
- It plays a role in cellular respiration.
- Vitamin E contains 8 related natural compounds that are biosynthesized in plants and are abundant in vegetables.
- Eight Vitamin E subtypes are tocopherols and tocotrienols.
- Its most active unit is α-tocopherol.
- Its main function is antioxidants.
What are the isomers of Vitamin E?
- α-Tocopherol (Alpha-Tocopherol).
- β-Tocopherol (Beta-Tocopherol).
- γ-Tocopherol (Gamma-Tocopherol).
- δ-Tocopherol (Delta-Tocopherol).
- ζ-Tocopherol (Zeta-Tocopherol).
- ε-Tocopherol (Epsilon-Tocopherol).
- η-Tocopherol (Eta-Tocopherol).
- 8-Methyl-tocotrienol.
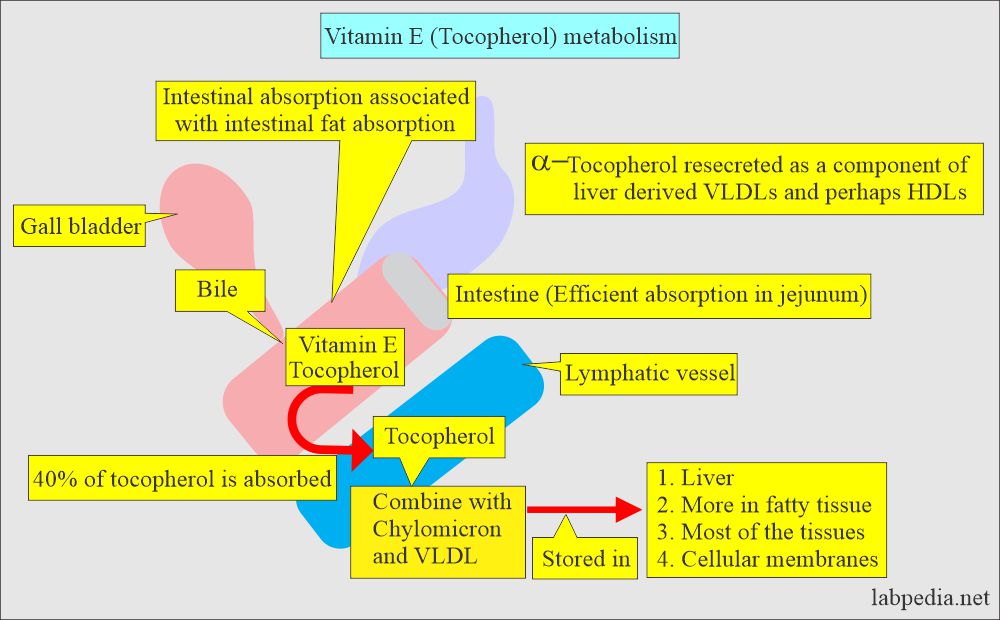
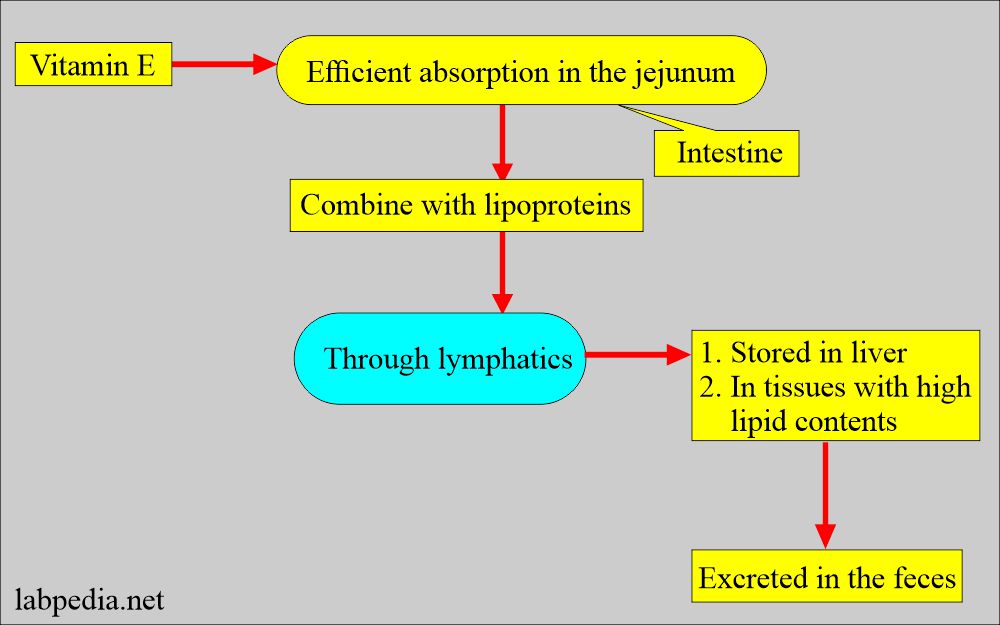
What is the mechanism of the absorption of vitamin E?
