Urine Analysis:- Part 3 – Urine Physical Examination and Interpretations
Urine Physical Examination and Interpretations
What sample is needed for urine analysis?
- Physical examination can be done on the random urine sample.
- You can keep the urine in the fridge for a few hours.
What are the precautions for urine physical examination?
- The doctor is advised to examine the urine as soon as possible.
- Urine must be analyzed within one hour of collection if held at room temperature.
- Keep urine at 2 to 8°C if delayed >8 hours.
- If urine is kept longer, it will get a false positive test, like nitrite, which will be positive.
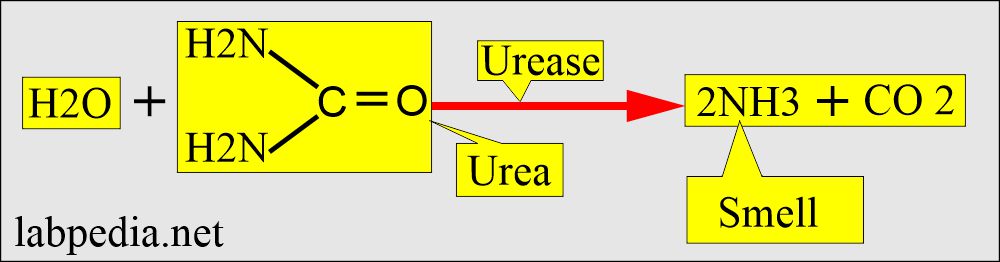
- Urea-producing organisms will degrade urea to ammonia and change the pH to alkaline.
- Change in pH causes degeneration of cast and cell lysis.
What is included in routine urine examination?
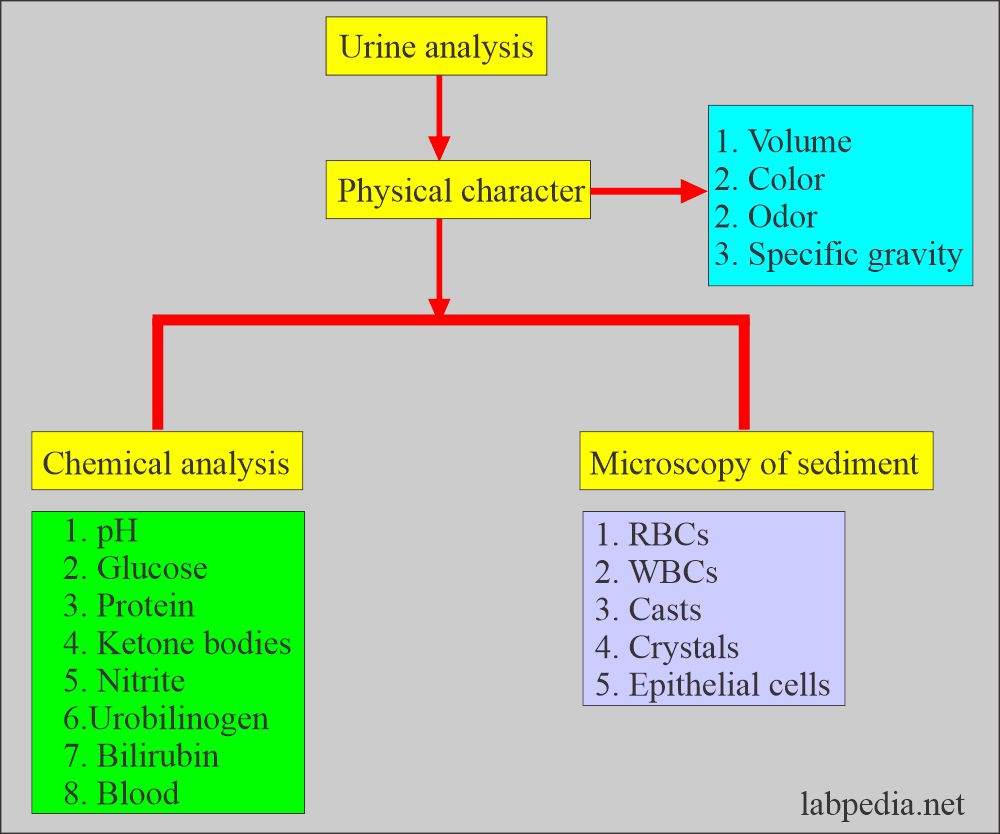
- Routine urinalysis includes:
- Physical character.
