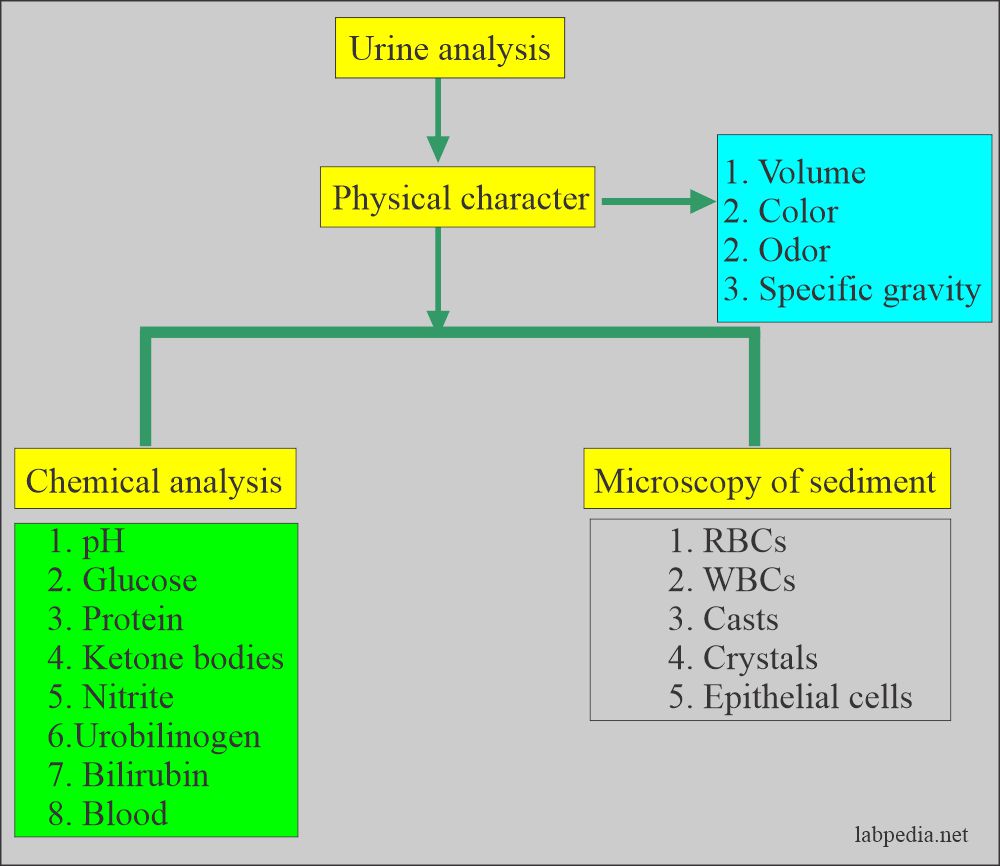
Urine Analysis:- Part 2 -Urine Microscopic Examination and Interpretations
Urine Microscopic Examination
What urine sample is needed for analysis?
- Freshly voided urine is the best sample.
- If delayed, then refrigerate the urine.
- The best volume for the centrifuge is 10 to 12 mL.
What factors will interfere with the urine analysis?
- Certain foods will color the urine, like:
- Carrots will change their urine color to dark yellow.
- Beets may cause red color urine.
- Rhubarb will change its color to red or brown.
- Asparagus produces a typical urine odor.
- If you keep urine on the table, bacteria will change its pH, making it alkaline because of urea-splitting bacteria, and ammonia will be produced.
What is the effect of the food on the urine pH?
- Eating citrus fruits, dairy products, and vegetables makes urine alkaline.
- A high protein diet and some foods (cranberries) make urine acidic.
- A high protein, a fat diet without the intake of carbohydrates also causes ketonuria.
- When radiopaque contrast media is given to the patient will give false-positive urine protein for at least 3 days.
- Females may have contamination from the vaginal secretions and show an increased number of WBCs.
- Traumatic catheterization may cause hematuria and false RBCs in the urine.
- Vaginal secretions contamination may cause false-positive leucocyte esterase.
- False proteinuria is seen when urine is contaminated with vaginal secretions.
- Urine culture gives false-positive results when contaminated with stool, vaginal secretions, and contaminated test tubes or hands and clothes.
How will you process the urine for microscopy?
- Centrifuge the Urine; clear supernatant is removed and leaves the uniform volume of sediment, usually 1 mL.
- The recommended time for centrifugation is 5 minutes.
- The standard centrifugation speed recommended is 400 g.
What is the normal urine sediment?
- Normally, there is no sediment or very little.
What are the normal contents of the sediments?
| Normal contents of the urine | Findings in the sediments |
|
|
|
|
|
|
|
|
|
|
|
|
What are the microscopic contents of urine?
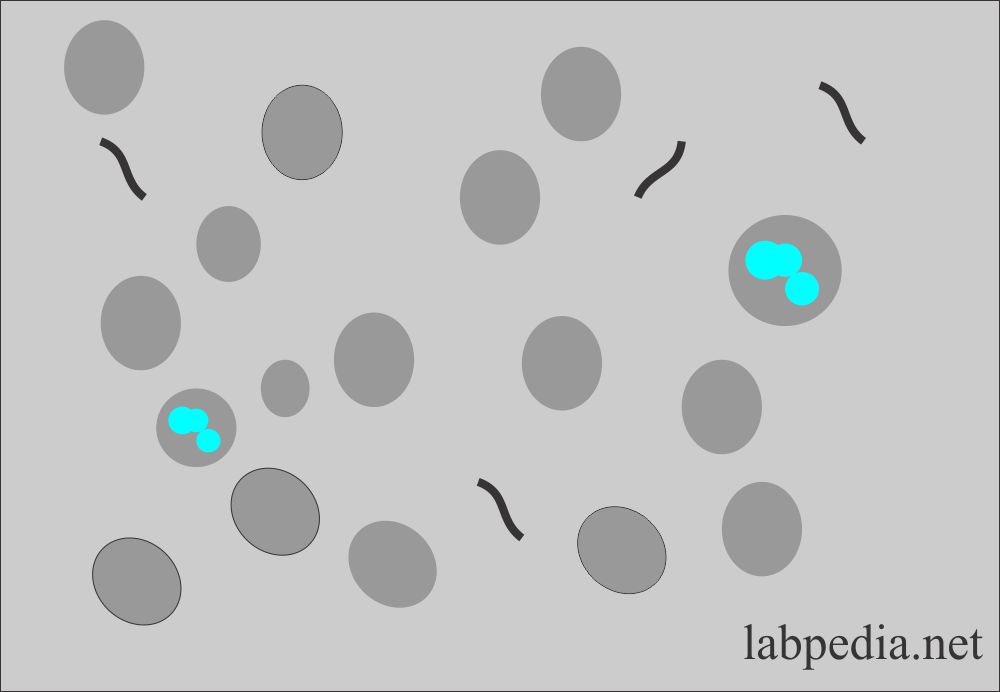
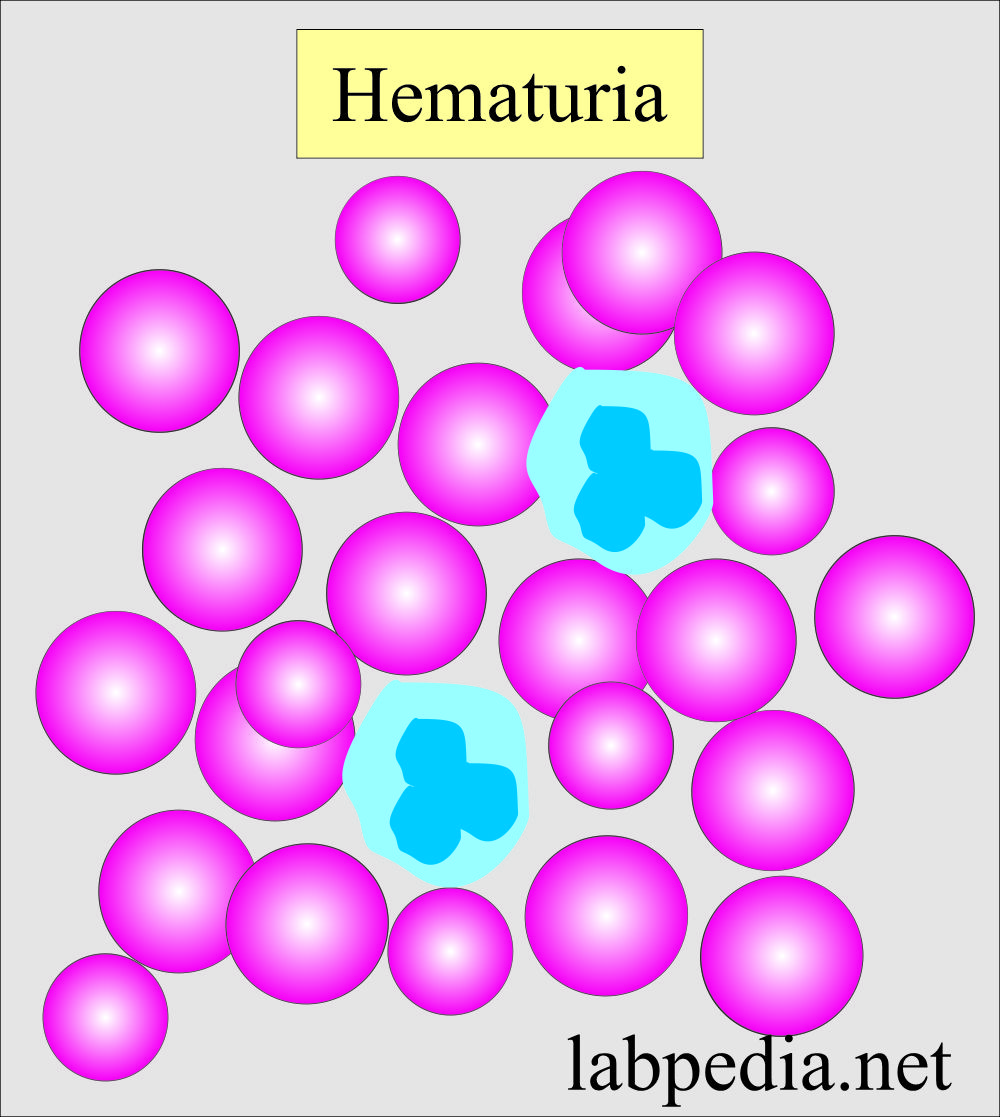
Red blood cells in urine:
- The presence of RBC in the urine is called Hematuria.
