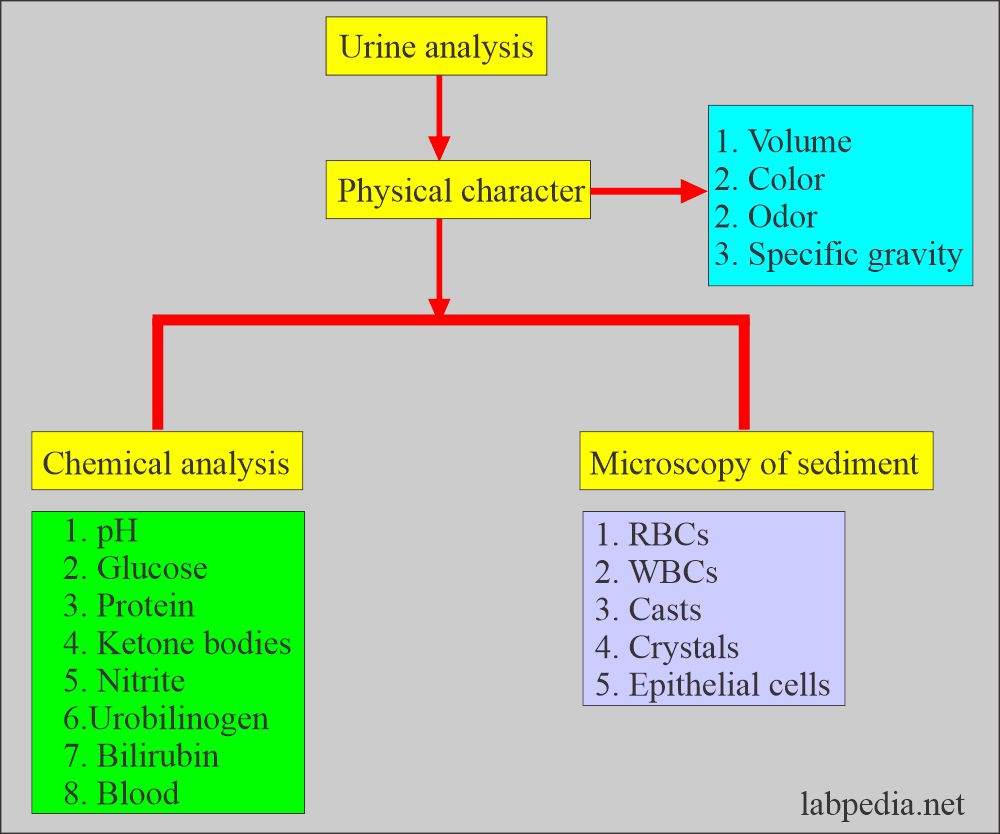
Urine Analysis:- Part 1 – Complete Urine Analysis Discussion
Urine Analysis
What samples are needed for urine analysis?
- The urine may be random or morning samples.
- Urine must be tested within 1 to 2 hours of collection.
- It may need 24 hours of urine collection.
What are the precautions for urine analysis?
- Urine can be refrigerated for 6 to 8 hours.
- At low temperatures, there will be precipitation of amorphous urates or phosphates.
- Bring the refrigerated urine to room temperature before testing.
- Urine collected for more than 2 hours may be rejected.
- The decomposition of urine begins in 30 minutes at room temperature and 4 hours in refrigeration.
- For longer periods, boric acid can be used as a preservative.
What factors will interfere with the urine analysis results?
- Certain foods will color the urine, like:
- Carrots will change their urine color to dark yellow.
- Beets may cause red color urine.
- Rhubarb will change its color to red or brown.
- Asparagus produces a typical urine odor.
- If you keep urine on the table, bacteria will change its pH, making it alkaline because of urea-splitting bacteria, and ammonia will be produced.
- Effect of the food on the urine pH:
- Eating citrus fruits, dairy products, and vegetables makes urine alkaline.
- A high protein diet and some foods (cranberries) make urine acidic.