- Chemical analysis.
- Microscopic examination.
What factors interfere with urine analysis?
- What foods will color the urine?
- Carrots will change their urine color to dark yellow.
- Beets may cause red color urine.
- Rhubarb will change its color to red or brown.
- Asparagus produces a typical urine odor.
- If you keep urine on the table, bacteria will change its pH, making it alkaline because of urea-splitting bacteria, and ammonia will be produced.
- What is the effect of the various factors on the urine pH?
- Eating citrus fruits, dairy products, and vegetables makes urine alkaline.
- A high protein diet and some foods (cranberries) make urine acidic.
- A high protein, a fat diet without the intake of carbohydrates also causes ketonuria.
- When radiopaque contrast media is given to the patient, it will give false-positive urine protein for at least 3 days.
- Females may have contamination from the vaginal secretions and show an increased number of WBCs.
- Traumatic catheterization may cause hematuria and false RBCs in the urine.
- Vaginal secretions contamination may cause false-positive leucocyte esterase.
- False proteinuria is seen when urine is contaminated with vaginal secretions.
- Urine culture gives false-positive results when contaminated with stool, vaginal secretions, and contaminated test tubes or hands and clothes.
Urine Physical examination:
Color:
What are the factors that influence the color of urine?
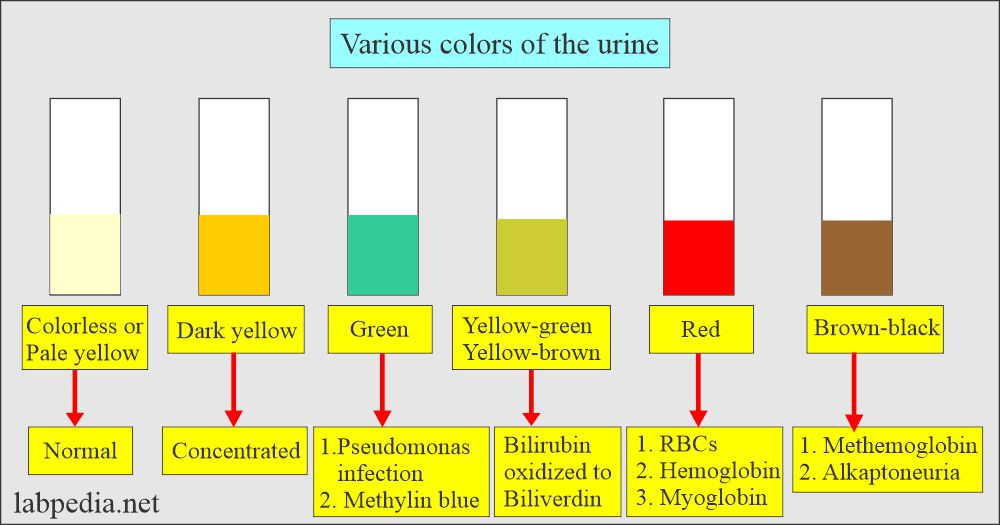
- The color of the urine varies from colorless to black.
- This variation in the color depends upon the following:
- Metabolic functions.
- Physical activity.
- Ingested food.
- Pathologic conditions.
- Any change in the color needs to be worked up to find the cause.
- The yellow color of the urine is due to pigment, which is called urochrome and is produced as endogenous metabolism.
- Color intensity depends upon the concentration of the urine.
- Concentrated urine is darker in color.
- The pale yellow to light color is due to diluted urine.
- The Yellow to amber color is due to urochromes, derivatives of urobilin, the end product of bilirubin degradation.
- Yellowish-brown to green color is due to bile pigment oxidation.
- While the blue/green color is due to pseudomonas infection.
- Blue urine color is due to the intake of medication of methocarbamol, methylene blue, and amitryptiline.
- Red and brown after standing are due to porphyrins.