- RBCs are seen as biconcave, non-nucleated discs measuring 7 µm in diameter.
- The presence of RBC is an indicator of renal disease.
- These are reported in a routine as the average number seen in 10 HPF (x400).
- RBCs swell and lyse rapidly in the diluted urine, releasing their hemoglobin and leaving only the cell membrane; these empty cells are called ghost cells. These can only be seen in reduced light. Otherwise, these are missed.
- RBCs are confused with:
- Yeast.
- Oil droplets.
- Air bubbles.
- How do we differentiate RBCs in the urine?
- Oil droplets and air bubbles are highly refractile.
- These are seen on a different level than the other sediments.
- RBCs are smaller than WBCs.
- Add acetic acid to the sediment, lyse the RBCs, and leave yeast, oil droplets, and air bubbles behind.
- Or do the supravital staining.
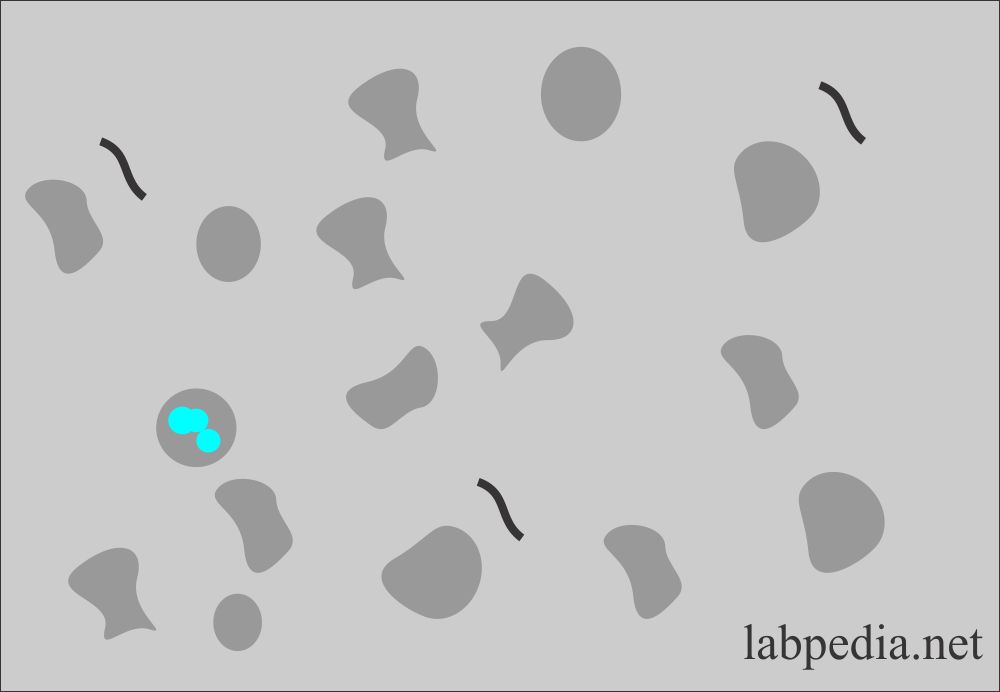
How will you define dysmorphic RBCs?
- These RBCs vary in size, have cellular protrusions, or may be fragmented.
- Wright’s stain can also help to differentiate these RBCs as hypochromic and prominent cellular blebs and protrusion.
- These RBCs are associated with glomerular bleeding.
- These are also seen after strenuous exercise, indicating glomerular RBCs.
What is the macroscopic hematuria?
- It shows cloudy urine with a red to brown color.
- This is seen in the following conditions:
- Trauma.
- Acute infection.
- Inflammation.
- Coagulation disorders.
How will you describe microscopic hematuria?
- Glomerular diseases.
- Malignancy of the urinary tract.
- Renal calculi.
- The possibility of menstrual contamination should be considered in females.
What are the causes of Hematuria?
- Renal disease
- Infections
- Renal stones
- Renal tumors
- Bleeding disorder.
- Anticoagulant therapy.
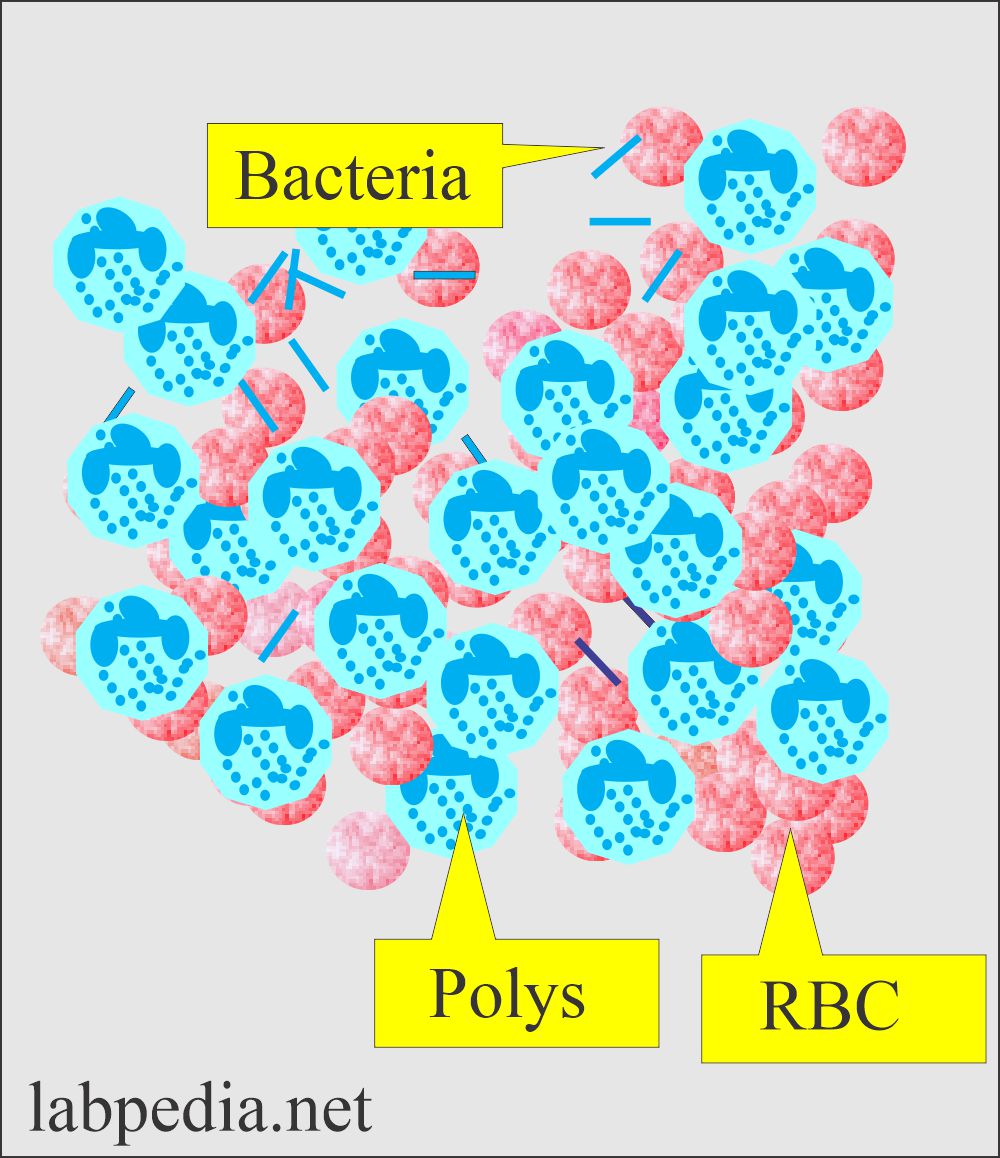
White Blood Cells (WBC), Neutrophils:
- WBCs are bigger than the RBCs, measuring an average of 12 µm in diameter.
- In the urine sediment, recognizing the WBCs is easier than recognizing the RBCs.
- Neutrophils contain multilobate nuclei and granules in the cytoplasm.
- WBCs can be identified in the high power and reported as the average number in 10 HPF.
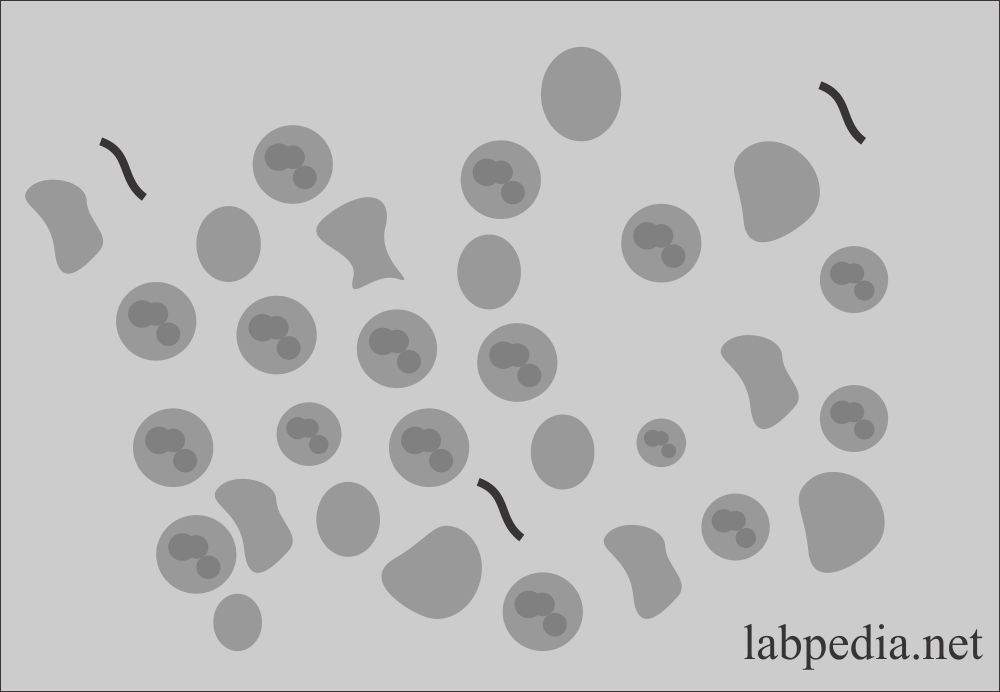
Urine analysis: Urine WBCs in the sediment
- Neutrophils lyse rapidly in the dilute alkaline urine and begin to lose nuclear details.