- A high protein, a fat diet without the intake of carbohydrates also causes ketonuria.
- When radiopaque contrast media is given to the patient, it will give false-positive urine protein for at least 3 days.
- Females may have contamination from the vaginal secretions and show an increased number of WBCs.
- Traumatic catheterization may cause hematuria and false RBCs in the urine.
- Vaginal secretions contamination may cause false-positive leucocyte esterase.
- False proteinuria is seen when urine is contaminated with vaginal secretions.
- Urine culture gives false-positive results when contaminated with stool, vaginal secretions, and contaminated test tubes or hands and clothes.
Complete Urine Analysis
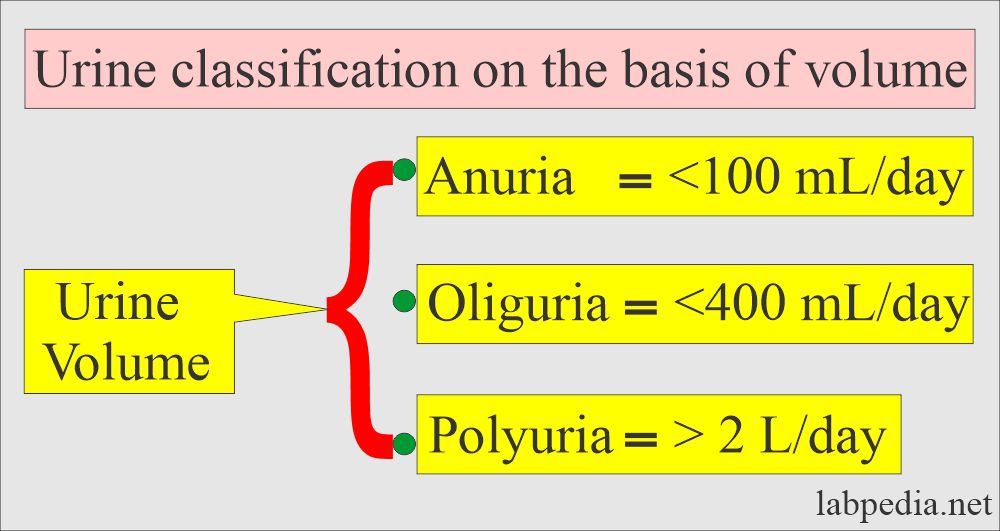
The volume of the urine
How much is the urine volume?
- It is 600 to 2500 ml /24 hours, and the average volume is 1200 ml/24 hours.
What is Polyuria?
- It occurs when urine amount exceeds 2000 mL/24 hours.
- This is seen in diabetes mellitus.
- In diabetes Insipidus.
- Excessive fluid intake.
- Drugs like diuretic therapy.
What is Oliguria?
- It is seen when urine volume is less than 500 mL/ 24 hours. This is seen in the following conditions.
- Renal tubular dysfunction.
- Edema.
- End-stage kidneys.
- Obstructive uropathy.
- Dehydration.
- Vomiting.
- Shock.
- Diarrhea.
What is Anuria?
- It occurs when there is no urine output. This is seen in the following conditions:
- Acute renal failure.
- Heart failure.
- Acute Glomerulonephritis.
- Obstructive uropathy.
- Shock.
How will you calculate urine output?
- Adult = >0.5 mL/Kg/hour.
- Child = >1 mL/Kg/hour.
- Neonate (< 1-year-old) = >2 mL/Kg/hour.
What factors will influence Urine volume?
- It varies according to age.
- Urine volume is 600 to 2500 mL/day; the average is 1200 mL/day.
- At night, urine volume is usually <700 mL and specific gravity is more than 1.018.
- The ratio of the night-to-day urine volume is 1:2 to 1:4.
- The range of 600 to 2000 mL/day is considered normal.