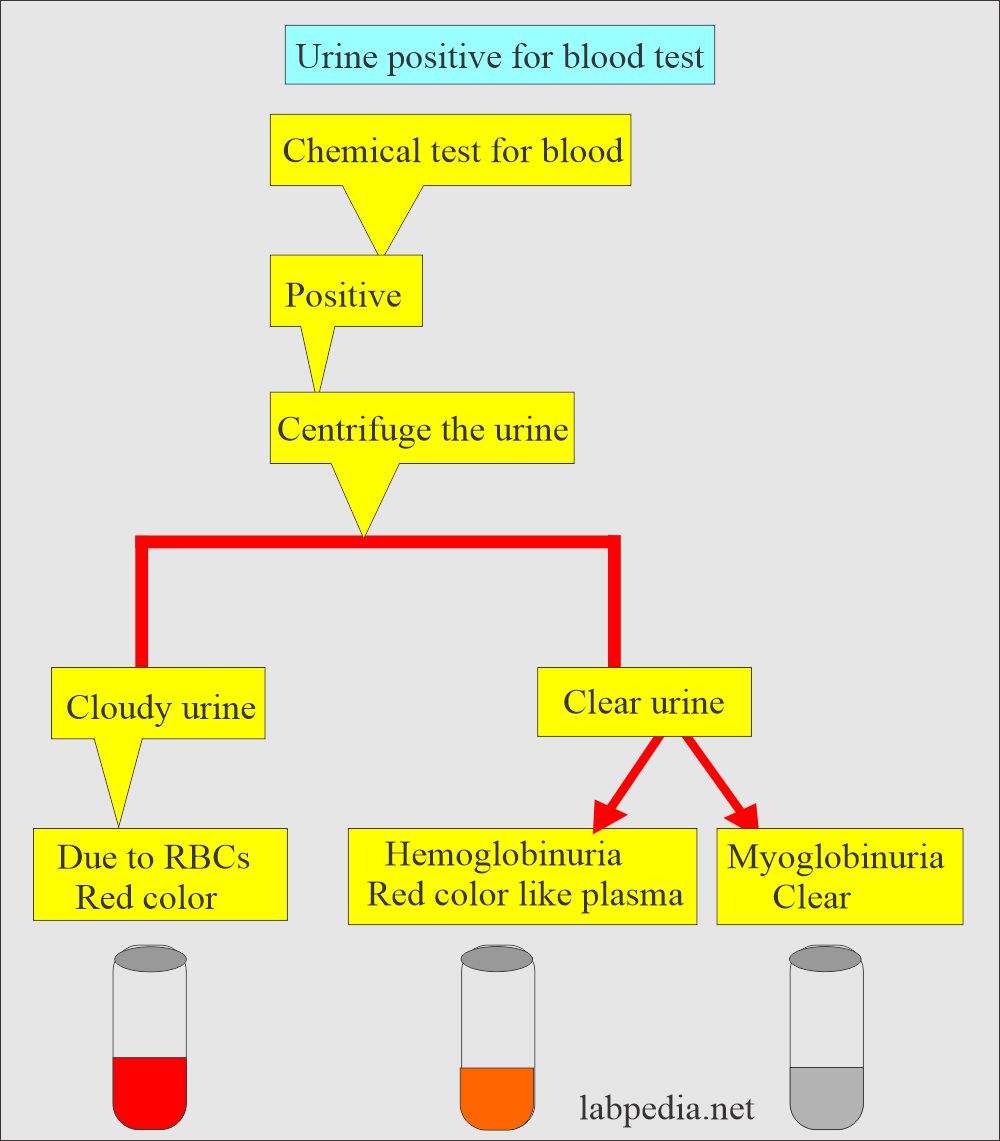
- The reddish-brown color in the fresh sample is from hemoglobin and red blood cells.
- When RBCs are present for several hours in acidic urine, they turn brown due to the oxidation of the methemoglobin.
- Hemoglobinuria shows red plasma due to hemolysis of the RBCs.
- Myoglobin is cleared from the plasma rapidly so that the plasma will be clear.
- Urine is positive for blood by chemical tests, and the brownish-black color on standing in the urine is due to alkaptonuria because of the homogentisic acid excretion. In this case, the chemical blood tests will be negative.
- In the case of malignant melanoma, melanogen oxidizes in the air to melanin.
- Drugs and some foods like beets may change the urine color.
- If urine shows large foam on shaking, it indicates increased protein in the urine.
What are the possible variations in the urine color?
| Urine color | Etiology for the color |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What drugs change the color of the urine?
| Drugs | Effect of the Drug on the Body | Change in the urine color |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the changes due to pathological and nonpathological conditions?
| Urine color | Pathological causes | Nonpathological causes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the causes of various colors of the urine?
Odor:
What are the factors that influence the odor of the urine?