- An increased number of WBCs in the urine is called Pyuria.
- Pyuria may be caused by:
- Bacterial infection of the urinary tract.
- Acute pyelonephritis shows casts along with WBCs, proteins, and bacteria.
- Lower urinary tract infection also shows WBCs but a small amount of protein.
What is the normal number of WBCs in the urine?
- Normally, few Neutrophils are seen.
- Usually 4 to 5 /HPF.
- >30 cells /HPF is considered an infection.
- WBCs clumps are a sign of infection and must be reported
What are the causes of increased neutrophils in urine?
- All renal inflammatory diseases.
- Glomerulonephritis.
- Cystitis and urethritis.
- Chronic pyelonephritis.
- Prostatitis.
- Pyogenic infection.
- Acute appendicitis.
- Acute pancreatitis.
- Tuberculosis.
- Urinary bladder tumors.
What are the causes of nonbacterial increased WBCs?
- SLE.
- Interstitial nephritis.
- Glomerulonephritis.
- Tumors.
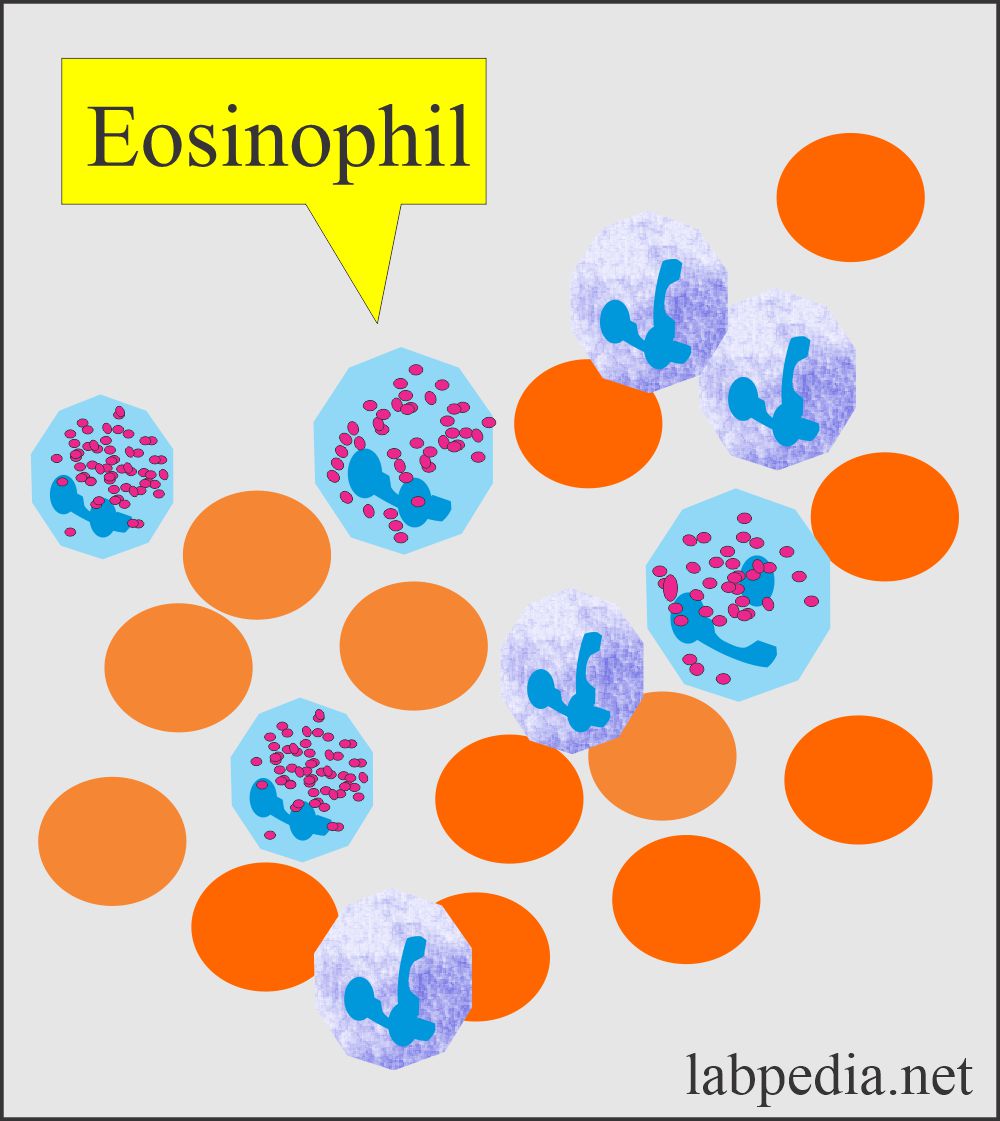
Eosinophils in urine:
- Eosinophils are usually not seen in urine sediment but may be present in a few, along with neutrophils.
- Eosinophils are difficult to recognize on wet preparation except for 2 or 3 lobes.
- The supravital stain detects these.
- Use Wright’s or a special stain for eosinophils like Methylene-blue and eosin-Y in methanol.
- Eosinophils may be seen in:
- Drug-induced interstitial nephritis (hypersensitivity), e.g., penicillin and its derivatives.
- Acute genitourinary diseases like tubulointerstitial disease.
- These are also seen in renal transplantation rejection.
How would you work to see eosinophils?
- Centrifuge the urine; concentrated sediments are needed to stain it.
- Or prepare the smear with a cytospin centrifuge.
- The best stains are Hansel’s stains, but you can use Wright’s stains.
- >1% eosinophils are a significant number.
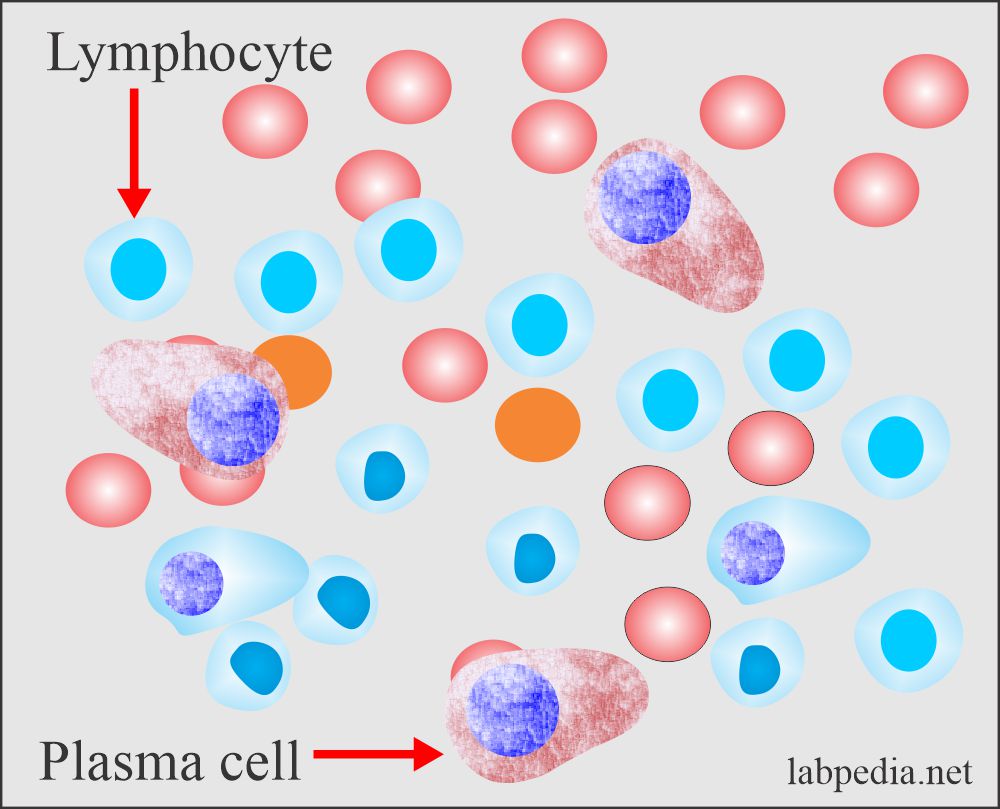
Lymphocytes in urine:
- Normal urine may contain a few small lymphocytes which are not recognized.
- Wright’s stain can recognize them.
- An increased number of lymphocytes is seen in the following:
- The first few weeks of renal transplantation are a sign of rejection.
- Many lymphocytes and plasma cells show renal transplantation rejection and acute renal allograft rejection.
Monocytes, Histiocytes, and Macrophages in urine:
- These cells are difficult to recognize in wet preparation. Normally, there are monocytes, macrophagic cells, and histiocytes.
- Lymphocytes are smaller than WBCs and may resemble RBCs.
- Monocytes, histiocytes, and macrophages are large cells and are vacuolated with inclusions.
- Recognizing these cells needs a special stain (Wright’s and Papanicolaou’s).