What is the urine volume in various age groups?
| Various groups | Various age groups | Normal volume per day |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
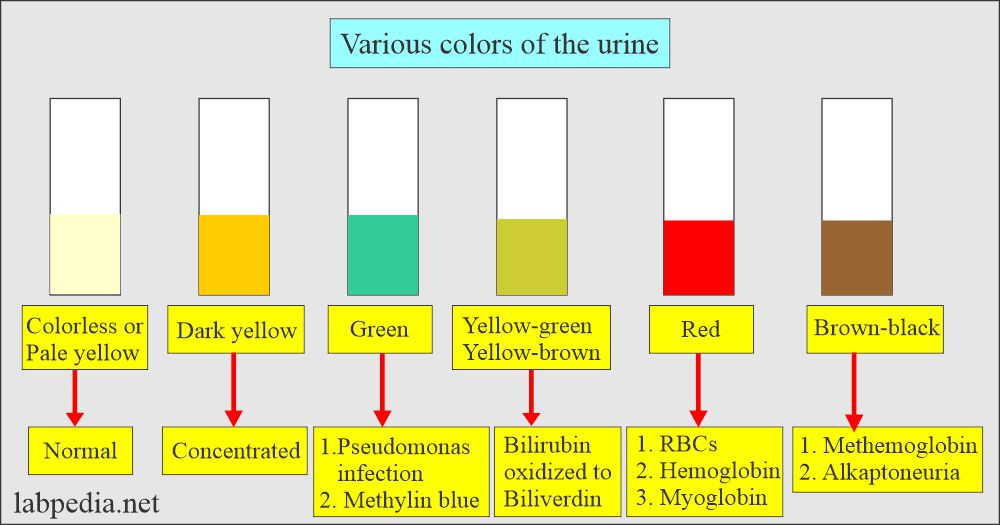
Color of the urine
What is the normal color of urine?
- The normal color is Pale to dark yellow.
What are the possibilities of abnormal Color?
- It may be due to some of the foods and medicines.
- Urine with no color may be caused by long-term kidney disease or uncontrolled diabetes.
- Dark yellow urine can be caused by dehydration.
- Red urine can be caused by blood in the urine.
- The Orange color is due to bilirubin.
- The dark yellow color may be seen due to bilirubin and urobilin.
- Brown and black may be due to melanin, homogentisic acid, and biliary pigments.
- Green-colored urine may be seen due to Biliverdin, pseudomonas infection, and oxidized bilirubin.
What are the causes of cloudy urine?
- Pus (white blood cells).
- Blood (red blood cells).
- Sperm, Bacteria, and yeast.
- Crystals.
- Mucus.
- Parasite infection, such as trichomoniasis.
What are the causes of red color urine?
- When clear, on standing, this will indicate the following:
- Hemoglobinuria.
- Myoglobinuria.
- When cloudy red urine indicates:
- Hematuria.
What are the possible colors of the urine?
| Color of the urine | Effect of the foods | Color change due to drugs | Medical causes for the color |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the drugs which change the color of the urine?
| Drugs | Effect of the Drug on the Body | Change in the urine color |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
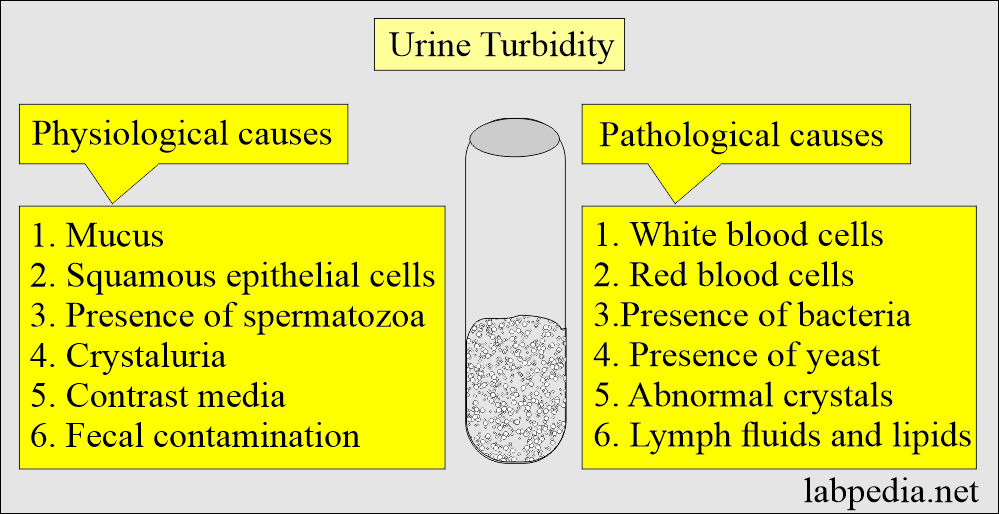
Clarity of the urine
How much is the clarity of urine?
