Urine Formation, Types of Urine, and Urine Preservatives
Urine formation
How will you define Urine?
- kidneys filter large amounts of plasma and reabsorb most of it, which is filtered and leaves behind the unwanted metabolic waste to be eliminated is called urine
- The kidneys form urine, passes through the ureters, and is stored in the urinary bladder.
- Normal urine specific gravity is around 1.024, and the color is clear.
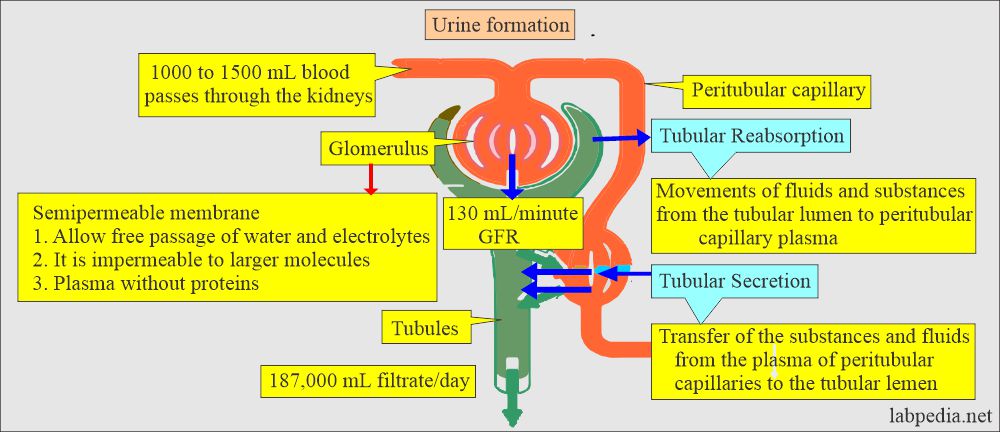
How does urine formation take place?
- Urine formation takes place in three steps:
- Ultrafiltrate formation from the glomeruli from the plasma.
- Reabsorption of the water and solutes from the ultrafiltrate.
- Secretion of the extra solutes into the tubular fluid, like urine.
What is the function of kidneys in urine formation?
- Urine formation.
- Protein conservation.
- Regulation of acid-base balance.
- Regulation of fluid and electrolyte balance.
- Hormonal function.
- Removal of potentially toxic material is one of the main functions of the kidneys.
What is the role of nephrons in urine formation?
- Ultrafiltration is a protein-free plasma filtrate.
- Maintain the body fluid volume.
- Maintain the balance of the composition of the electrolytes.
- Maintain the pH.
What is the role of tubular reabsorption process in urine formation?
- This is the movement of fluids and substances from the tubular lumen to the peritubular capillary plasma.
Tubular Reabsorption:Mode of transport Substances Site of reabsorption - Active transport
- Sodium (Na)
- Proximal and distal convoluted tubule
- Chloride (Cl–)
- The ascending loop of Henle
- Glucose, salts, and amino acids
- Proximal convoluted tubule
- Passive transport
- Urea
- Proximal convoluted tubule
- The ascending loop of Henle
- Sodium (Na+)
- The ascending loop of Henle
- Water (H2O)
- Proximal convoluted tubule
- Descending loop of Henle
- Collecting tubules.
What is the tubular secretion process in urine formation?
- This is the transfer of substances and fluids from the plasma of the peritubular capillaries to the tubular lumen.
Tubular secretion process in urine formation:
| Substances | Site of secretion |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Chemical substances and their excretion and absorption in the renal system:
| Chemical substance | After filtration | Reabsorption g/24 hours | Excreted g/24 hours |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- Each day, an average of 115 to 180 L for females and 130 to 200 L of fluids for men were filtered through the glomeruli.
- Water 180 L is filtered, 178.2 L is reabsorbed, and only 1.5 L is excreted daily.
- Sodium 25,200 meq/day is filtered, 25050 is reabsorbed, and only 150 meq is excreted daily.
- Potassium 720 meq/day is filtered, 620 is reabsorbed, and only 100 meq is filtered per day.