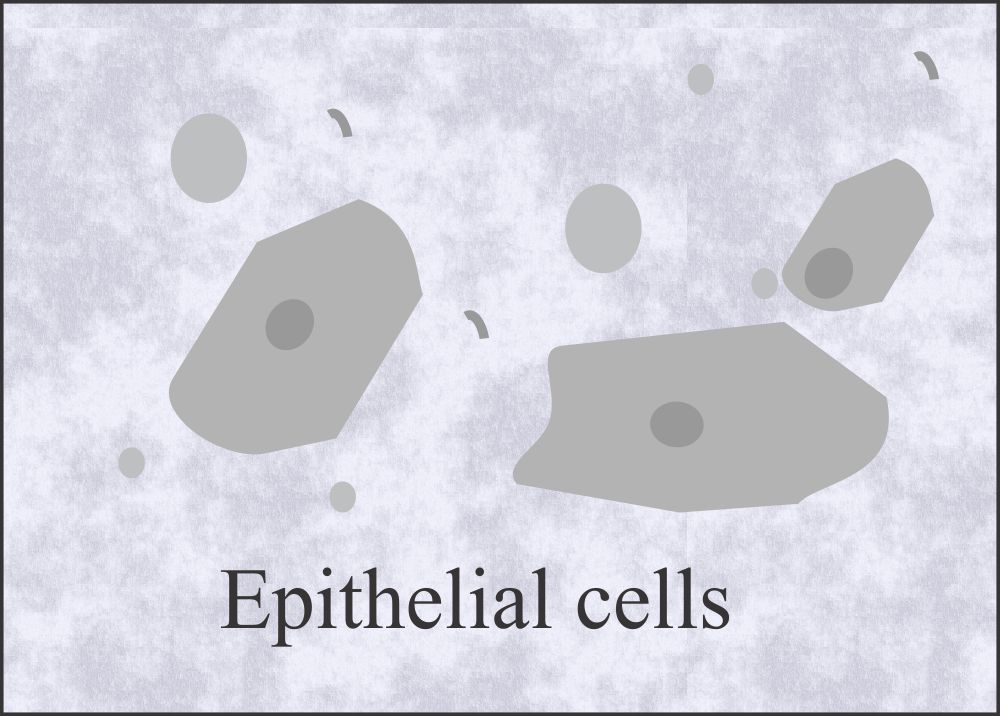
Epithelial cells in urine:
- These cells are mainly shed from the urethra and urinary bladder.
- Few renal epithelial cells are seen normally in the sediment.
- Epithelial cells are the following types :
- Squamous epithelial cells
- Transitional epithelial cells
- Renal epithelial cells.
Squamous epithelial cells in urine:
- These cells line the female urethra, trigone, and male urethra.
- These cells also line the vagina, and in the female, these are the source of contamination.
- What is the Origin of squamous epithelial cells?
- These squamous epithelial cells take origin from the vagina, female urethra, and lower portion of the male urethra.
- These represent normal sloughing and have no pathologic significance.
- Midstream clean catch will have less number of these cells.
- These cells have little significance but help to focus on the microscope.
- What is the morphology of squamous epithelial cells?
- These large cells contain abundant irregular cytoplasm and a prominent nucleus, which may be around the size of an RBC.
- The squamous epithelial cells are reported as follows:
- Rare
- Few.
- Moderate.
- Many.
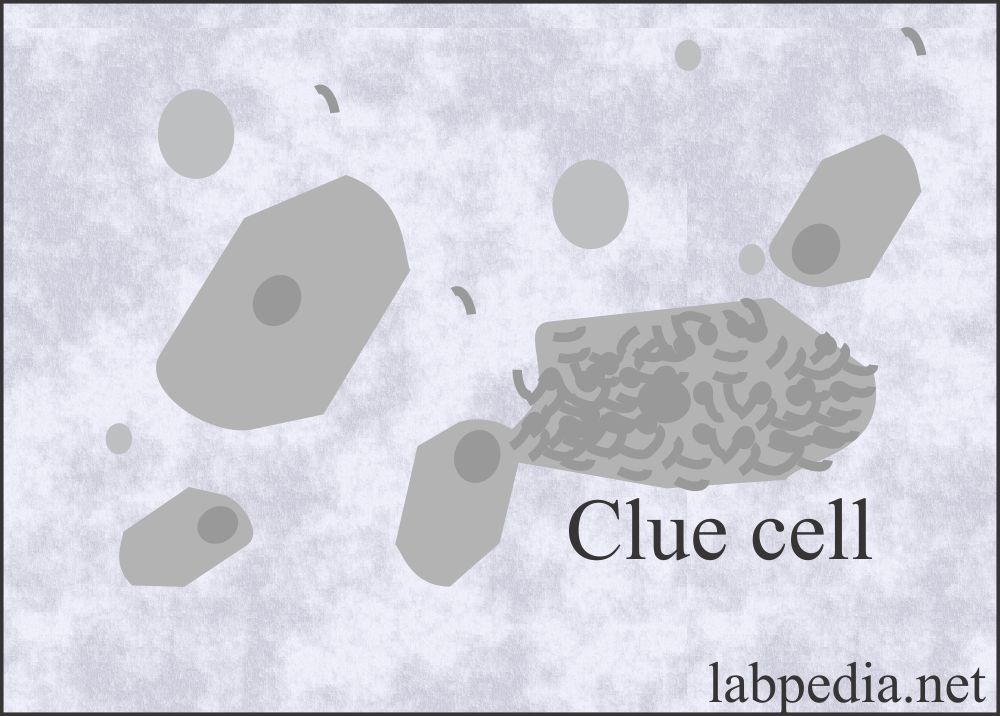
Clue cells in the urine:
- These are a special type of squamous cell and take their origin from the vagina. These are covered by coccobacilli (Gardnerella vaginalis) and indicate bacterial vaginitis.
- A small number of clue cells may be present in the urine sediment.
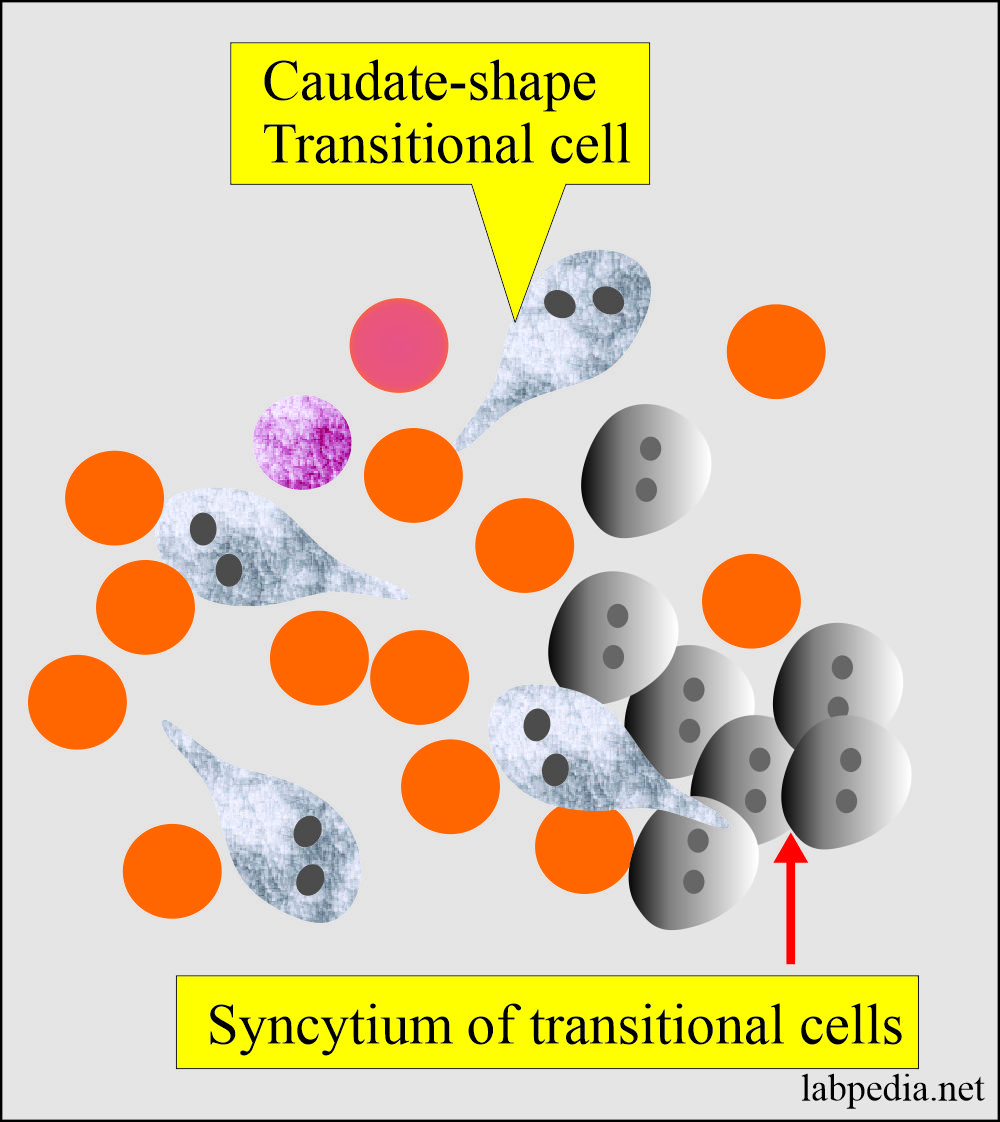
Transitional Epithelial cells in the urine:
- These are stratified epithelial linings of the urinary tract system, starting from the kidney’s pelvis and moving to the urinary bladder base in the female and proximal parts of the male urethra.
- What is the morphology of the transitional cells?
- These are smaller than the squamous epithelial cells.
- These have various shapes, like spherical, polyhedral, and caudate forms.
- All forms have a distinct central nucleus.
- These cells originate from the lining of the renal pelvis, calyces, ureter, urinary bladder, and upper part of the urethra.
- How will you Report the Transitional cells?
- Normal urine may contain few transitional cells.
- Rare.
- Few.
- Moderate.
- Many.
