Urine History, Composition, Normal Findings
Urine History, Composition, Normal Findings
Urine History
What is the history of the urine examination?
- Ancient Egyptian physicians used to taste the urine to find the disease.
- Indian physicians started using urine to diagnose diseases in almost 2000 BC.
- Greek physician Hippocrates also recognized the value of urine examination.
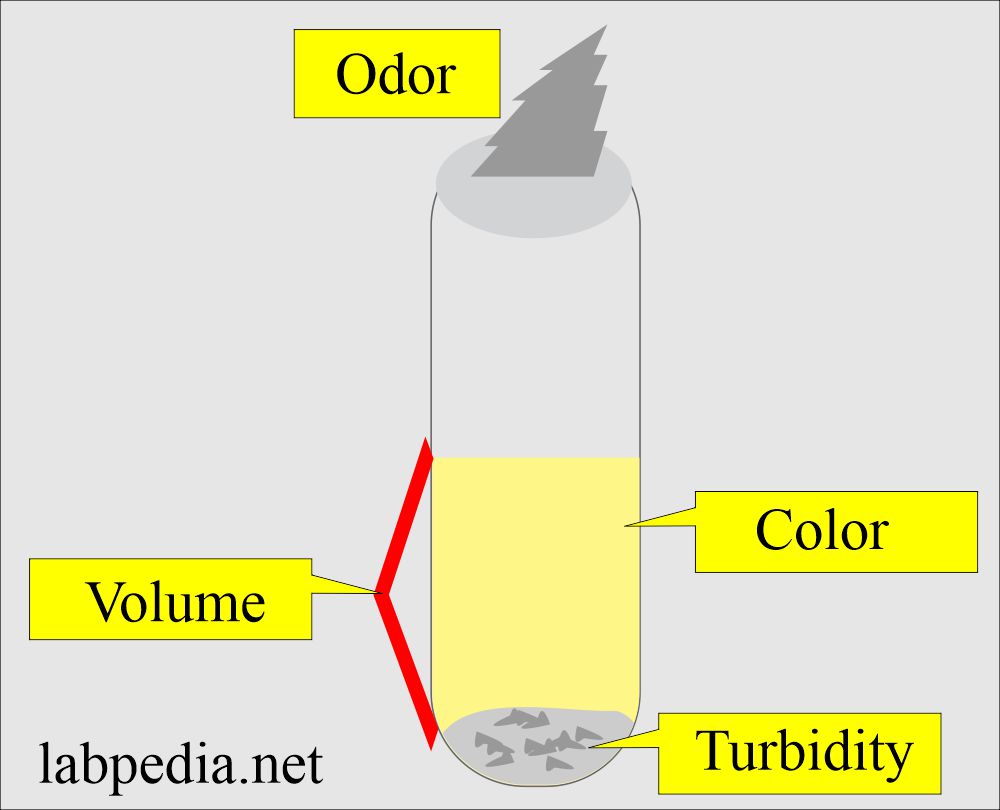
- He noted that the color, odor, and even taste of the urine helped in the diagnosis.
- Then, in the Middle Ages, urine examination also became important.
- They started measuring the specific gravity with a urinometer.
- With the invention of the microscope in the 19th century, urine examination started helping diagnose various diseases, such as hematuria and bacterial infection.
- In the modern era, urine examinations diagnose diabetes mellitus, proteinuria, and ketone bodies.
- The analysis of the urine is the beginning of laboratory medicines.
- The physicians then checked the urine’s gross appearance, like color, turbidity, odor, volume, and urinary infection.
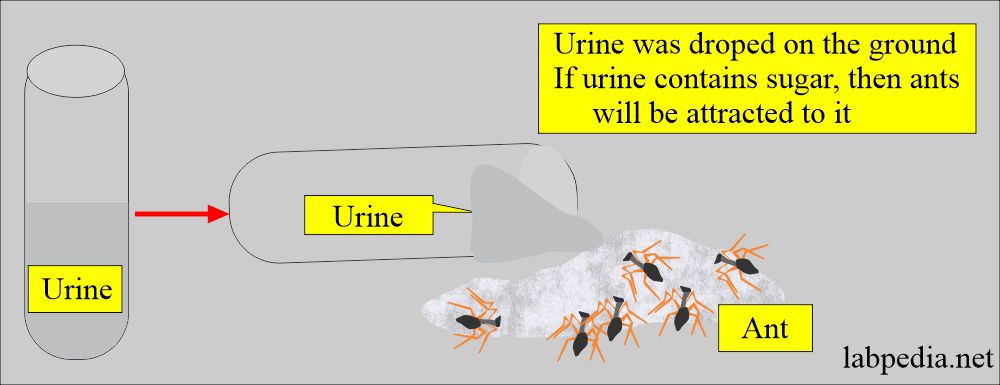
- They tested the viscosity and even the sweetness. For sweetness, they observed the ants’ attraction to urine.