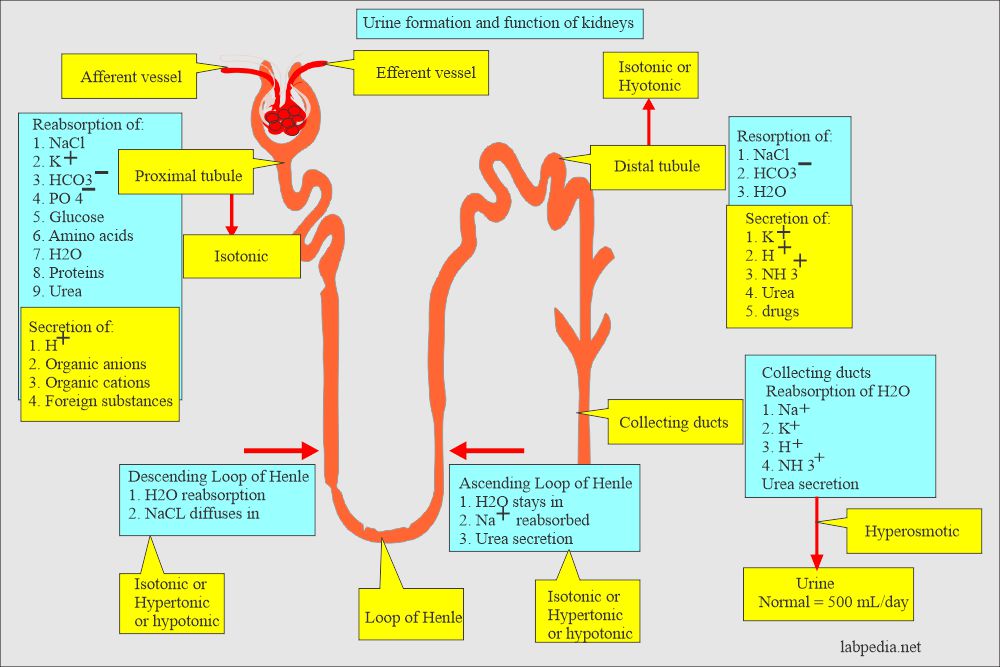
How will you summarize urine formation and functions of the kidney?
- The process of absorption needs metabolic energy to do active reabsorption.
- This process is against the gradient, so it needs energy.
- The kidneys regulate the active reabsorption of glucose, amino acids, low-molecular-weight protein, sodium, calcium, magnesium, potassium, uric acid, chloride, and bicarbonate according to the level of these substances in the blood and the body’s needs.
- Passive reabsorption occurs when substances move by simple diffusion due to an electrical or chemical concentration gradient.
- No cellular energy is involved in this process.
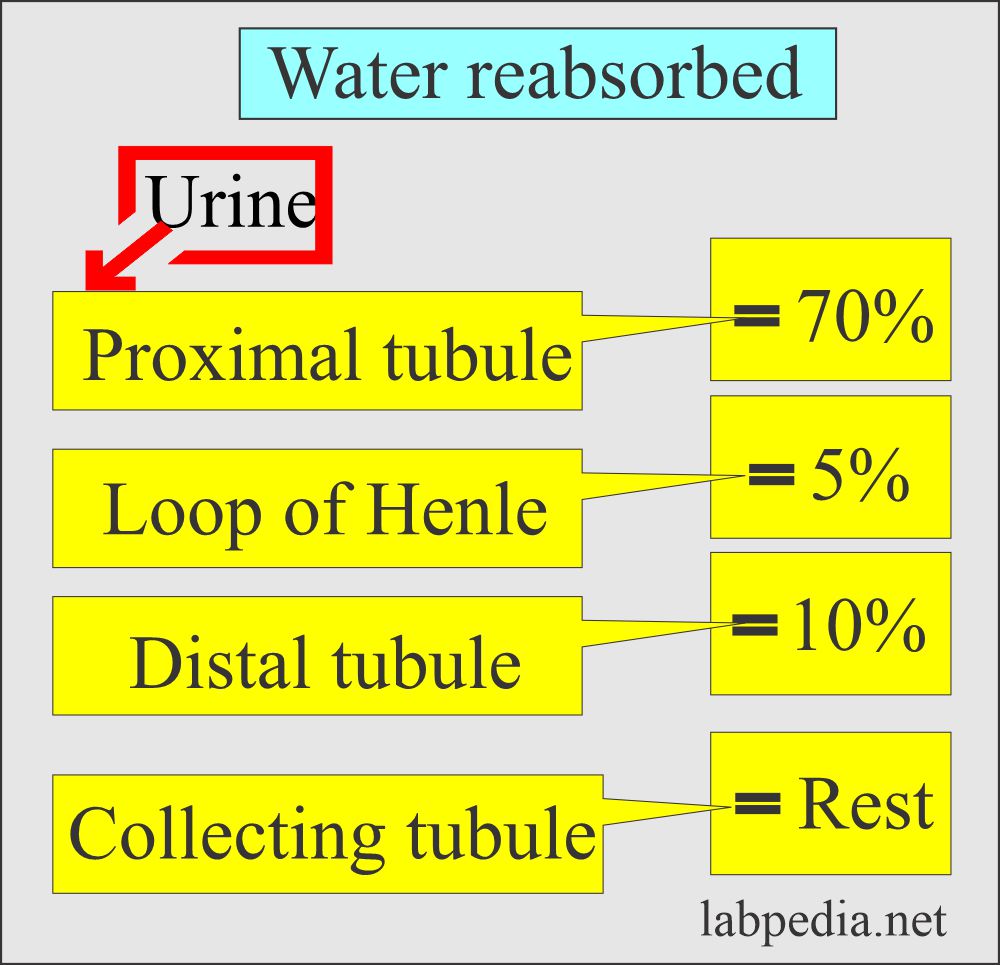
What is the role of the proximal tubules in urine formation?
- Proximal tubular cells perform various physiologic functions for the formation of urine.
- About 80% of salts and water are reabsorbed from the glomerular filtrate in the proximal tubules.
- All glucose and amino acids are reabsorbed.