- Renal cells exfoliate more in:
- Inflammatory process and infection.
- Malignancies.
- After radiation, these cells become large and have multiple nuclei.
- After catheterization or washing of the urinary bladder.
- These cells need special stains.
- An increase in the number of transitional epithelial cells with abnormalities like vacuoles in the cytoplasm and irregular nuclei may suggest malignancy or viral infection; such cases need cytological examination.
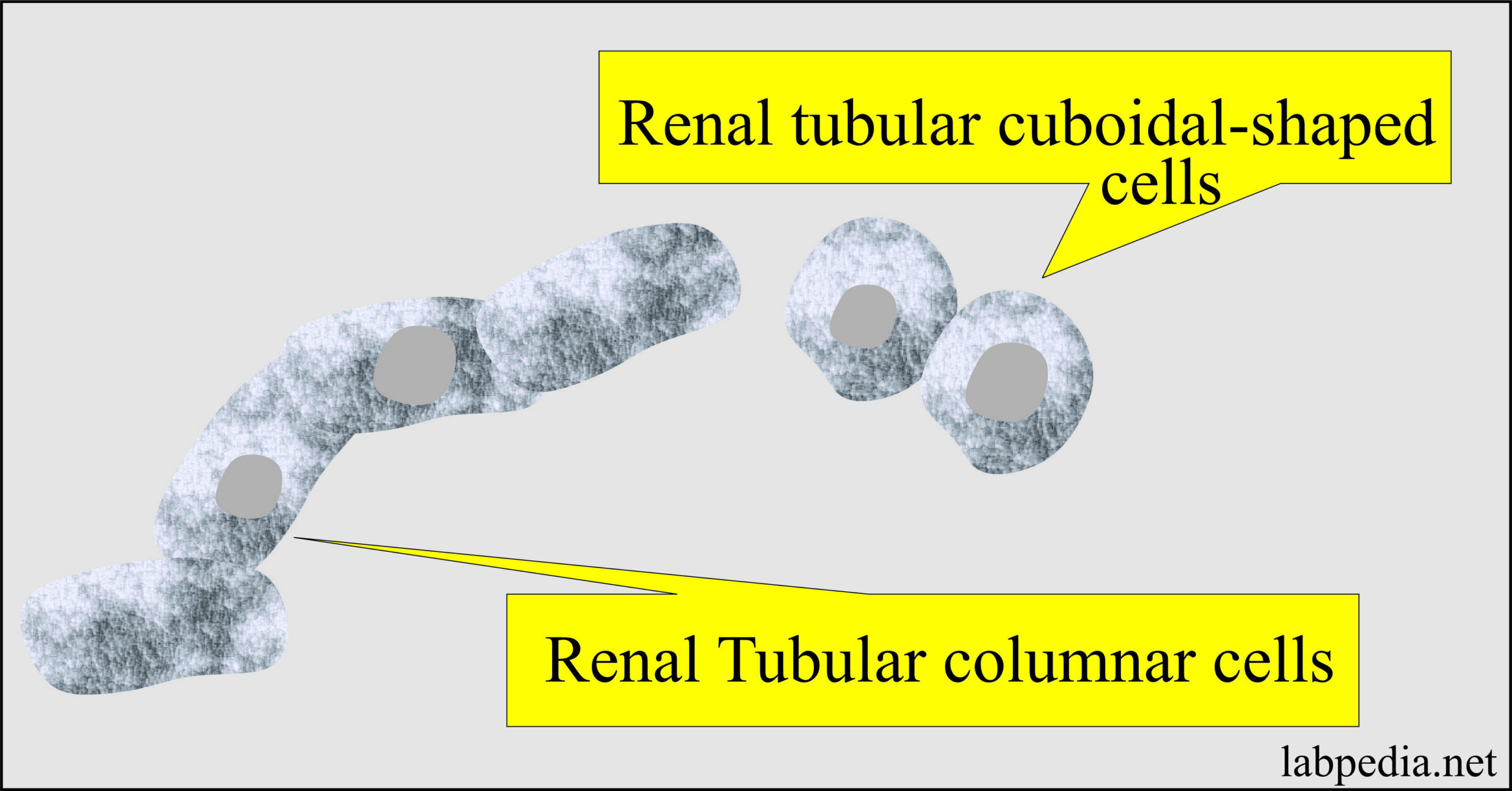
Renal Tubular Epithelial cells in urine:
- These cells line the proximal to distal convoluted tubules and small and large collecting ducts.
- Proximal convoluted tubular cells are rectangular, coarsely granular cytoplasm.
- Collecting duct cells are cuboidal to columnar, finely granular, and not larger than WBCs.
- Normally, a few cells may be found in the urine sediment.
- An increased number is significant, indicating renal disease.
- What is the function of renal tubular cells?
- The main function of these cells is reabsorption.
- In hemoglobinuria, these cells contain yellow-brown hemosiderin pigments.
- In the case of bilirubin, the color of these cells is deep yellow.
- The critical number is more than 15 cells/10 HPF. When >2 cells are found, cytologic examination is recommended.
- What is the significance of renal tubular cells?
- When present in groups, it indicates severe renal damage.
- Acute tubular necrosis.
- It is seen in heavy metal poisoning.
- Drug-induced toxicity.
- Hemoglobin and myoglobin toxicity.
- Viral infections like HBV.
- Pyelonephritis.
- Viral infections.
- Allergic reactions.
- Acute allogenic Rejection phenomenon.
- Malignant infiltration.
- These are not easily identified in the centrifuged material. It needs special stains.
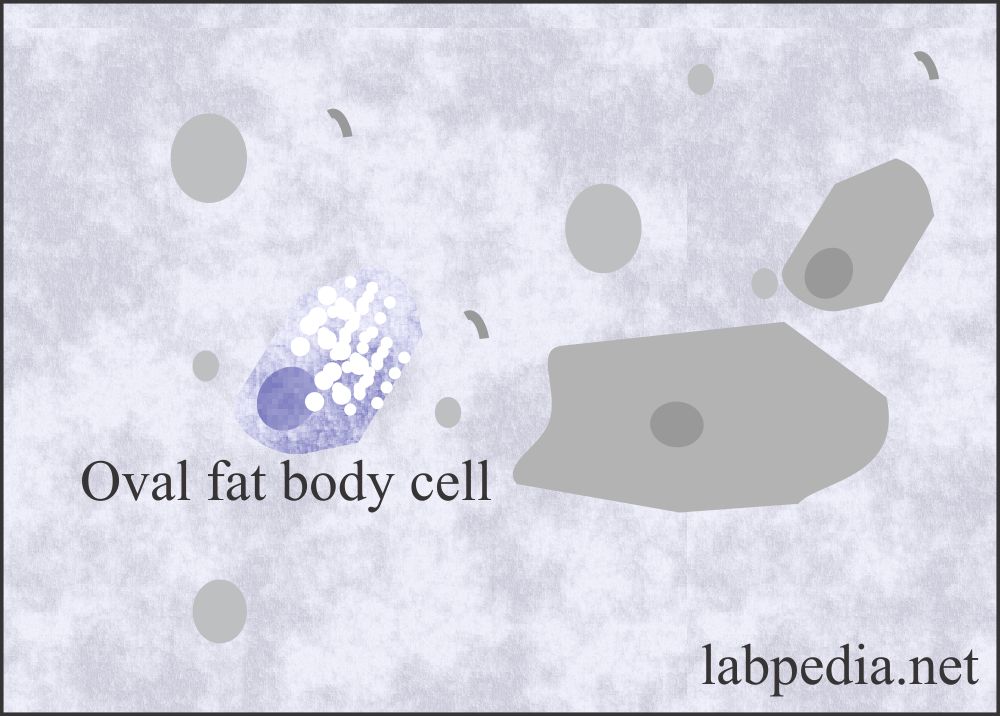
Fat Globules and Fat Oval Bodies:
- Tubular cells absorb the fat, which is present in the glomerular filtrate.
- These cells containing the fats are refractile, and the nucleus is difficult to see. These fat-containing renal tubular cells are called fat oval bodies.
- These fat oval bodies can be seen in the polarized microscope with the special Sudan black III or oil red O fat stain.
- These are seen along with fat globules or droplets.
- These fat droplets consist of triglycerides, neutral fat, and cholesterol.
- The fat stain will stain triglycerides and neutral fat and give an orange-red color.
- Fat in the urine is called lipiduria. It is usually seen in nephrotic syndrome when the glomeruli are damaged.
- Special stain Sudan 111 or oil red O is needed.
- What are the causes of Lipiduria?
- Advanced diabetes mellitus.
- Severe tubular necrosis.
- Nephrotic syndrome.
- Lupus disease.
- In mercury poisoning.
- Ethylene glycol poisoning.
- In trauma, bone marrow fats leak from the long bone.
- Lipid storage disease is when large fat-laden histiocytes are present. These are differentiated from fat oval bodies by their large size.
Spermatozoa in urine:
- The spermatozoa are oval, slightly tapered heads and long flagellate-like tails.
- Urine is toxic to sperms, so they are nonmotile in the urine.
- There should be a lab protocol when reporting spermatozoa in the urine, particularly female urine. There may be legal consequences.
- These may be seen in males and females following intercourse (coitus).
- Spermatozoa in the urine is significant in infertility cases and sexual abuse.
- In males, it may be seen after a nocturnal emission or ejaculation.
- Also seen in diseases of the genital tract.
- Their presence in the urine is of significance in the case of retrograde ejaculation, where the sperms go into the urinary bladder instead of the urethra.