- Normally, it is Clear. No visible particles are seen.
- Hazy urine is where there are few particulates, and print can be seen easily through urine.
- Cloudy when there are many particulates, and the print is blurred through urine.
- Turbid urine, when through urine print, cannot be seen.
- Milky where there are many particulates, and it may be clotted.
What is the urine turbidity?
- It is seen in nonpathological conditions like:
- With the presence of squamous epithelial cells.
- The presence of mucus.
- The presence of spermatozoa.
- Amorphous phosphates, urates, and carbonates.
- In the case of contrast media.
- In the case of fecal contamination.
What is the pathological urine turbidity?
- Urine turbidity is seen in pathological conditions like:
- White blood cells.
- Red blood cells.
- Presence of bacteria.
- Presence of yeast.
- Abnormal crystals.
- Lymph fluids and lipids.
What is the solubility of urine in various conditions?
| Solubility in various conditions | Substances/ chemicals solubilized |
|
|
|
|
|
|
|
|
|
|
|
|
- In Alkaline urine, amorphous phosphate and carbonates are seen.
- In acidic urine, amorphous urates and radiographic contrast media are seen.
- Soluble by heat are amorphous urates and uric acid crystals.
The odor of the urine
What is the odor of urine?
- The odor is not clinically significant. This is not part of the urine analysis.
- The odor is normally slightly “nutty” (faint, aromatic).
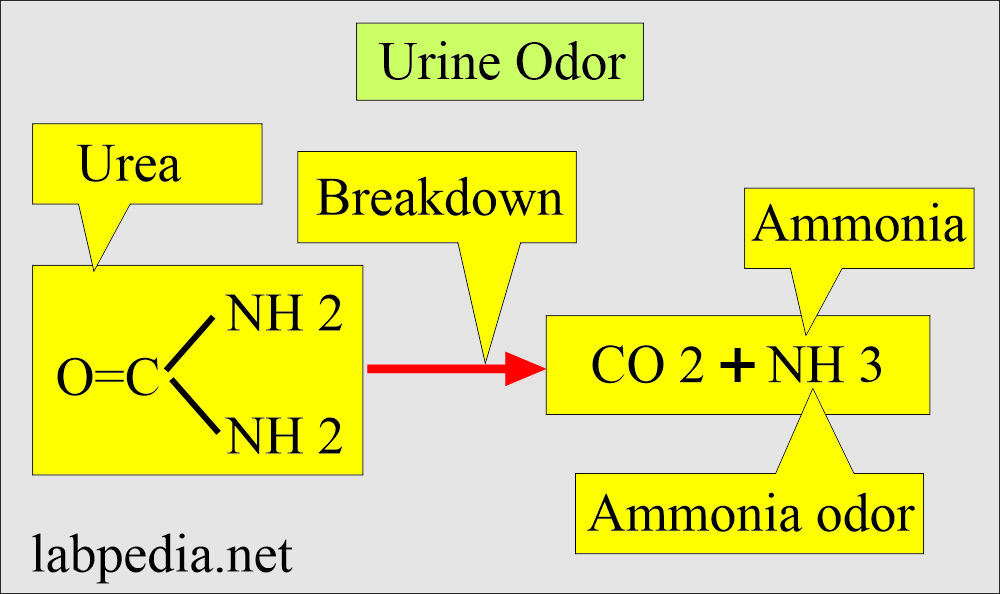
- When urine is kept, the ammonia odor is more prominent. This is because the urea is broken down.
