Vitamin D (Vitamin D2 and D3)
Vitamin D (Vitamin D2 and D3)
What sample is needed for the estimation of Vitamin D?
- Venous blood is needed to prepare the serum.
- A random sample can be used.
- The sample is stable at room temperature for 72 hours.
- The sample is stable at 22 to 25 °C.
What are the Indications for Vitamin D?
- Indicated in postmenopausal women to evaluate Vitamin D levels needed for Calcium absorption.
- To evaluate the role of Vitamin D in osteoporosis.
- To find the role of Vitamin D in the prevention of cancer.
What is the history of Vitamin D?
- In 1822, it was found that rickets could be prevented by cod liver oil.
- Rickets where there were muscle hypotonia and skeletal deformities.
- After 100 years, the antirachitic factor in cod liver oil was found to be vitamin D.
- These antirachitic factors are collectively called vitamin D.
- In 1925, it led to eliminating the widespread disease of nutritional rickets.
- Vitamin D is now considered to be a hormone.
How will you define Vitamin D?
- These are a group of fat-soluble vitamins that affect calcium and phosphorus metabolism.
- There is the effect of UV radiation on this vitamin.
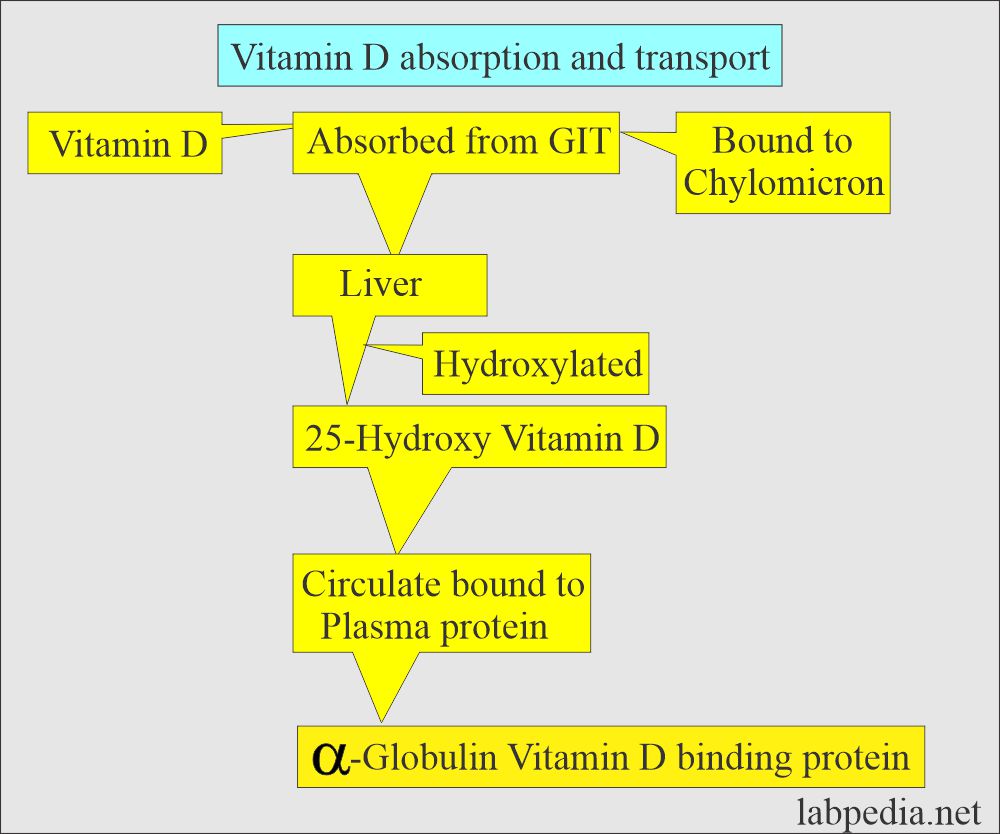
- Cholecalciferol (D3) in the liver is hydroxylated to 25-hydroxycholecalciferol.
- In the kidneys, they are hydroxylated to dihydroxy metabolites.