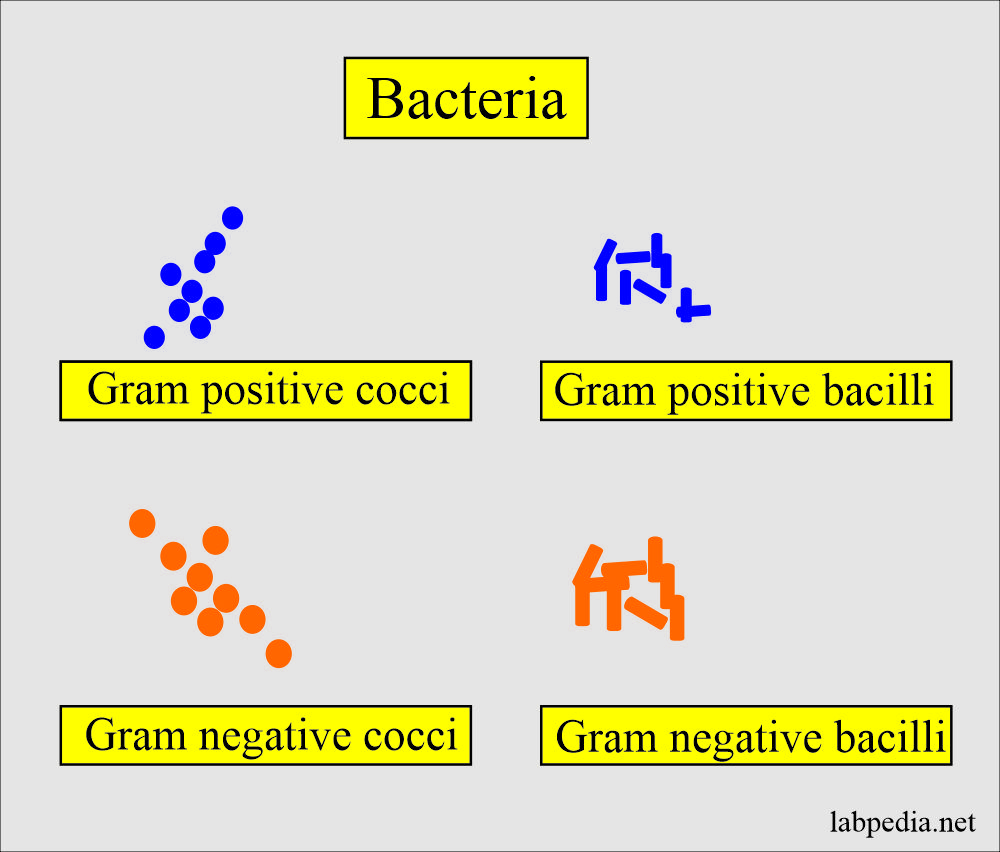
Bacteria in the urine:
- Few bacteria are present unless you collect the urine in strict sterile conditions.
- There are bacteria due to contamination from the vaginal secretions, urethra, genitalia, or the container.
- These bacteria multiply if the urine is left at room temperature and give a nitrite test positive and may result in pH 8, which indicates an unacceptable specimen.
- If urine is kept at room temperature in the lab, bacteria can multiply.
- When bacteria are seen in the urine, they should be reported per high power as:
- Few.
- Moderate.
- Many.
- When reporting bacteria, then you should see the WBCs in the urine.
What is the % of bacteria causing urinary infection?
| Type of bacteria causing infection | % of urinary tract infections |
|
|
|
|
|
|
|
|
|
|
|
|
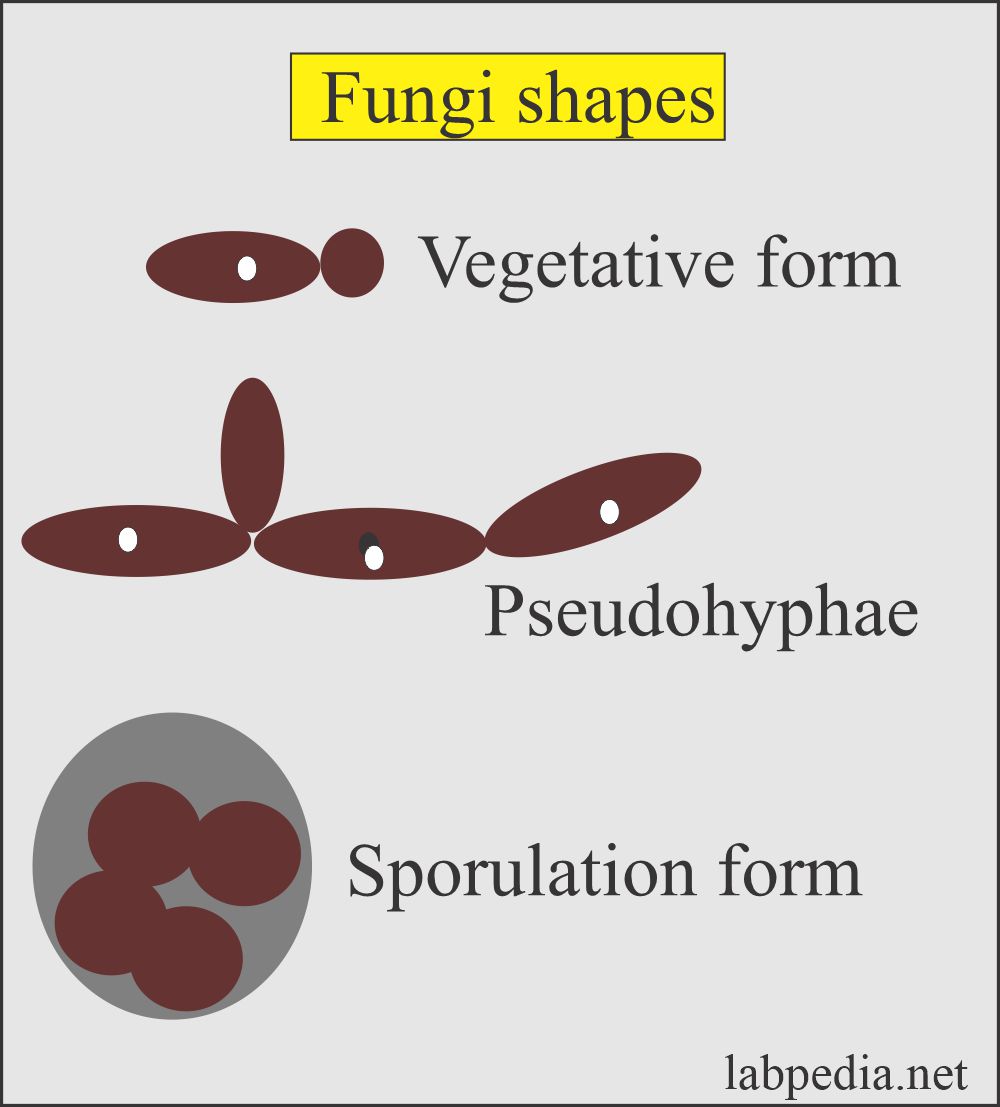
Yeast in the urine:
- The most common yeast in the urine is candida.
- There may be vaginal contamination due to vaginal infection.
- This yeast, primarily candida, is seen in:
- The patients with diabetes. Because sugar is used as a source of energy for yeast growth.
- These are also seen in immunocompromised patients.
- Female with vaginal moniliasis.
- The infection is suspected when the presence of WBCs accompanies candida.
- What is the structure of yeast?
- These may be seen as small, refractile oval structures that may be laking buds.
- These are strongly gram-positive.
- Wright’s stain differentiates yeast from the RBCs.
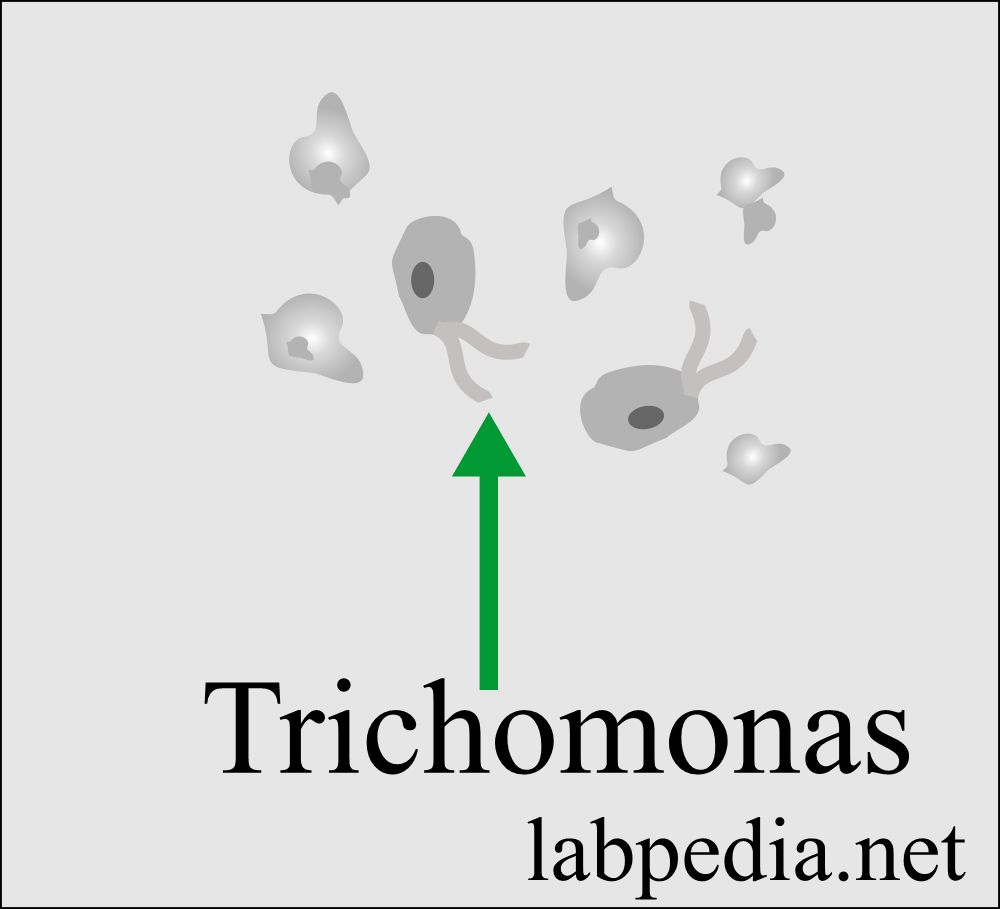
Trichomonas (parasites):
- This protozoan is the common cause of vaginal infection called Trichomonas vaginitis caused by Trichomonas vaginalis.
