Urine for Urobilinogen and Ehrlich Reagent
Urine for Urobilinogen
What sample is needed for urine urobilinogen?
- The test is done in the urine.
- A random sample can be taken.
- 2 hours fresh urine sample can be used, kept cool, and protected from the light.
- The sample is stable at 2 to 8 °C for 24 hours when urine is kept in the dark.
- Don’t expose urine to light or store it at room temperature.
- 2 to 3 hours postprandial after the noon meal is the best sample.
What are the Indications for urine urobilinogen?
- To assess liver function.
- This is the earliest sign of liver disease.
- This is positive in hemolytic anemia.
What are the precautions for estimating urobilinogen in urine?
- False-positive test seen in:
- Drugs containing azo dyes:
- Phenazopyridine.
- Nitrofurantoin.
- Riboflavin.
- p-aminobenzoic acid.
- Highly colored pigments and their metabolites.
- Methyldopa.
- False-negative test seen in:
- Oxidation of urobilinogen to urobilin.
- Formalin preservative.
How will you discuss the pathophysiology of Urobilinogen?
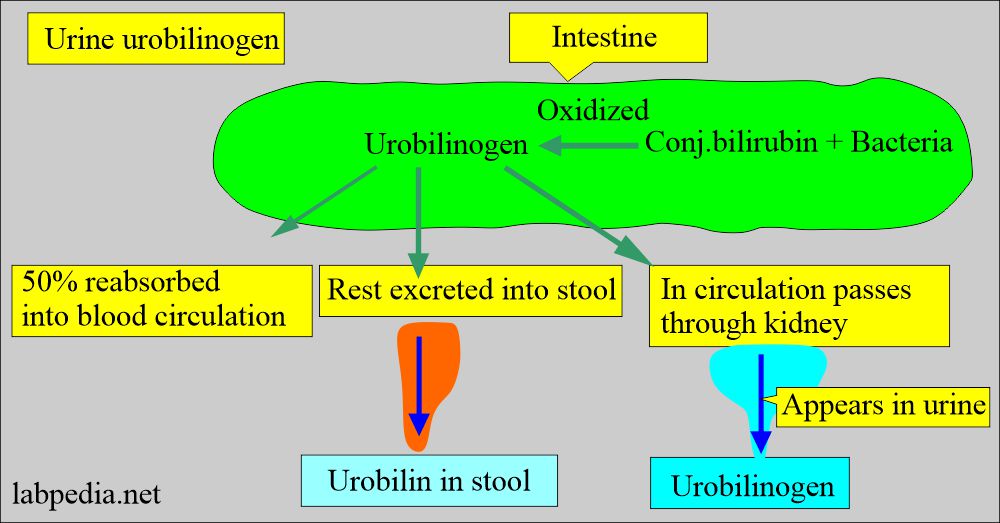
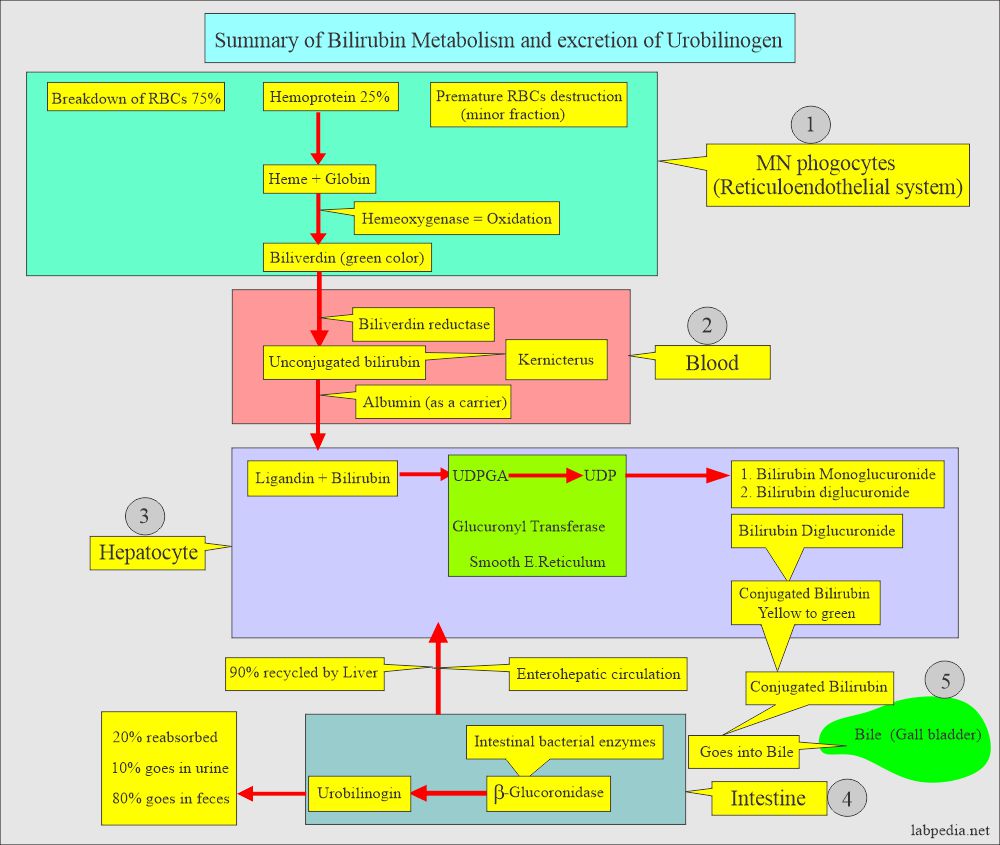