- The plasma glucose level is completely reabsorbed and does not appear in the urine.
- The higher the plasma concentration of the glucose, the greater the quantity of glucose excreted in the urine.
- Unless it crosses renal thresholds.
- Low-molecular-weight substances are reabsorbed to some extent like:
- Protein.
- Urea.
- Uric acid.
- Chloride, bicarbonate, phosphate.
- K+, Ca++, Mg++.
- Secreted into a tubular fluid by the tubular cells are:
- Organic acids.
- Bases.
- H+ ions.
- Ammonia (NH3).
What is the role of Tubular Secretion in urine formation?
- There is the transport of the substances into the tubular lumen.
- This process is opposite to tubular reabsorption.
- This may be an active or passive process.
- Substances that are transported from blood to the tubules and excreted in the urine include potassium (K+), ammonia, uric acid, certain drugs (penicillin), and hydrogen ions (H+).
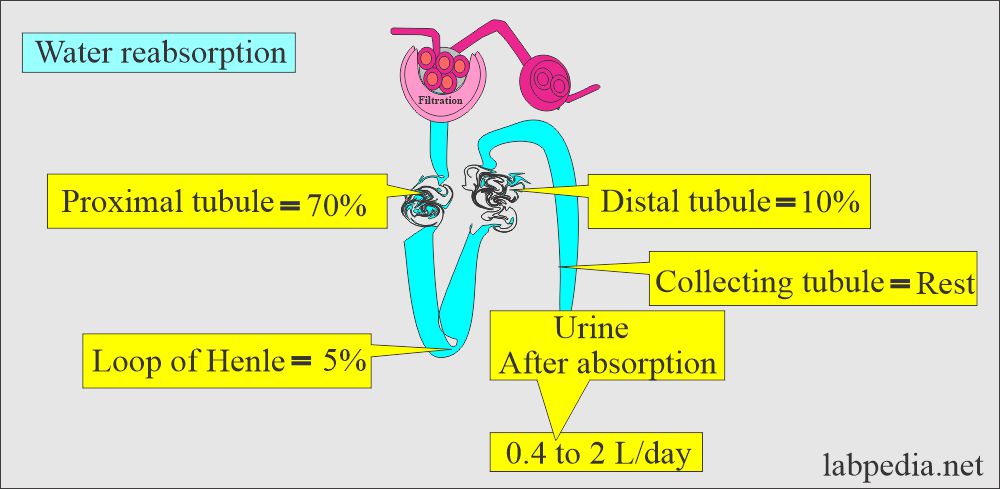
What is the role of Loop of Henle in urine formation?