What are the causes of abnormal Odors in the urine?
- Some foods, such as asparagus, onions, and garlic, cause a pungent odor.
- Vitamins and antibiotics (such as penicillin) can cause urine to have a different odor.
- A sweet, fruity odor may be caused by uncontrolled diabetes mellitus.
- A urinary tract infection (UTI) can cause an unpleasant odor.
- Urine that smells like maple syrup means maple syrup urine disease when the body cannot break down certain amino acids.
- Phenylketonuria gives a mousy smell.
- Bleach-like odor is due to contamination.
What are the various causes of the odor of urine?
| Various types of odor (smell) | Etiology of the odor |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The specific gravity of urine
What is the specific gravity of urine?
- One of the kidneys’ most important functions is the ability to selectively reabsorb essential chemicals and water from the glomerular filtrate.
- Bring the urine to room temperature to measure specific gravity if it is refrigerated.
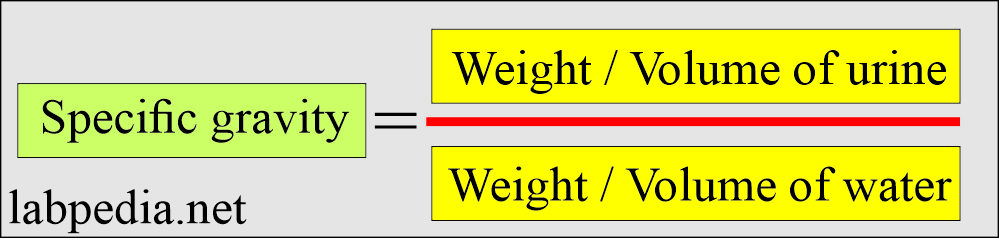
- Specific gravity is a substance’s density relative to distle water’s density.
- The normal range of urine specific gravity = 1.005 to 1.030
- The normal urine sample ranges between 1.010 to 1.025.
- Specific gravity is higher in the first-morning urine specimen (>1.020).
- The normal range of urine-specific gravity = 1.005 – 1.030.
- Neonates = 1.012.
- Infants = 1.002 to 1.006.
- Adults = 1.003 to 1.030.
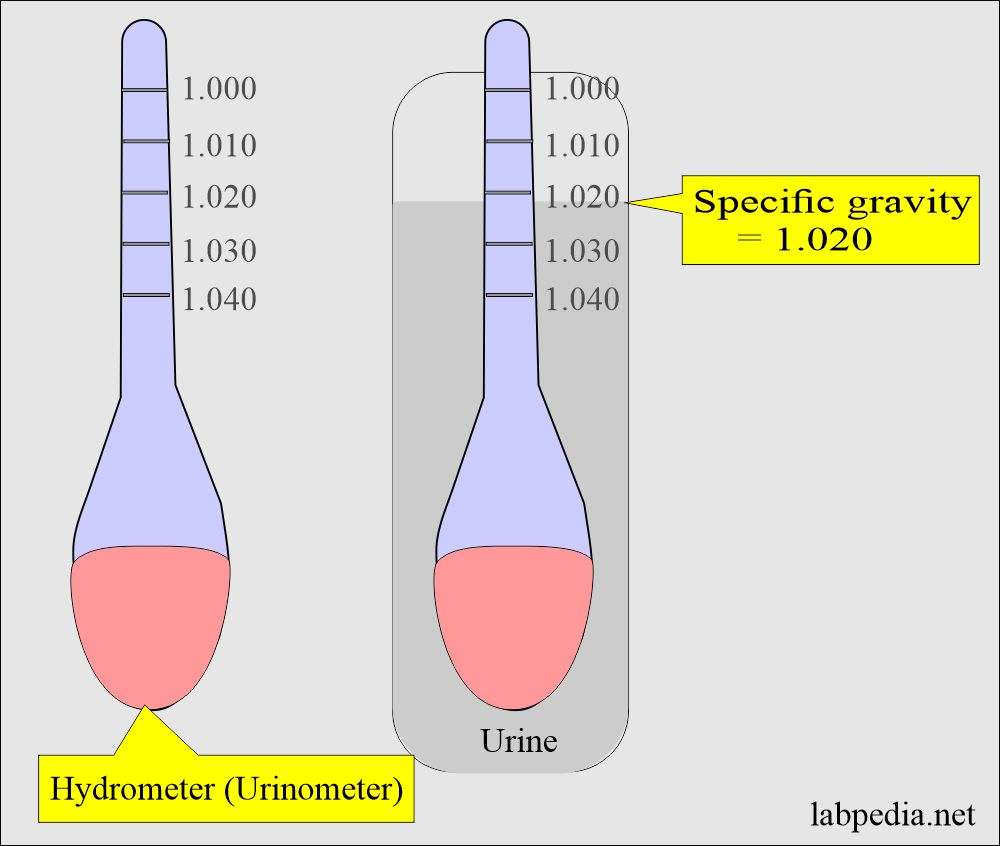
- The urinometer measures specific gravity.