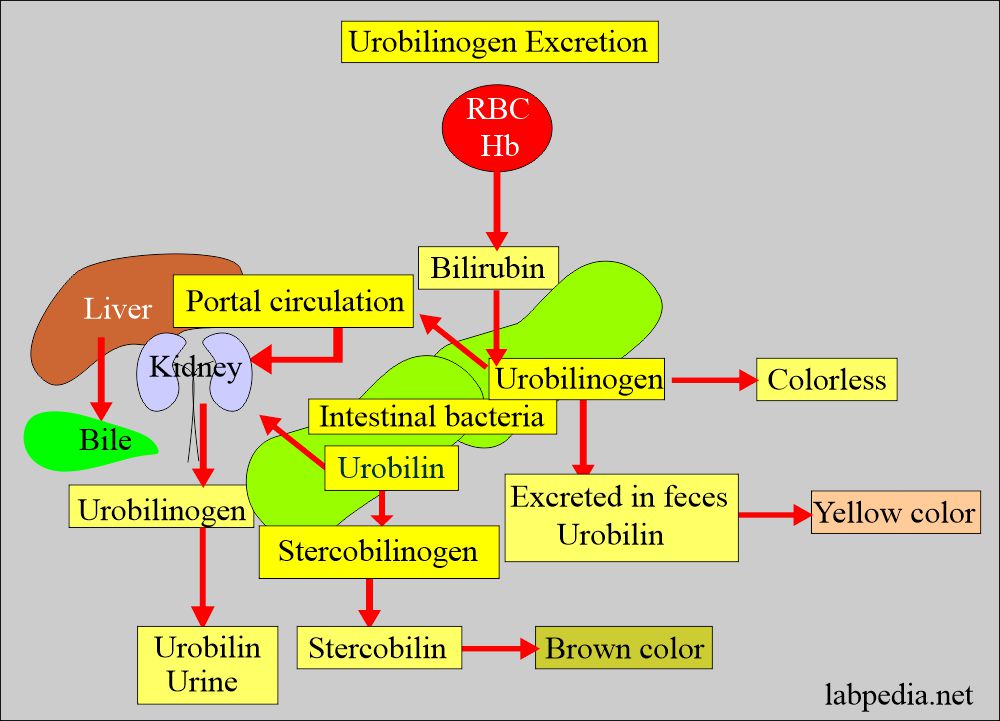
- Hemoglobin breaks into bilirubin and enters the intestine, and thereby, the action of bacteria is transformed into urobilinogen.
- Urobilinogen in the intestine is excreted as urobilin, giving urine a yellow color.
- Urobilinogen in the intestine is reduced to brown stercobilin, giving stool color.
- Urobilinogen is absorbed into the portal circulation, reaches the liver, metabolizes, and excreted into the bile.
- Urobilinogen traces escape removal by the liver and is carried to the kidney and excreted in the urine.
What are the characteristics of urobilinogen?
- Urobilinogen is colorless.
- The intestinal bacteria oxidize urobilinogen to Urobilin, which is a brown pigment.
- Its absence indicates obstructive jaundice.
What is the normal urobilinogen in urine?
- Random sample = < 1 mg/dL.
- 24-hour sample = 0.5 to 4 mg/dL.
Another source
- Urine = 0.5 to 4.0 Ehrlich units/day.
- Feces = 75 to 400 Ehrlich units/day.
Another source
- Urine urobilinogen = 0.1 to 1.0 Ehrlich units /2 hours.
- One Ehrlich unit = approximately 1 mg of urobilinogen.
How will you detect urobilinogen in urine?