- Hippocrates wrote a book on urine examination as uroscopy in 5th BC.
- In 1140 AD, color characteristics were developed, describing the significance of 20 different urine colors.
- Chemical testing progressed after the ant gathered around the diabetic urine.
- Later on, taste testing was also started.
- In 1694, Frederick Dekkers discovered the protein Albuminuria by boiling the urine.
- Pisse prophets by the Charlatans became the subject of the book published by Thomas Bryant in 1627.
- The advent of the microscope in the 17th century led to the examination of urine sediments.
- Richard Bright, in 1827, made the urine examination a routine for the patients.
- In 1930, the number and complexity of urine examinations made them impractical.
- With modern facilities, the urine examination is a routine part of the patient’s doctor’s office visit.
What is the modern urine examination?
- Now, a urine examination is popular due to the following:
- Easily available sample.
- Urine gives much of the body’s metabolism information.
- This information from the urine is cheap.
- The National Committee for Clinical Laboratory Standards (NCCLS) defines urine analysis as reliable, accurate, safe, and cost-effective.
How will you define Urine?
- Urine is a liquid biopsy obtained without pain or cost to the patient, but it provides a wealth of diagnostic information.
- Urine is the main source of information from sick (damaged) kidneys to physicians.
- Urine is the fluid excreted through the kidneys, passes through the ureter, and is stored in the urinary bladder. When the urinary bladder is full, it is discharged through the urethra.
How would you describe urine in a healthy person?
- Sterile.
- Clear.
- Amber color.
- It is slightly acidic (pH 5 to 6).
- Specific gravity is 1.024
- It has a characteristic odor.
- The daily output is 500 mL.
- Anuria:
- It occurs when the urine volume is <100 mL/24 hours.
- Oliguria:
- When the urine volume is <400 mL/24 hours.
- Polyuria:
- When the urine volume is >2000 mL/24 hours.
What is the main purpose of the urine?
- The main purpose of urine is:
- It removes the body’s waste products.
- It controls the blood volume.
- It regulates the blood pressure.
- It keeps the blood chemistry in the normal range.
What is the composition of the urine?
- Ultrafiltrate:
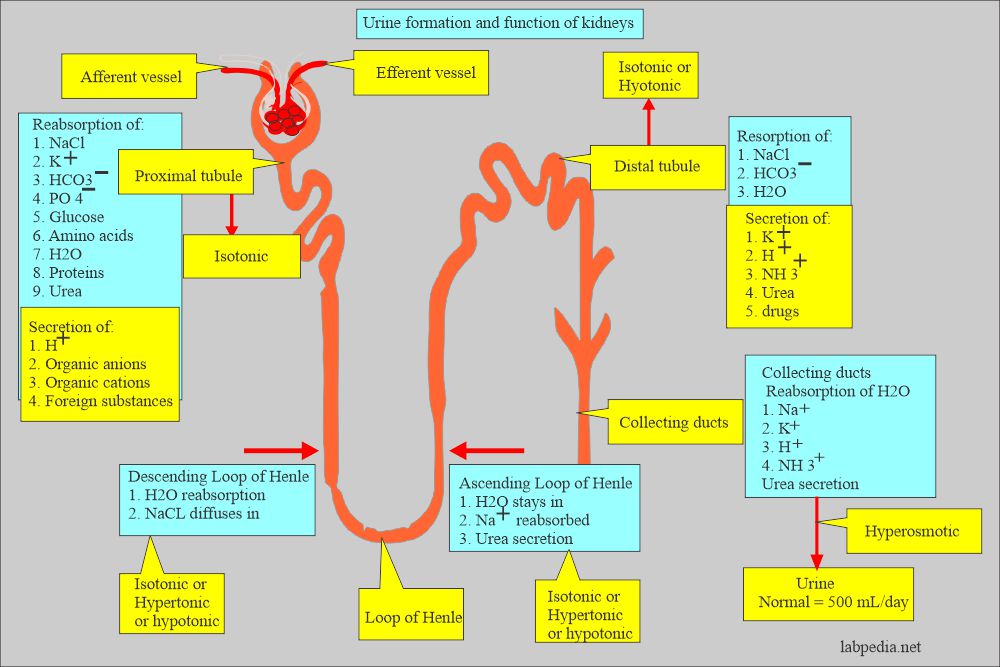
- The kidneys continuously form urine as an ultrafiltrate of plasma. Reabsorption of water and filtered substances is essential to the body’s function, converting roughly 170,000 mL of filtered plasma to the average daily urine output of 1200 mL.