- Trichomonas is a sexually transmitted disease that causes inflammation in females.
- While the infection of the male urethra and prostate is asymptomatic.
- What is the structure of Trichomonas?
- Trichomonas is a pear-shaped flagellate with an undulating membrane.
- It is easily identified in a wet preparation and the urine sediment by its rapid darting movement under the microscope.
- Identifying when these are not moving is challenging because they resemble WBCs or transitional cells.
- How will you report trichomonas/HPF?
- Rare.
- Few.
- Moderate.
- Many.
- These protozoa reside in the prostate and vagina.
- Wet preparation from the vagina or urethra by direct swab preparation can diagnose it.
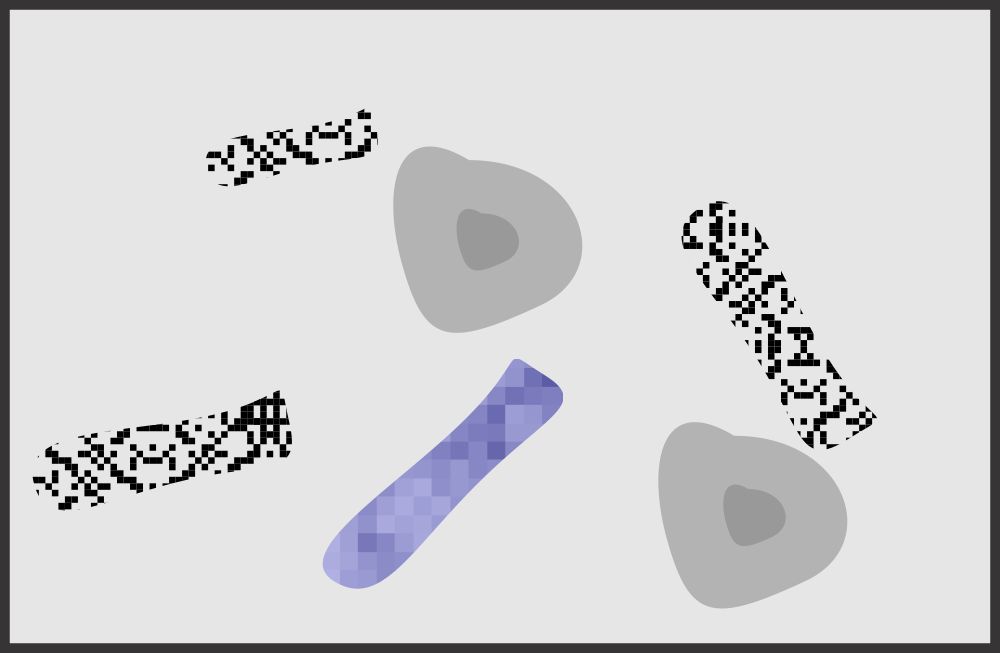
Casts in the urine:
What is the mechanism of the formation of the cast?
- These casts are precipitated proteins in the tubules. It forms in the lumen of distal convoluted tubules and collecting ducts.
- Their shape is representative of the tubular lumen with parallel sides and mostly rounded ends.
- The shape and content of the cast depend upon:
- The material is present in the filtrate at the time of formation.
- Length of time, it remains in the tubules.
- Any other components present in the filtrate at the time of formation, like bacteria, granules, pigments, and crystals, may become embedded in or attached to the cast matrix.
- The casts dissolve easily in the dilute alkaline urine.
Composition of the cast:
- The major component is the Tamm-Horsfall protein. This protein is produced from the renal tubular epithelium and upper collecting ducts.
- Other proteins are albumin and immunoglobulins.
- These proteins gels under the following conditions:
- Urine flow stasis.
- The acidity of the urine.
- In the presence of Na+ and Ca++.
- Protein glycosylation is also important.
- The width of the cast depends on where the cast is formed.
- These casts lead to blockage of the urinary outflow in the tubules.
- Reporting:
- These are screened under low power and are usually seen at the edges of the coverslip.
- It also needs low light because the cast refractive index is low.
- After identifying under the low light, go to high-power magnification and report cast number / 10 HPF.
- There are the following types of casts seen in the urine:
- Hyaline cast
- Cellular cast
- Waxy cast
- Granular cast
- Pigmented cast (maybe hemoglobin, myoglobin, bilirubin, and drugs casts)
- Fatty cast
- Inclusion cast
Hyaline casts:
- Hyaline casts are the most common casts.
- This cast mainly consists of Tamm-Horsfall protein. In unstained sediments, it is colorless, and its refractive index is like urine’s.
- These can be easily seen in phase microscopy.
- Or stain with Sternheimer-Malbin, which produces the pink color of these casts.
- These are of the least importance.
- Normal:
- There may be <2 / PHF seen in a normal person (0 to 2 /HPF are normal).
- These may be seen without any significant proteinuria.
- These are seen in acidic urine and absent in alkaline urine.
- Normally, Hyaline casts are seen in the following:
- After severe exercise.
- Dehydration.
- Emotional stress.
- Heat exposure.
- Pathologically hyaline casts are seen in:
- Acute glomerulonephritis.
- Chronic renal disease.
- Pyelonephritis.
- Congestive heart failure.
- > 20 / PHF is seen in moderate or severe renal disease.
Granular casts:
- What is the structure of granular cast?
- Granulat cast appears homogenous, coarsely granular, colorless, and very dense.
- These casts are a breakdown of cells and plasma protein aggregates (fibrinogen, immune complexes, and globulin in the Tamm-Horsfall matrix).
- What is the normal number of granular casts?
- Few may be seen in a normal person or after vigorous exercise.
- Occasional 0 to 2 /HPF.
- Granular casts are seen in:
- Acute tubular necrosis.
- Pyelonephritis.
- Advanced glomerulonephritis.
- Malignant nephrosclerosis.
- The increased number indicates severe renal disease.
- Presence of cells in the cast:
- Red cells in the cast indicate a glomerular injury.
- The presence of epithelial cells indicates renal tubular injury.
- The presence of WBC indicates infection or interstitial injury.
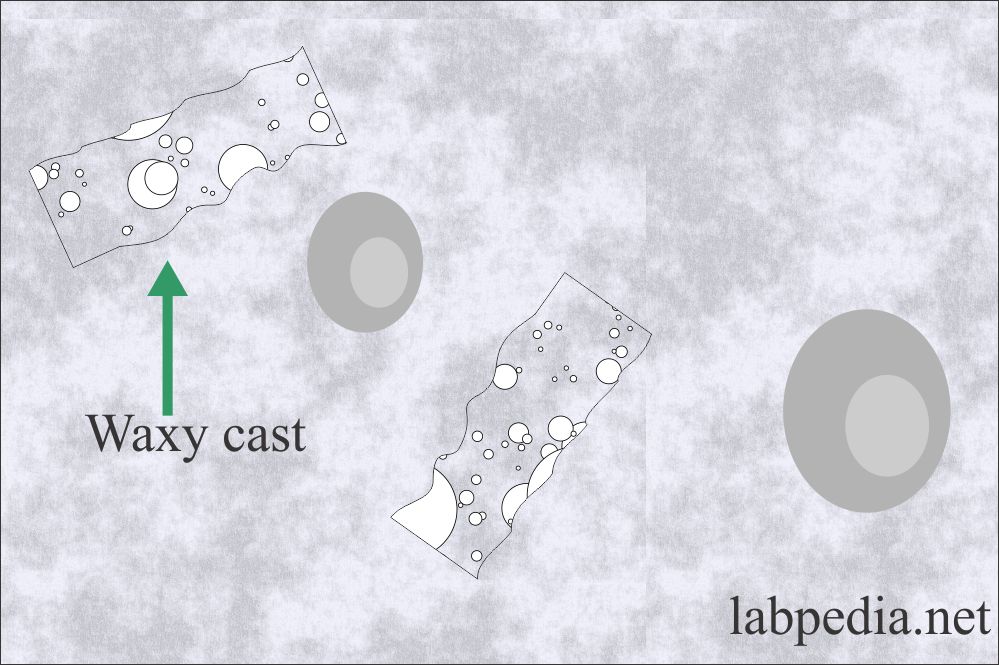
Waxy casts:
- These are not seen normally in the urine.
- What is the structure and formation of waxy casts?
- Waxy casts formed from the degeneration of the granular cast.
- These casts are larger than the other casts and are waxy and granular in appearance.
- These are broader than other casts and called broadcast, or broad renal failure casts.
- These are like the hyaline cast but are more refractile and have sharper outlines.
- These are also called renal failure casts.
- Their presence indicates severe pathology.
- Waxy casts are seen in:
- Chronic renal disease.
- Severe renal failure.
- Renal amyloidosis.
- These are rare in acute renal disease.
- Malignant hypertension.
- Renal amyloidosis.
- Diabetic nephropathy.
- Renal allograft rejection.