- This is not part of the urine analysis. It has no clinical significance.
- Odor has little value in the diagnosis of various possibilities.
- There is a typical ammonia smell.
- When urine is sometimes kept on the table, ammonia (NH 3) odor becomes more prominent.
- The breakdown of the urea by the bacteria in the urine is responsible for the ammonia smell.
- The characteristic pungent odor in fresh urine is due to volatile aromatic acids.
- Urinary tract infection gives a noxious, fecal smell, and it is unpleasant to smell.
- Diabetic urine often smells fruity as a result of ketones.
- Ingestion of onions, garlic, and asparagus can cause an unusual or pungent odor.
- Maple syrup odor is seen in maple syrup disease.
- A bleach-like smell is seen in the contamination.
- The mousy odor is seen in phenylketonuria.
What are the causes of the urine odors?
| Odor | The reason for that odor |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Clarity:
What are the factors influencing urine clarity?
- Normal urine is clear and is judged against the light source.
- The cloudiness of the urine specimen depends on pH and dissolved solids components like amorphous phosphates and carbonates.
What are the types of urine clarity?
| Urine degree of clarity (cloudiness) |
Criteria |
|
|
|
|
|
|
|
|
Turbidity:
What are the factors influencing urine turbidity?
- It is generally due to gross bacteriuria.
- In alkaline urine, turbidity is due to amorphous phosphates and carbonates.
- In acidic urine, turbidity is due to amorphous urates.
- Smoky urine is due to hematuria.
- In women, the epithelial cells and mucus may result in hazy urine.
- Urine, when kept in the fridge, may become turbid without any pathology.
- Amorphous phosphates, carbonates, and urates in refrigerated urine give rise to thick turbidity.
- Other turbidity causes are contamination with semen, feces, vaginal cream, talcum powder, and contrast media.
- Turbidity may be seen in bacterial infection and the presence of RBCs and WBCs.
What are the common causes of urine turbidity?
| Normal causes | Pathologic causes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the causes of urine turbidity?
| The Effects on the Turbidity of Urine | Possible cause of the turbidity |
|
|
|
|
|
|
|
|
|
|
|
|
Specific gravity in urine:
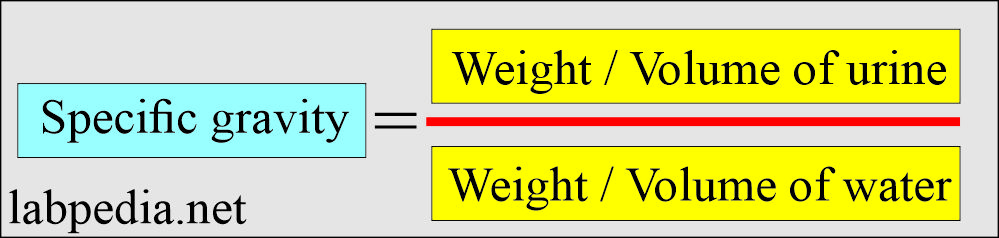
- One of the most important body functions is the kidneys’ ability to selectively absorb essential chemicals (electrolytes) and water from the glomerular filtrate.
- When the specific gravity is <1.003, it is mostly not urine.
How will you define specific gravity?
- This is the weight of 1 mL of urine in grams divided by 1 mL of water.
- This helps to give the state of hydration and dehydration.
- This indicates the kidney’s ability to concentrate.
- How will you measure urine-specific gravity?