- To check the urinometer’s reliability, put it into the water, which should read 1.000.
- It can be checked by using the known specific gravity solution.
What is the principle of a urine refractometer?
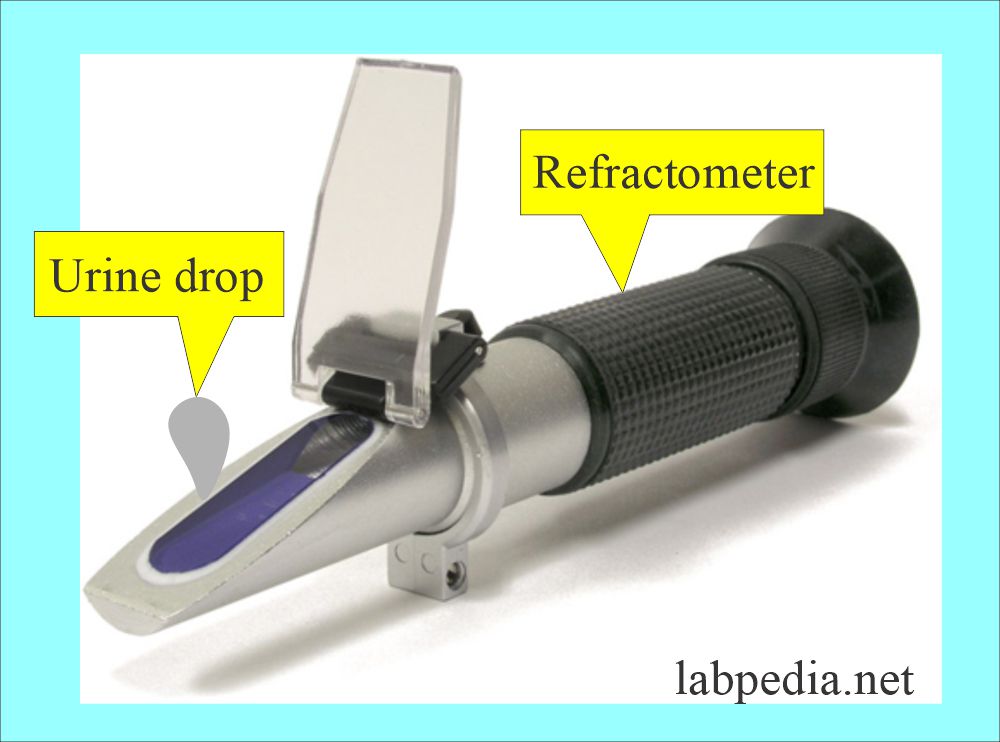
- It measures the refractive index of the urine.
- Its principle is that the refractive index compares the velocity of the light in air with the velocity of light in a solution.
- The concentration of dissolved particles in the solution will determine the velocity and angle at which light passes through it.