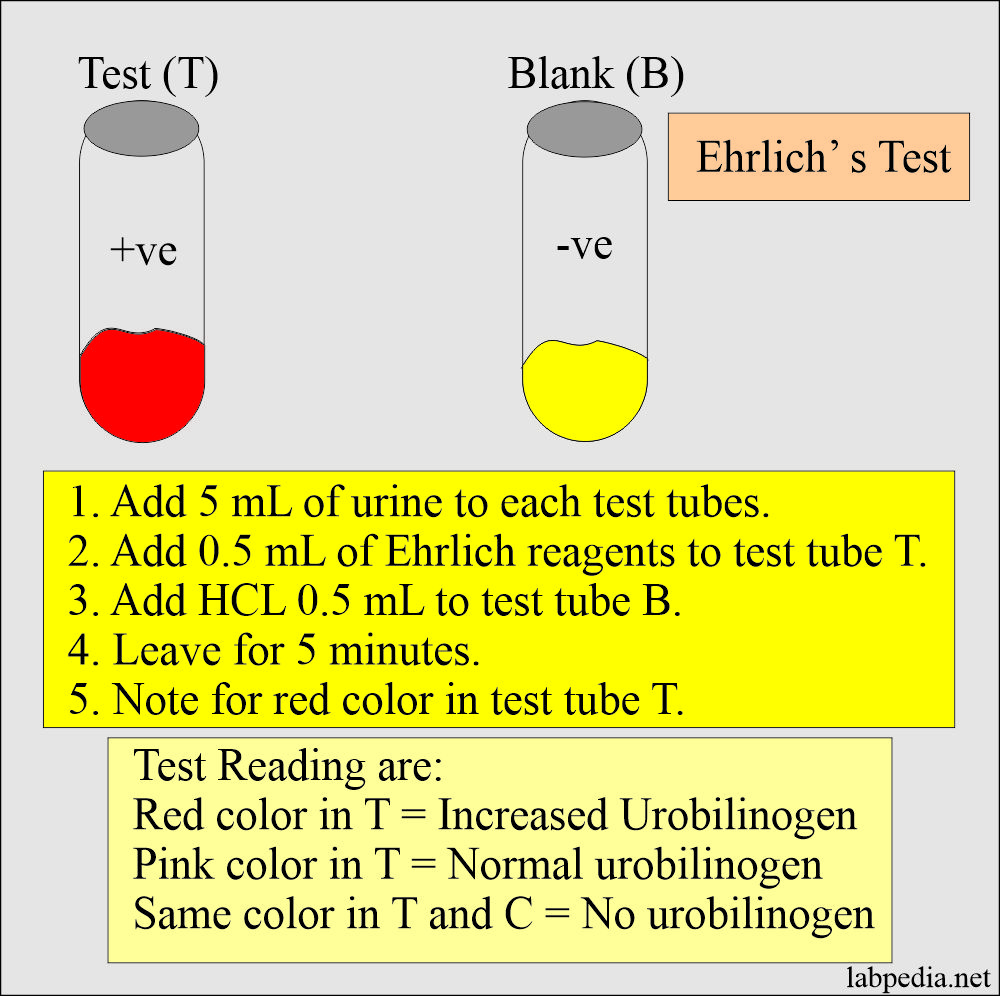
- Add a fresh urine sample to Ehrlich’s reagent.
- Ehrlich’s reagent:
- Principle:
- Urobilinogen + p-dimethylamino benzaldehyde (Erhlich’s reagent) = Form red color.
- Ascorbic acid is added as a reducing agent to keep urobilinogen in a reduced state.
- The addition of saturated sodium acetate stops the reaction.
- Preparation of the reagent Ehrlich’s reagent:
- p-Dimthylaminobenzaldehyde (4-dimethylaminobenzaldehyde) = 4 grams.
- Hydrochloric acid, concentrated = 40 mL.
- Distle water = 160 mL.
- Take the 4-dimethylamino benzaldehyde dissolve in distle water.
- Add the conc HCL and mix well.
- This is stable at room temperature in a colored bottle, especially dark brown. Protect it from sunlight.
- The procedure of the Ehrlich’s reaction:
- Take two test tubes.
- Label one as a test (T) and the other for comparison (B).
- Add 5 ml of freshly voided urine to each test tube.
- Add 0.5 mL of Ehrlich’s reagent to test (T).
- Add 0.5 mL of conc HCL to the B test tube and mix.
- Leave both test tubes at room temperature for 5 minutes.
- Note the red color in the test (T) tube.
- For feces, the same method can be used except:
- Stool Aquos extract is treated with alkaline ferrous hydroxide to reduce urobilin to urobilinogen.
- Now add Ehrlich’s reagent.
What are the causes of increased Urobilinogen in urine?
- Cirrhosis due to:
- Alcoholic cirrhosis.