- The specific gravity of the urine can be measured by:
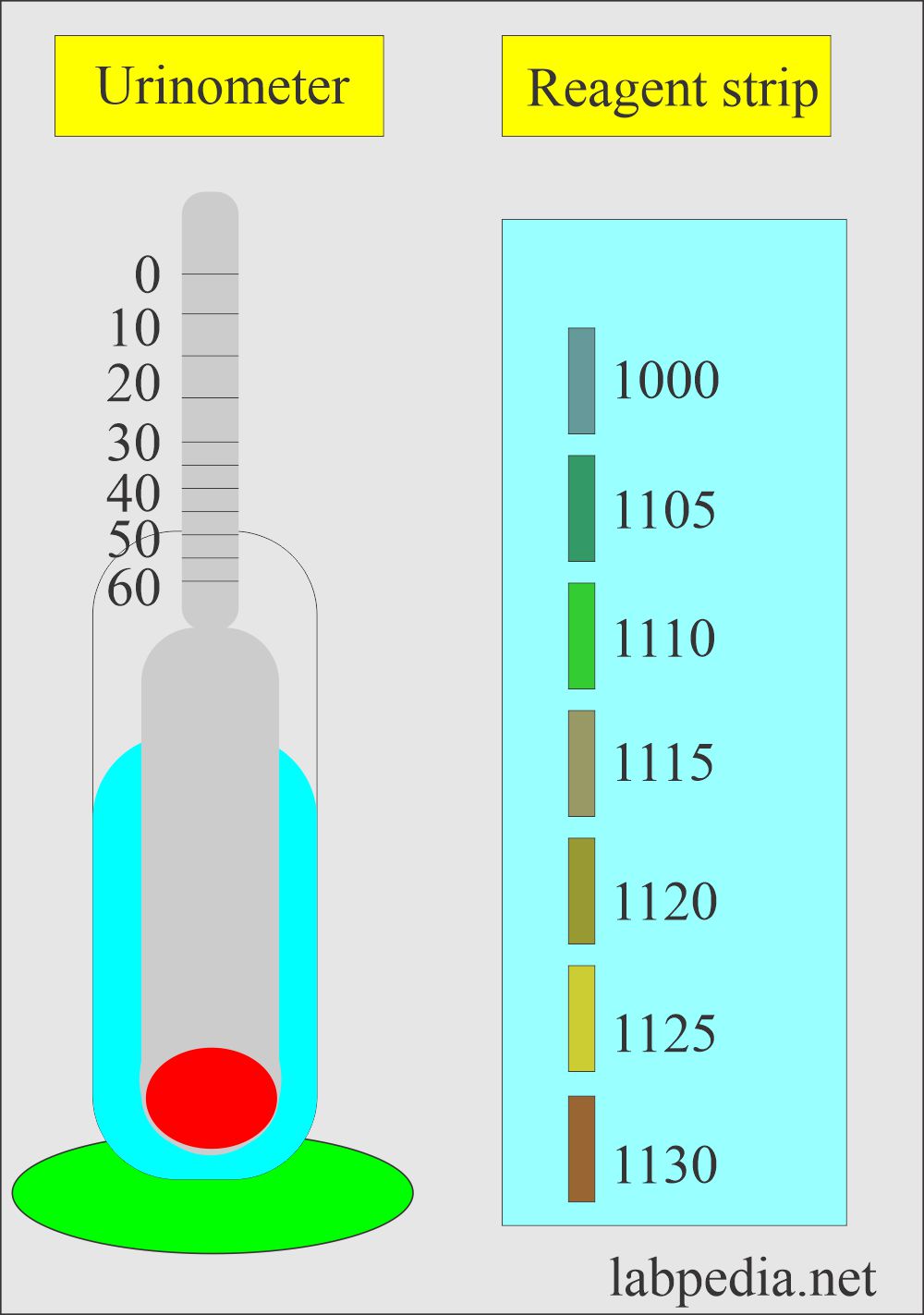
- Urinometer (hydrometer):
- This consists of a weighted float attached to the scale that has been calibrated to urine-specific gravity.