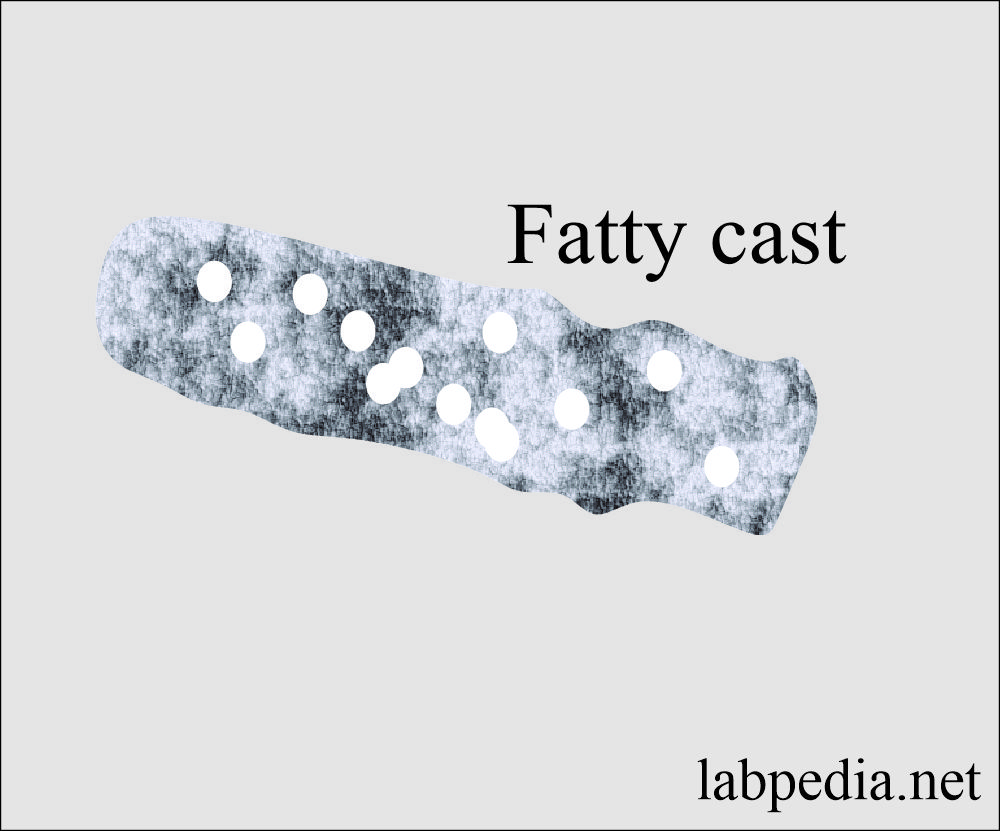
Fatty casts:
- What is the mechanism of formation of fatty casts?
- Fat casts are formed from the fat droplets’ attachment and degenerating fat oval bodies embedded in the protein matrix.
- Fatty casts are highly refractile and contain yellow-brown fat droplets or fat oval bodies.
- These also indicate severe renal disease.
- Where will you see fatty casts?
- Nephrotic syndrome.
- Chronic glomerulonephritis.
- Severe diabetes mellitus.
- Toxic nephrosis due to mercury poisoning and ethylene glycol.
- SLE.
- Toxic renal poisoning.
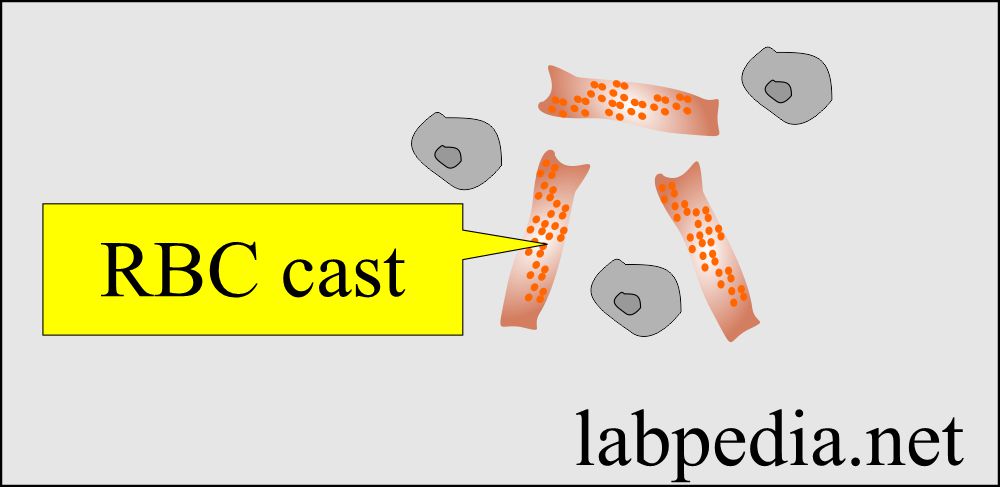
Red Blood Cell cast:
- Fresh RBCs cast retain their brown pigments and consist of RBCs in a tubular cast matrix.
- These casts indicate intraparenchymal bleeding.
- These are the hallmarks of glomerulonephritis.
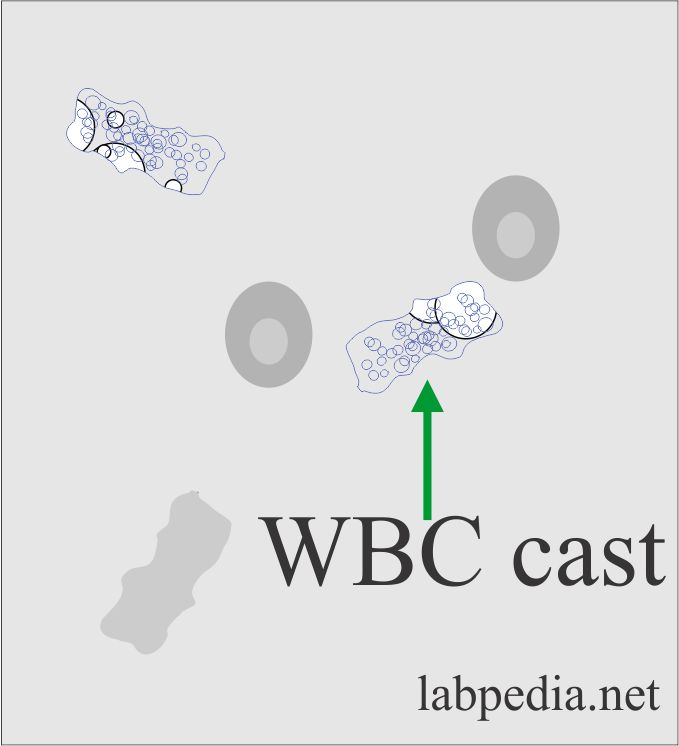
White Blood Cell cast:
- There are WBCs in a protein matrix.
- These originate from kidney tubules.
- Where will you see WBC casts?
- These are characteristics of pyelonephritis.
- Interstitial nephritis.
- Tubulointerstitial infection.
- These are used fully to distinguish from lower urinary tract infections.
- Normal:
- Not seen normally.
Tubular Cell Cast:
- There are few tubular cells in a hyaline matrix of dense aggregates of shed tubular cells.
- These are seen in concentrated urine.
- Tubular cell sloughing occurs in acute tubular necrosis.
What is the association of various casts with diseases?
| Type of cast | Clinical disease association |
|
|
|
|
|
|
|
|
|
|
|
|
What is the etiology of various casts in the urine?
| Nature of the cast | Physical appearance | Possible reason |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
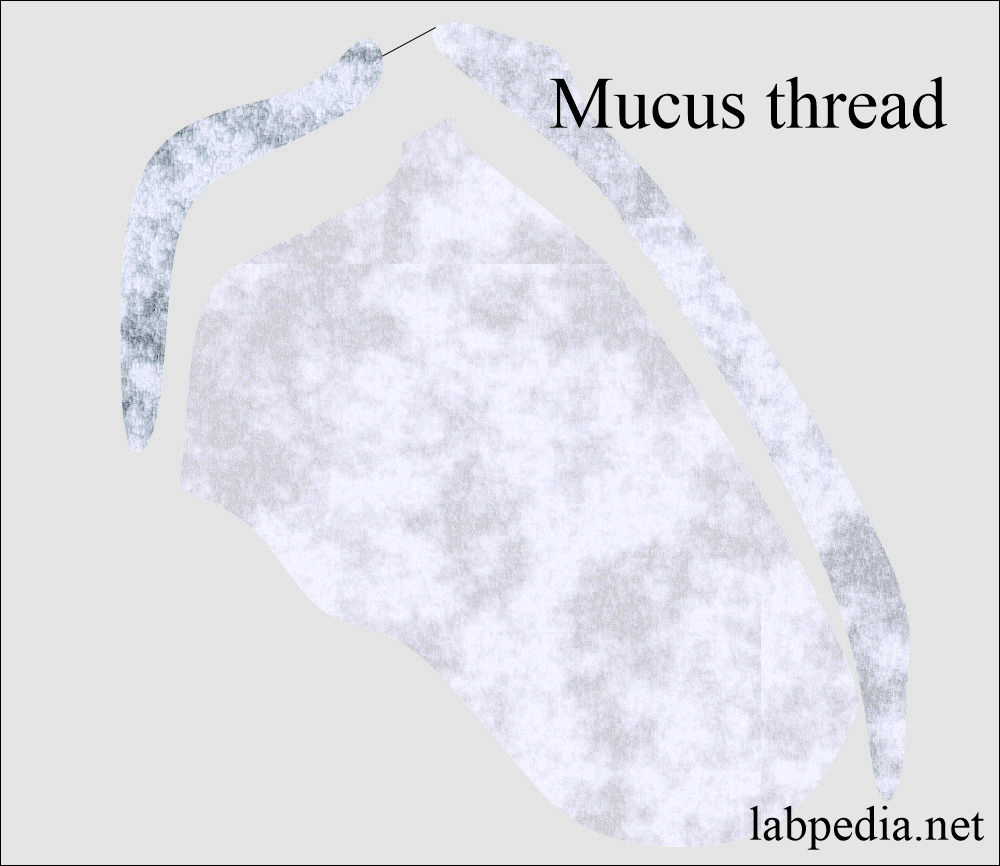
Mucous threads:
- Mucus is a protein produced by the glands and the epithelial and renal tubular cells of the lower genitourinary tract.
- The main component of the mucus is the Tamm Horsfall protein.
- These may be mistaken for hyaline casts.
- These are long threads, undefined edges, and pointed or irregular ends.
- Mucus has a low refractive index.
- Mucus threads are reported as:
- Rare.
- Few.
- Moderate.
- Many or abundant.
- It has no clinical significance in males or females.
Questions and answers:
Question 1: What is the significance of the trichomonas in the urine?
Question 2: What is the significance of RBC cast?
Please see more details in Urine Analysis Part 1.