- The descending loop of Henle is highly permeable to water.
- The loop of Henle is increasingly hypertonic.
- Urine is highly concentrated at the bottom of the loop.
- The ascending limb is relatively impermeable to the passage of the water but actively absorbs sodium (Na+) and chloride (Cl–).
- The ascending limb of the loop of Henle transfers sodium chloride (Na+Cl–) actively from its limen into the interstitial fluid.
- The tubular fluid in the lumen is hypotonic, and interstitial fluid becomes hypertonic.
What is the role of Distal convoluted tubule in urine formation?
- A small fraction of the filtered sodium (Na+), Chloride (Cl+), and water are reabsorbed in the distal convoluted tubule.
- The distal convoluted tubule responds to ADH (anti-diuretic hormone).
- Distal convoluted tubule permeability for water increases in the presence of ADH. It will be low in the absence of the ADH hormone.
- Potassium (K+) is reabsorbed or secreted in the distal tubule.
- Aldosterone stimulates sodium (Na+) reabsorption and potassium (K+) secretion in the distal tubule.
- Hydrogen (H+), ammonia, and uric acid secretion occur in the tubule. At the same time, bicarbonate is reabsorbed in the tubule.
What is the role of collecting ducts in urine formation?
- ADH (anti-diuretic hormone) controls the water permeability of collecting tubules in all its length.
- In the presence of ADH, a hypotonic tubular fluid entering the ducts loses water.
- Sodium (Na+) and chloride (Cl+) are reabsorbed in the collecting duct.
- The collecting duct also reabsorbed potassium (K+), ammonia (NH3), and Hydrogen (H+).
- The collecting duct is relatively impermeable to urea.
How will you summarize the Urine formation?
| Chemical substances | Quantity filtered/day | Quantity excreted/day | Amount reabsorbed |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the types of Urine samples?
- Random Sample:
- This is collected without any precaution and may be collected at any time of the day.
- This may be collected for the drug abuse analysis.
- Morning sample:
- This is the first sample when the patient gets up in the morning.
- This is concentrated urine.
- This is the choice of sample for microscopic examination.
- This is also the sample choice for the urine constituents to detect protein, HCG, and other substances.
- 8 hours sample:
- This may be an alternative to the first-morning sample because this will also be concentrated in the urine.
- 24-hour sample:
- This sample is used to quantify any urine solutes like proteins to avoid that substance’s diurnal variation.
- Instruct the patient to void the first sample and note the time. After that, all the samples will be collected until 24 hours have passed.
- Now, void the last sample in the container.
- 24 hours of samples are used for the substances with diurnal variations like catecholamines, 17-hydroxysteroids, and electrolytes.
- Timed Specimen:
- These samples are collected at a predetermined time, like 1,4, or 24 hours.
- A sample patient is given special diet or drug-use instructions for a collection of times.
- Clean catch sample:
- In this case, the patient is instructed to clean the genitalia with water and soap.
- Then, the midstream sample is collected.
- These are used for the bacteriological culture.
- Caution should be taken that the container should not touch the genitalia.
- Catheter samples:
- These are usually collected from seriously ill patients who are already catheterized.
- Or insert the catheter into the urinary bladder to collect the sample.
- These are used for the microbiological examination of critically ill patients.
- Suprapubic sample:
- The sample is directly collected from the urinary bladder using a suprapubic needle that has been completely sterilized.
- This sample is ideal for the culture, and there is a bypass of the urethra.
- This will be a good sample for the culture of the urinary bladder.
- This is usually done from the distended urinary bladder.
- Urine from children:
- Collecting the samples from infants is difficult.