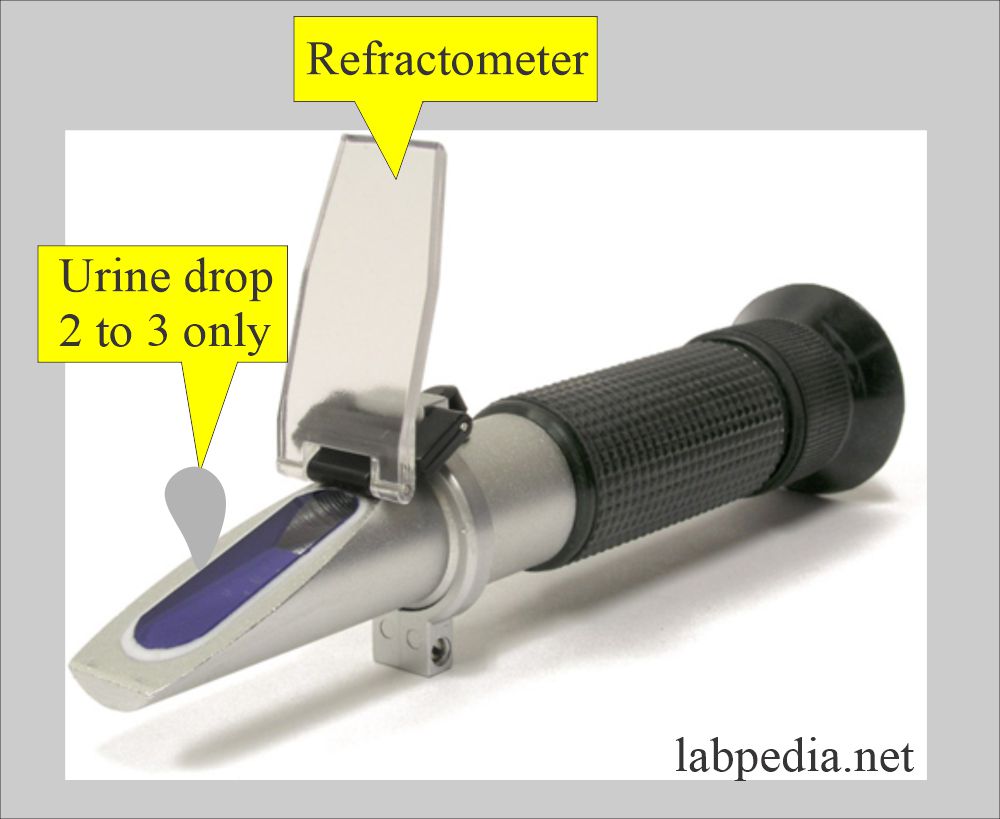
- Refractometer:
- This will determine the concentration of the dissolved particles in the urine by measuring the refractive index. This index compares the velocity of light in air with the velocity of light in the solution.
- The refractometer’s advantage is that it needs two or three drops of urine.
- Chemical reagents strips:
- These are disposable colorimetric reagent strips. No instrument is needed.
- Automated instruments.
What is the normal urine specific gravity?
- 1.003 to 1.030 (1.005 to 1.030).
- Most urine falls in the range of 1.015 to 1.025.
- Newborn = 1.012
- Infants = 1.002 to 1.006
- Adult = 1.002 to 1.030
- After 12 hours of fluid restriction = >1.025
- Urine 24 hours = 1.015 to 1.025
- The diluted urine range is 1.000 to 1.010.
- Concentrated urine is 1.025 to 1.030.
What are the causes of Low specific gravity of urine (hyposthenuria)?
- Diabetes inspidus (not go above 1.001 to 1.003. There is a lake of ADH hormone.
- Pyelonephritis.
- Glomerulonephritis.
- The consistently low specific gravity of 1.010 is known as isosthenuria. It is seen in chronic renal disease, where the capacity to concentrate urine is lost.
What are the causes of High specific gravity urine (hypersthenuria)?
- Diabetes mellitus.
- Congestive heart failure.
- Dehydration due to sweating, fever, vomiting, or diarrhea.
- Adrenal insufficiency.
- Liver disease.Nephrosis.
Urine pH:
What is the controlling mechanism of urine-specific gravity?
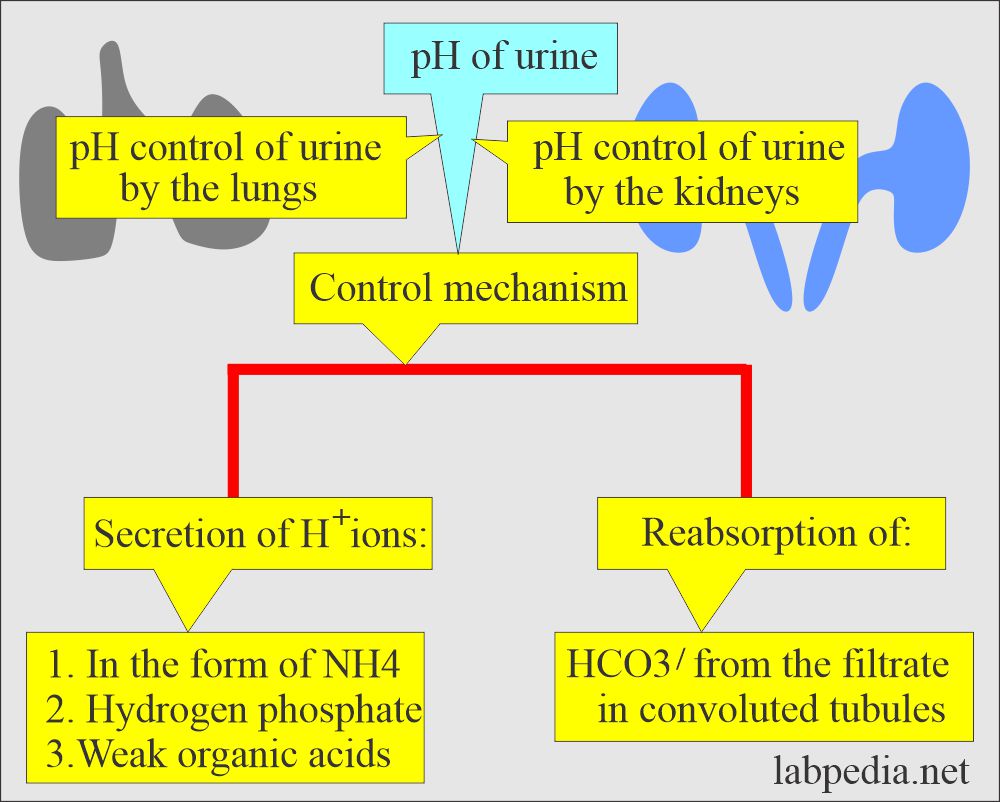
- The lungs and the kidneys are major regulators of the body’s acid-base balance.
- These two organs control the pH by secreting hydrogen ions in the form of ammonium ions, hydrogen phosphate, and weak organic acids.
- These organs can maintain the pH by reabsorption of HCO3– from the filtrate in the convoluted tubules.
- Urine pH must be measured on a fresh sample because urine tends to change pH when standing.
- The first-morning sample shows a pH of 5 to 6.
- After the meal pH may be alkaline.
- Urine pH is 4.6 to 7.0, and the average is 6.0
- pH depends upon the diet.
- pH <7.0 is primarily caused by the phosphates, which are excreted as salts conjugated to Na+, K+, Ca+, and NH4+.
- Acidity also reflects the excretion of nonvolatile metabolic acids pyruvate, lactate, and citrate.