- PTH increases the production of 1,25,(OH)2 D3 in renal proximal tubules and causes increased intestinal calcium absorption.
How will you discuss the pathophysiology of Vitamin D?
- Vitamin D is a fat-soluble vitamin, and it is a hormone-like steroid.
- The naturally occurring fish liver oil is vitamin cholecalciferol (Vitamin D3).
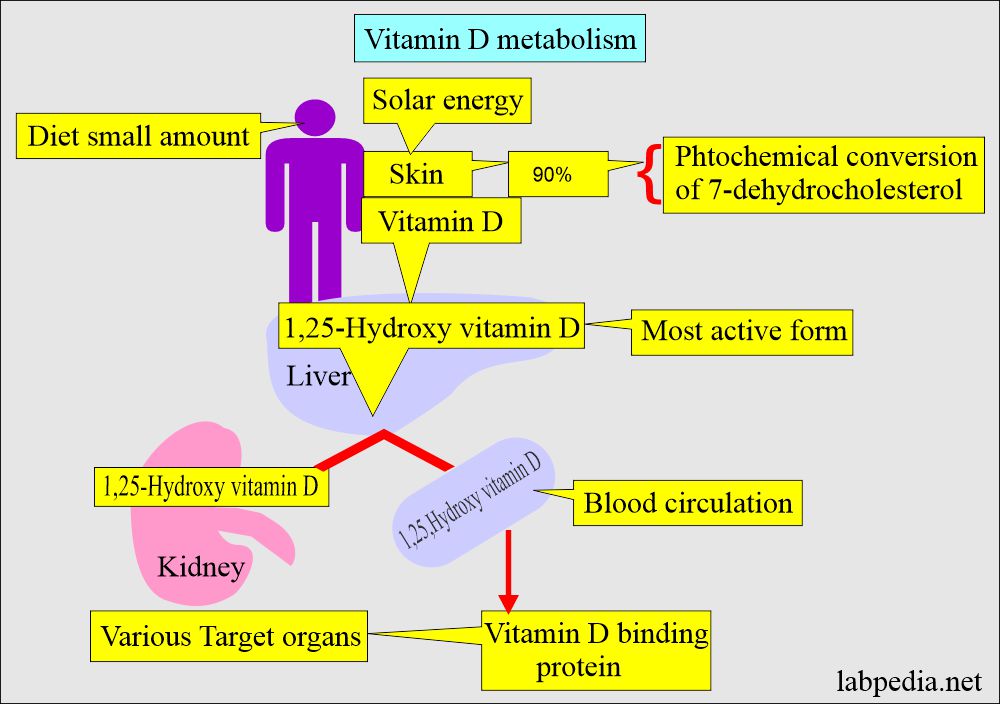
- It is produced in the skin from ultraviolet activation of 7-dehydrocholesterol.
- 7-hydrocholesterol in the skin is produced by sunlight (ultraviolet rays) and converted into D2 and D3.
- Vitamin D is found in two forms:
- Vitamin D2 (Ergocalciferol). It is a plant-derived vitamin.
- Vitamin D3 (Cholecalciferol).
What is the difference between Vitamin D2 and D3?
| Differentiating points | Vitamin D2 (Ergocalciferol) | Vitamin D3 (Cholecalciferol) |
|
It is plant-based like:
|
It is animal based like:
|
|
It is derived from:
|
It is formed:
|
|
|
|
|
It is more sensitive to:
|
It is more:
|
|
|
|
|
|
|
What are the main sites of vitamin D action?
- The target organs of the vitamin D action are:
- Intestine.
- Kidneys.
- Bones.
- Vitamin D (Calcitriol) facilitates calcium and phosphorus absorption from the intestine.
- It induces a specific calcium-binding protein in the intestine.
- Vitamin D (Calcitriol) works with PTH to increase bone resorption by increasing osteoclastic activity.
- Vitamin D (Calcitriol) increases the renal reabsorption of calcium and phosphorus.
- 99% of the filtered calcium is reabsorbed.
- 1, 25-hydroxy vitamin D administration increases the vitamin D receptor mRNA concentration in the parathyroid gland.