- There are adhesive bags available to put on the urethra to collect urine.
What are the types of urine and their indications?
| Type of urine sample | Indications |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the Urine preservatives?
What is the role of urine preservatives?
- These preservatives are added for the following purposes:
- Reduce bacterial growth.
- Decrease the decomposition of the chemicals.
- Keep the substance in solute form.
- Decreases the atmospheric oxidation of unstable compounds.
- Refrigeration is the most useful tool for collection, and its utility increases with adding preservatives.
- The tablets commercially available are:
- Potassium acid phosphate.
- Sodium benzoate.
- Benzoic acid.
- Methenamine.
- Sodium bicarbonate.
- Red mercuric acid.
What are the advantages of preservatives?
- These tablets act mainly by lowering the pH of urine and releasing formaldehyde.
- Formalin is used as a preservative, but in large amounts, it precipitates urea and inhibits some chemical reactions.
- Acidification of the urine below pH 3 is widely recommended. This is widely used to preserve urine for 24 hours and is particularly useful for calcium, steroids, and vanillylmandelic acid determination. HCL 10 mL, 6 mol/L per 24 hours of urine is used.
- Sulfamic acid is used at 10 g/L to reduce the pH.
- Boric acid is used at 5 mg/30 mL, but it causes precipitation of the urates.
- Toluene is only an organic preservative and is still used; this will not prevent anaerobic microorganisms’ growth.
- Sodium carbonate is used at 5 g/for 24 hours urine sample to preserve the porphyrins and urobilinogen.
What are the various urine preservatives?
Refrigeration:
- When there is a delay in examining urine, refrigerate at 2 C to 8 C.
- Urine can be freezed at -24 C to -16 C.
- If urine collection for the examination is delayed by more than 2 hours, it needs preservatives.
- When urine is refrigerated:
- This will not interfere with the urine chemical tests.
- It prevents bacterial growth.
- Refrigerate for albumin, aldosterone, amylase, chloride, cortisol, estradiol, FSH, lipase, oxalate, protein, and uric acid.
- The disadvantage is there is an increase in the specific gravity.
- Precipitate amorphous phosphates and urates.
HCl (Hydrochloric acid):
- Add 6 mL of hydrochloric acid (HCL) for Aldosterone, calcium, creatinine, cystine, homovanillic acid, 17-ketosteroids, oxalate, and VMA.
Boric acid:
- It will preserve protein.
- Preserves formed elements.
- It will not interfere with the routine examination except for the pH.
- This is bacteriostatic.
- Add boric acid for albumin, cortisol, estrogen, aldosterone, amino acid, chloride, HCG, citrate, cortisol, creatine, DHEA, FSH, glucose, phosphate, 17- Ketosteroids, protein, uric acid, and zinc.
- The disadvantage is that it may precipitate crystals when used in large amounts.
- It interferes with drugs and hormones.
Formalin (formaldehyde):
- It is the best for urine sediments.
- It acts as a reducing agent.
- Rinse the container with formalin to preserve the cells and casts.
- The disadvantage:
- It interferes with chemical tests like glucose, esterase, blood, and white blood cells.
Sodium fluoride:
- It prevents glycolysis.
- This is a good preservative for the drug’s analysis.
- The disadvantage:
- It will interfere with test strips for glucose, white blood cells, and red blood cells.
Phenol:
- It does not interfere with routine tests.
- It changes the odor.
- Use one drop of phenol per ounce of urine.
Toluene:
- It does not interfere with routine tests.
- The disadvantages are that it floats over the surface of the urine and may block the pipette.
Thymol:
- It is an excellent preservative for glucose and sediments.
- The disadvantage:
- It interferes with acid precipitation for the protein.
Commercial preservative tablets:
- It is easy to use when refrigeration is not available.
- Check the tablets’ composition to find any effect on the test.
- These tablets contain the above preservatives and sodium fluoride.
Summarize various urine preservatives?
| Samples | Preservative |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: What is the role of sodium fluoride?
Question 2: What is the purpose of thymol preservative of urine?

Prepare it for pdf form,for easly downloading
Please this website labpedia.net is always present on internet.