- The acidity of urine (<7.0) is seen in the following:
- Systemic acidosis in diabetes mellitus.
- Renal tubular acidosis.
- The alkaline urine (>7.0) is seen in:
- This is a normal reaction to gastric acidity (HCL) dumped into the duodenum and then into circulation.
- Urinary tract infection.
- Bacterial contamination of the urine.
- Medications like sodium citrate and sodium bicarbonate will reduce pH.
- Fanconi’s syndrome is congenital generalized aminoaciduria due to defective proximal tubular dysfunction.
What are the causes of acidic and alkaline urine?
| Alkaline urine (pH is alkaline) | Acidic urine (pH is acidic) |
|
|
Osmolality and Osmolarity of urine:
How will you define osmolality?
- Specific gravity depends on the number of particles in a solution and the particles’ density, whereas osmolarity is affected only by the number of particles present.
- Osmolarity is the number of solute particles in one liter of the solvent.
- Osmolality is the number of solute particles in one Kg of solvent.
- The unit of osmolarity is Osm/L.
- The difference in the dilute solution is negligible.
- Osmolality is preferred over osmolarity because it is higher.
- When evaluating the ability of kidneys concentration, Na+, K+, and Urea are important. All these three contribute to the osmolarity of the urine.
- Example: Osmolal solution of the Glucose is 180 g dissolved in 1 Kg of solvent.
- The osmolar solution of glucose is 180 g dissolved in 1 Liter of solvent.
- The unit used in the laboratory is mOsm (milliosmole).
- What is the use of the osmolality/osmolarity?
- It can monitor renal concentration ability for the course of renal disease.
- It can monitor fluid and electrolyte therapy.
- It can differentiate between hypernatremia and hyponatremia.
- It evaluates the secretion and renal response to ADH.
- There is a need to get the osmolarity of the serum and the urine.
What is the normal osmolality and osmolarity?
- Urine osmolality = 300 to 900 mOsm/kg H2O (depending on fluid intake).
- After 12 hours fluid restriction = At least 3 times the serum level. or >850 mOsm/Kg H2O (>850 mmol/Kg H2O)
- Newborn = 100 to 600 mOsm/Kg H2O (SI unit 100 to 600 mmol/Kg H2O)
- Children + 50 to 850 mOsm/Kg H2O (50 to 850 mmol/Kg H2O).