What is the mechanism of absorption of Vitamin D3?
- In the diet, vitamin D is in two forms:
- Cholecalciferol (D3)
- Ergocalciferol (Vitamin D2).
- 1. 25, (OH)2 D3 stimulates the intestinal absorption of Ca++ and PO//.
- Bile salts are needed for its absorption.
- It is stored in the liver and excreted in the bile.
- Under the influence of the PTH, it helps for:
- Bone growth.
- Metabolism.
What are the Vitam D sources?
- Diet is not the major source of vitamin D; the main source is skin exposure to sunlight.
- Major dietary sources include irradiated foods and commercially prepared milk.
- A dietary source of fish that is rich in Vitamin D.
- The artificial sources are milk, breakfast cereals, and supplements.
- Small amount occurs in butter, egg yolk, liver, salmon, sardines, and tuna.
- Vitamin D2 is derived from plant sterols.
- Vitamin D3 is provided by animals or of synthetic origin.
- In normal adults, endogenous photosynthesis in the skin provides 90% of vitamin D, which may amount to 1.5 to 10 mg/day.
What are the Vitamin D3 sources?
- Animal food.
- Fatty fish.
- Eggs.
- Liver.
- Butter.
- Vitamin D3 is produced in the skin under the influence of sunlight.
- There is a special effect of ultraviolet light (ultraviolet B radiation).
- 7-dehydrocholesterol under the influence of ultraviolet-B light converted into vitamin D3.
- The wavelength of ultraviolet light is 270 to 300.
- These lights are present at sea level and not seen in the Arctic Circle.
- Exposure to the sun for 10 to 15 minutes a week forms an adequate amount of vitamin D3.
- Don’t use sunblock.
- Vitamin D formation depends upon the melanin contents. People with more melanin need more time.
- Vitamin D from the skin or from food is converted into 1,25-dihydroxyvitamin D in the liver and kidneys.
- 1,25, dihydroxy vitamin D is a hormonally active form of vitamin D and is released into circulation.
- It binds to a carrier protein (vitamin-D binding protein = VDBP) and reaches various target organs.
- Vitamin D receptors (VDR) are present in the nucleus.
- The binding of vitamin D3 to VDR of target cells now acts as a transcription factor.
- This will ultimately lead to the absorption of Calcium in the intestine.
- Activation of VDR in the intestine, bone, kidney, and parathyroid glands maintains calcium and phosphorus in the blood.
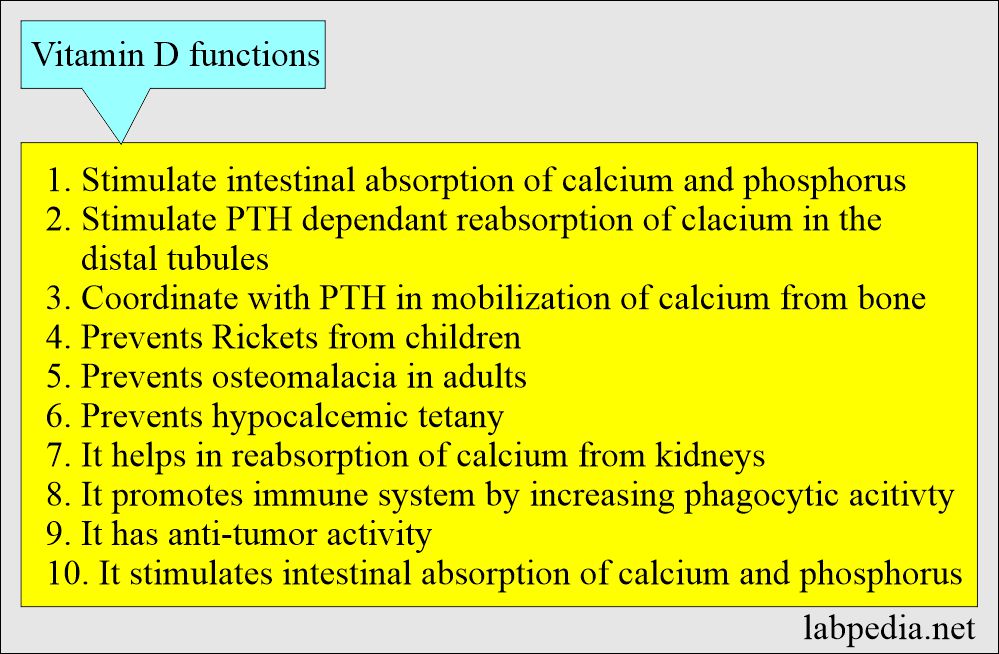
What are the functions of vitamin D?