- Its absorption takes place in the presence of bile in the small intestine.
- Most of the tocopherol enters the bloodstream via lymph.
- So, it is associated with chylomicron and very low-density lipoprotein.
- About 40% of the ingested tocopherol is absorbed.
- The physiological requirements of vitamin E (Tocopherol) increase with increasing polyunsaturated fatty acids in the diet.
- Absorbed vitamin E (tocopherol) is first associated with circulating chylomicron and VLDL.
- Some vitamin E (Tocopherol) is transferred to adipose tissue during triglyceride hydrolysis.
What are the sources of vitamin E?
- Vegetable oils.
- Fresh leafy vegetables.
- Eggs and yolk.
- Legumes.
- Peanuts and seeds.
- Margarine.
- Most of it is stored in the adipose tissue.
What is the metabolism of Vitamin E?
- Vitamin E (Tocopherol) absorption, transportation, and storage are partially understood.
- Vitamin E (Tocopherol) is absorbed along with chylomicron and VLDL.
- Bile salt is needed for its absorption.
- When the normal dose of Vitamin E is given, a very small amount appears in the urine.
What are the functions of Vitamin E?
- Vitamin E (tocopherol) is an Antioxidant.
- The specific role of humans is unclear.
- It protects unsaturated fatty acids from peroxidation (it is the cleavage of fatty acids).
- Cleavage of fatty acids at their unsaturated sites by oxygen addition across the double bond and formation of free radicals.
- Protect from free radicals.
- Prevent the oxidation of the cell membrane’s vitamin A, DNA, and phospholipids.
- Acts with selenium for the maintenance of cell membranes. This effect may be more neuronal.
- Vitamin E plays a role in protecting the RBC membranes from oxidant stress.
- There is evidence to prevent retrolental fibroplasia, intraventricular hemorrhage, and mortality of premature infants.
- Vitamin E may have a preventive role in cardiovascular disease.
- Vitamin E also plays a role in neurological diseases.
- It maintains healthy skin by preventing oxidative stress.
What is the presentation of Vitamin E deficiency?
- There is irritability and edema.
- There is peripheral neuropathy and ataxia.
- There is a degeneration of the spinal cord.
- Vitamin E protects the RBC’s cell membrane from oxidants.
- The anemia is due to the fragile RBC membrane, and there is no response to iron therapy.
- Mild Hemolytic anemia in infants.
- These symptoms due to its deficiency are rare except for malabsorption.
- There is a loss of tendon reflexes.
- There may be pigmentary retinopathy.
What are the signs and symptoms of vitamin E deficiency?
- The major symptom is mild hemolytic anemia.
- A relationship exists between vitamin E deficiency and progressive loss of neurological function in infants and children with chronic cholestasis.
- Premature infants are supplemented with vitamin E to stabilize the RBC membranes and prevent hemolytic anemia.
- It has been found that there is a relationship between vitamin E deficiency and the progressive loss of neurological signs in infants and children with chronic cholestasis.
- The nervous system is very sensitive to vitamin E deficiency.
- Some signs of Vitamin E deficiency include axonal deterioration in the spinal cord, which is associated with gait disturbance and stability.
- Sterility is found in animal models.
- There is macrocytic megaloblastic anemia in α-Tocopherol deficiency.
- How will you diagnose vitamin E deficiency?
- α-Tocopherol concentration is <5 mg/L.
What are the signs and symptoms of Vitamin E toxicity?
- There is decreased platelet aggregation.
- There may be impaired wound healing.
- There is impaired fibrinolysis.
- There may be hepatomegaly.
- There is creatinuria.
- How will you Diagnose vitamin E toxicity?
- Infants receiving sufficient amounts of α-Tocopherol where serum level is >30 mg/L have an increased incidence of sepsis and necrotizing enterocolitis.
- The patients receiving a synthetic diet should be monitored to avoid Vitamin E toxicity.
What is the normal Vitamin E?
Source 1
- Some recommend > 0.5 mg / 100 ml.
- Premature neonates = 0.31 to ± 0.06 mg/dL.
- 1 to 12 years = 0.3 to 0.9 mg/dL
- 13 to 19 years = 0.6 to 1.0 mg/dL
- Adult = 0.5 to 1.8 mg/dL
- Deficiency = <0.3 mg/dL
- Excess level = >4 mg/dL
Another source
- Recommended daily dose for adult males = 10 mg/day.
- For females = 8 mg/day.
Questions and answers:
Question 1: What is the main complication of vitamin E deficiency?
Question 2: What is the main role of Vitamin E?