- Serum osmolarity = 275 to 300 mOsm/L.
- Urine osmolarity = 50 to 1400 mOsm/L.
The volume of the urine:
What are the factors that influences volume of the urine?
- The urine volume depends on the amount of water excreted by the kidneys.
- The volume of the urine depends upon the following:
- The fluid (water) intake.
- Fluid (water) loss from nonrenal sources.
- The amount of ADH secretion.
- Excretion of dissolved solids such as glucose or salts.
- The urine volume excreted indicates the balance between fluid ingestion and water loss from the lungs, sweat, and intestine.
What is the normal urine volume?
- 1200 to 1500 mL/24 hours.
- The 600 to 2000 mL/24 hours range may be considered normal.
- The average urine volume is 1200 ml.
- Night urine volume is usually less in amount.
- The ratio of day and night urine is 2: 1 to 4:1.
What are the type of urine volume?
- Nocturnal polyuria:
- There is increased urine at night. This may be seen in diabetes mellitus and diabetes inspidus.
- This may be seen as diuretics or the intake of tea, coffee, or alcohol, which will suppress the ADH.
- Polyuria is seen in:
- Diabetes mellitus.
- Diabetes inspidus.
- Chronic renal disease.
- In the case of acromegaly.
- In the case of myxedema.
- Oliguria:
- There is a decrease in the normal daily urine volume.
- Anuria or oliguria, where urine volume is <200 mL/day.
- This is seen in dehydration due to vomiting, diarrhea, perspiration, or severe burns.
- Nephritis.
- Urinary tract obstruction.
- Acute renal failure.
- Oliguria may lead to anuria.
- Drugs that have diuretic effects are:
- Thiazides.
- Alcohol.
- Caffeine.
- The drugs which decrease the volume and are nephrotoxic are:
- Analgesics like salicylates.
- Antibiotics like neomycin, penicillin, and streptomycin.
- There is a decrease in the normal daily urine volume.
What is the normal volume of the urine?
| Age | Normal volume |
| Newborn | |
| 1 to 2 days | 30 to 60 mL/24 hours |
| Infant | |
| 3 to 10 days | 100 to 300 mL/24 hours |
| 60 to 365 days | 400 to 500 mL/24 hours |
| Child | |
| 1 to 3 years | 500 to 600 mL/24 hours |
| 8 to 14 years | 800 o 1400 mL/24 hours |
| Adult | |
| Male | 800 to 1800 mL/24 hours |
| Female | 600 to 1600 mL/24 hours |
| Elderly | 250 to 2400 mL/24 hours |
Normal urine picture:
| Physical features | Chemical features | Microscopic findings |
|
|
|
Questions and answers:
Question 1: What is the difference between osmolality and osmolarity?
Question 2: What is the specific gravity to rule out that the sample is not urine?
Question 3: What is normal urine volume in infants of 1 to 2 days?
Note: Details are seen in Part 3, which is a complete urine analysis.

Really nice collection of tests
Loved it, using for my students
You are welcome.
dr. Dipak please see this link, https://www.labpedia.net/urine-analysis-part-3-complete-urine-analysis/
Thanks
thank you sir, great informative article for for every patient
Thank you.
This was incredibly helpful! It would be amazing and refreshing to have you as a professor! Thank you kindly for sharing your wisdom!!
Thanks for the beautiful words.
Thaks very machs Dr Dipak Gadade for the prife explination of urinalaysis physical exmination
Hello Doc, I’m 23 years old male. Id the results of my urinalysis okay?
Color: Light Yellow
Transparency: Slightly Turbid
pH: 6.0
Specific gravity: 1.005
Sugar:Negative
Protein: Negative
RBCs: None
PUS cells: 0.2/hpf
Squamos Ephitelial Cells: Rare
Mucus Threads: Moderate
Your urine report is normal. No need to worry.
Hello Dr. Riaz How are you doing. I was surfing around and ends up here. My question is where to gets Urine deposits atlas for medical student as well permanent/mounted/ fix slides to study and recognized the various diseases sedimentation for diagnosis and get practice under microscope. Appreciated very Much.
Please see this link:
https://labpedia.net/urine-analysis-complete-urine-analysis-discussion/
Please also see this link:
https://labpedia.net/urine-microscopic-examination-and-interpretations-part-2/
Please search urine analysis and see all these topics.