- Viral diseases.
- Chemicals.
- Biliary obstruction.
- Biliary tract infection, cholangitis.
- Hepatotoxic drugs, e.g.aminosalicylic acid, Phenothiazine, and penicillin,
- Due to increased RBCs destruction:
- Hemolytic anemia.
- Pernicious anemia.
- Malaria.
- Drugs.
- Acute hepatitis.
- Pulmonary infarction.
- Hematoma.
- Excessive ecchymosis.
What are the causes of decreased Urobilinogen in urine?
- Gallstones.
- Biliary obstruction.
- Biliary tract infection (severe).
- Pancreatic cancer (head of the pancreas)
- Drugs, e.g., Aspirin, Chloramphenicol, Insulin, phenytoin, Streptomycin, tetracycline, Methyldopa, and sulphonamide.
Give the differential diagnosis of urine bilirubin and urobilinogen in various conditions?
| Test | Normal person | Hemolytic anemia | Liver disease | biliary obstruction |
|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
Normal urine picture:
| Physical features | Chemical features | Microscopic findings |
|
|
|
Questions and answers:
Question 1: What will be urine urobilinogen in hemolytic anemia?
Question 2: What will be the end result of Ehrlich's reagent for urine urobilinogen?

please, in case of obstructive jaundice why there is urobilin in urine although no bilirubin passed to intestine ??
thanks
Direct bilirubin is water-soluble and in obstructive jaundice, this direct bilirubin can not reach the intestine, instead of enters the bloodstream where it is filtered out by the kidneys and excreted in the urine. Now urine urobilinogen in the obstructive jaundice will be absent. I hope your quaetion is answered.
Why there both increased and decreased of urobilinogen are seen in biliary obstruction? Thought that it would be decreased or absent of urobilinogen in urine for obstuctive jaundice.
When there is an obstruction then conjugated bilirubin is water-soluble and it goes back into the circulation. There is a possibility of the complete absence of urobilinogen in the urine.
In biliary obstruction, below-normal amounts of conjugated bilirubin reach the intestine for conversion to urobilinogen. With limited urobilinogen available for reabsorption and excretion, the amount of urobilin found in the urine is low. High amounts of the soluble conjugated bilirubin enter the circulation where they are excreted via the kidneys.
https://en.wikipedia.org/wiki/Urobilinogen
My urobilogen has suddenly increased to 2.0. There’s also been 2+ hemoglobin, found for well over a year now. Latest test also found mucus (mod) and calcium (rare) the GI doc said it wasn’t a GI issue today. The kidney doc says monitor with CBC and ua every 6 mos or kidney biopsy (she doesn’t think I need) no other options. Monday she told me to discuss my latest results with the GI doc today. I’m SICK. I’ve been complaining about severe nausous, random vomiting, recurring abdominal attacks that start right under my breastbone and spread down and around my back, constant aching. Stabbing. Gas.appetite and weight loss for over a year now and I don’t know what else to do here. Any advice? Thank you
Thanks. I have replied in your email.
Dr. Riaz I have found out through my gastroenterologist that I have fatty liver disease and mild liver stenosis. I keep all my blood test records over the years. The only records that I don’t have is from bloodwork from 3 surgeries at North Broward Medical Center in Florida. 8/2013 RT Hip replacement 4/2015 Cervical Spine surgery in neck and 3/2019 LFT Hip replacement. I checked the bloodwork and urinalysis taken at the hospital and saw that my urobilinogen kept going up. From 1.0 to 2.0 and then 4.0. After many years of normal hemoglobin and the like, after the hip replacement in 3/2019 I developed anemia that did not improve much. After trying Nuiron recommended by my endocrinologist for 6 month with little change, my gastroenterologist have me 2 iron infusions which were successful. I have an appointment in January. I checked with Quest Labs and they don’t test for Urobilinogen. I would like to know if there is a lab anywhere near Boca Raton Florida that accept regular Medicare ( I am 72 ). Unless you fell that it’s not necessary I would appreciate your help.
Urobilinogen test is very simple, and most of the lab can do it. Another possibility is that they may not give importance in the USA and may depend more on Liver function tests. Rest, your physician is the best person to advise.
THANK YOU
Urobilinogen 2.0 and good liver panel. No gallbladder. Autoimmune. Bloating… ankle swelling.. face swelling.. blood in urine past 5 yrs. Vit b12 2000 than 1500. Vit D was diffident now high.
It would help if you had some good physician consultation.
Is all of the urobilinogen in urine converted to urobilin? Does this lab test for both urobilinogen and urobilin?
Ehrlich’ test only detect urobilinogen. Urobilinogen rapidly converted into urobilin. So this should be checked immediately.