- Urea:
- It is produced in the liver by breaking down proteins and amino acids.
- This is 50% of the dissolved solid substances in the urine.
- Organic substances like creatinine and uric acid.
- Inorganic substances:
- The major substance is chloride (CL¯), followed by Na+ and K+.
- The dietary intake makes it difficult to decide on the normal level.
- Water.
- Other substances found are:
- Hormones.
- Drugs.
- Vitamins.
- Cells.
- Cast.
- Crystals
- Bacteria.
What are the factors needed for urine formation?
- Physical activity.
- Dietary intake.
- Body metabolism.
- Endocrine functions.
How can you confirm the urine sample?
- Advise urea and creatinine; these are present in higher concentrations than any other body fluids and confirm that the specimen is urine.
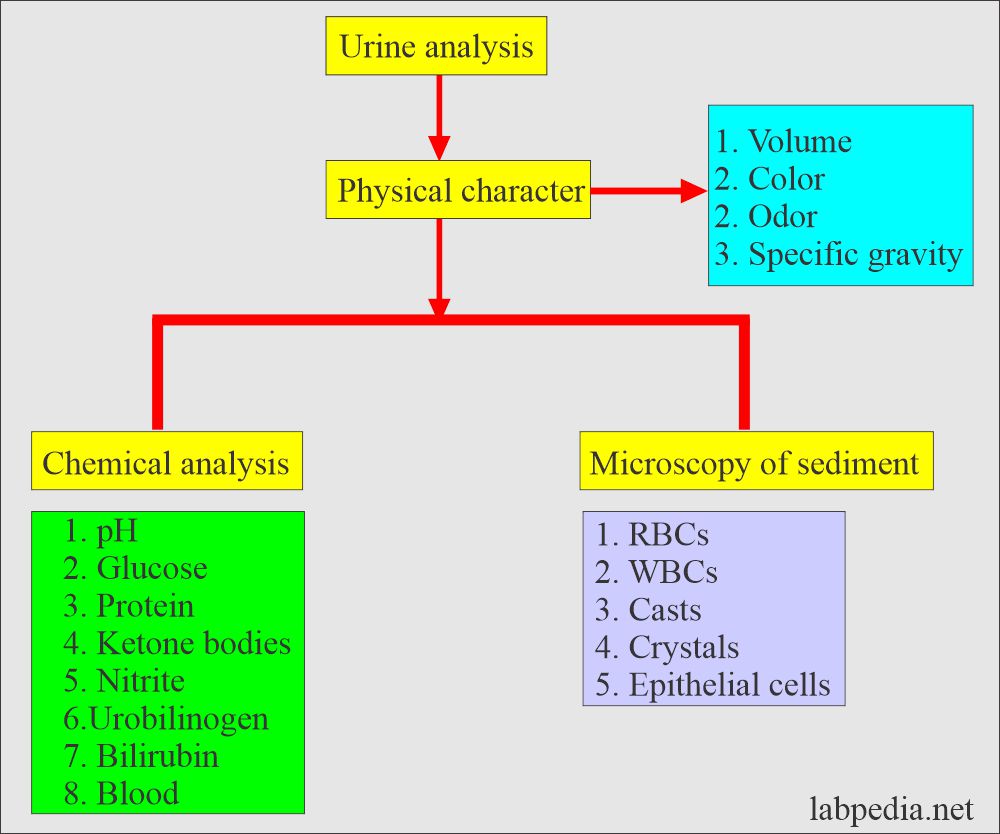
What are the contents of Urine analysis?
Physical properties include:
- Water (95%).
- Color
- Appearance (opaque or colorless)
- Odor
Chemical Tests include:
- pH
- Specific gravity
- Protein
- Glucose
- Ketones
- Bilirubin
- Urobilinogen
- Blood
- Nitrite
- Leukocyte esterase
Microscopic Examination includes:
- Red blood cells
- White cells (WBC)
- Casts
- Crystals
- Epithelial cells
- Bacteria and other microorganisms
What are the normal findings of urine?
| Characteristic | Normal |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1.3 to 7.0 mg/24 hours |
|
|
|
|
|
|
What are the advantages of routine urine analysis?
| Parameter | Advantages of the test |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: What was a test of ants on urine?
Question 2: How can you confirm that the sample is urine?
- Please see the details in Urine Analysis Part 2.