- Vitamin D’s major role is to regulate serum calcium and phosphorus in the blood by:
- Promoting their absorption of food in the intestine.
- By promoting the reabsorption of calcium in the kidneys.
- This will prevent Rickets from growing children.
- Prevents osteomalacia in adults.
- Prevents hypocalcemic tetany.
- Vitamin D corrects and maintains the concentration of ionized calcium.
- Vit. D inhibits parathyroid hormone secretion from the parathyroid gland.
- Vitamin D promotes:
- The immune system increases phagocytosis.
- Anti-tumor activity.
- Immunomodulatory function.
- Role in calcium absorption:
- It stimulates intestinal absorption of calcium and phosphorus.
- It stimulates the PTH-dependent reabsorption of calcium in the distal renal tubule.
- It helps PTH to mobilize the calcium from the bone.
- PTH, vitamin D, and calcitonin maintain normal Ca++ in bone and plasma.
What is the outcome of a deficiency of vitamin D?
- Rickets in the children in the growing age.
- Osteomalacia in adults.
- Prolonged deficiency causes osteopenia.
- Hypocalcemia.
What is the toxicity of vitamin D?
- Overdosage of vitamin D leads to metastatic calcification of soft tissues.
- Hypervitaminosis of vitamin D (calcitriol) leads to hypercalcemia.
- An increased vitamin D level increases intestinal absorption and causes excessive bone resorption.
- Increased vitamin D leads to increased calcium and suppresses the PTH.
What are the causes of Vitamin D deficiency?
- Inadequate dietary intake.
- Inadequate sunlight exposure.
- Malabsorption syndrome.
- Liver or kidney disorders.
- Metabolic hereditary disorders.
- Vitamin D deficiency leads to (Bone-softening diseases like):
- Rickets in children.
- Osteomalacia in adults.
- Osteoporosis.
- Recent evidence is that deficiency may be associated with cancers of the colon, breast, and pancreas.
- This may be associated with increased blood pressure and cardiovascular disease risk.
What group of people are at risk of Vitamin D deficiency?
- Infants on breastfeeding (human milk is deficient in Vit. D).
- Occupation is when people are not exposed to the sun.
- Individuals with a body mass index (BMI) >30 are too fatty because Vitamin D is trapped in fatty tissues.
- Malabsorption from GIT.
- Patient with liver or kidney diseases.
How will you measure Vitamin D?
- Measure 25-hydroxy D2 and D3 = Total Vit D.
- Treatment is based on the total Vit.D level.
What is the normal Total Vitamin D?
Source 1
- 16 to 65 pg/mL
- Maternal concentration is 2-fold higher.
Another source
- 25-hydroxy vitamin D = 30 to 100 ng/mL
Other sources
- Indicate vitamin D deficiency = <20 ng/mL
- Insufficiency of vitamin D = 20 to 30 ng/mL
- Optimal level of vitamin D = >30 ng/mL
- Toxic level of vitamin D = >200 ng/mL
- The recommended dose of vitamin D for adults is 5 µg/day.
What are the causes of increased levels of Vitamin D?
- Excessive dietary supplement.
- William syndrome. This is a rare genetic disorder.
What are the causes of decreased levels of Vitamin D?
- Rickets.
- Osteoporosis.
- Liver diseases.
- Renal diseases.
- Inadequate dietary intake.
- Inadequate exposure to sunlight.
- Acute inflammatory diseases.
- Familial hypophosphatemic rickets.
Questions and answers:
Question 1: Which form of vitamin D is biologically active?
Question 2: What is the cause of rickets?