- The refractometer’s advantage is that it uses only 1 to 2 drops of urine when the urinometer needs more.
What are the causes of abnormal Specific Gravity?
| Types of specific gravity | Etiology or causes |
|
|
|
|
|
|
pH of the urine
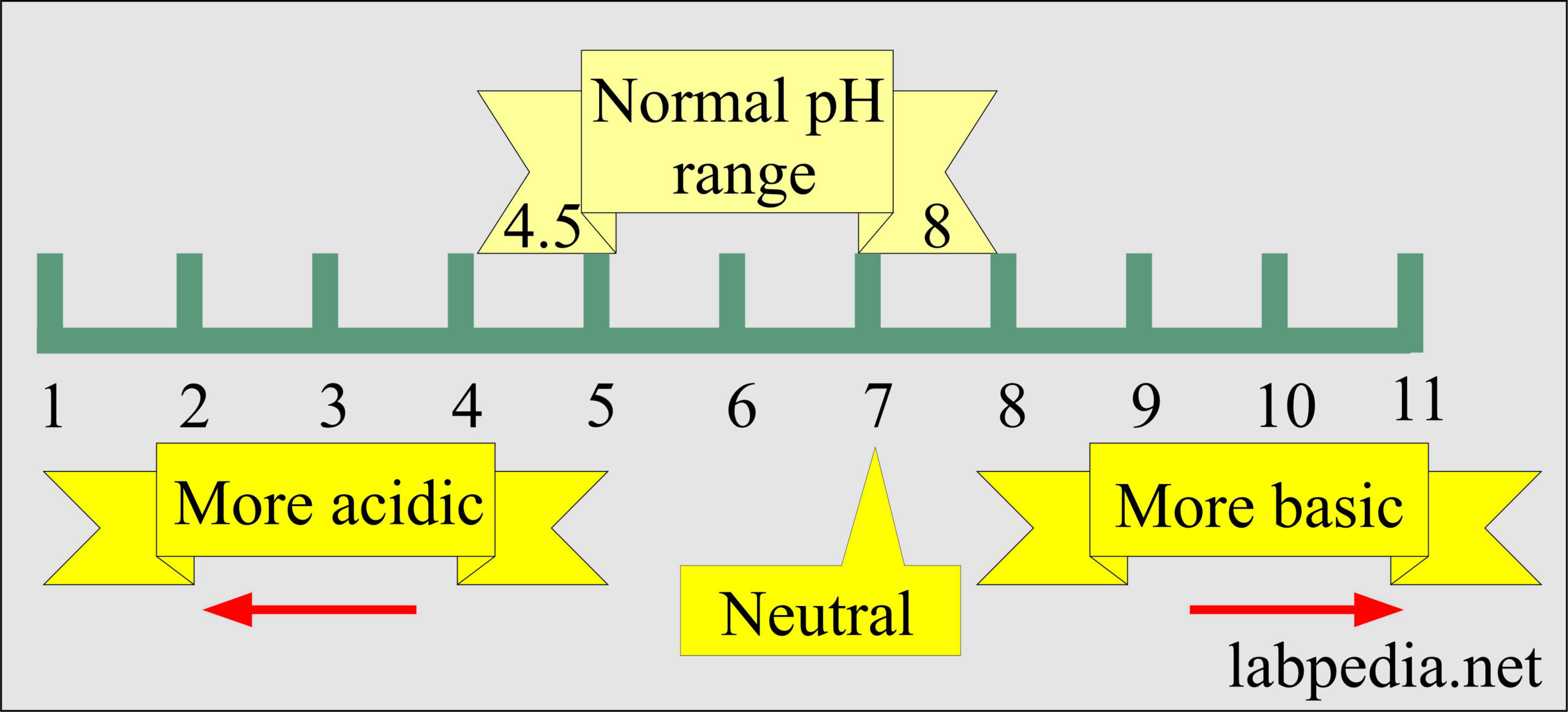
How will you define urine pH?
- Normal pH = 4.6 to 8.0.
- The average person has a pH of 5 to 6.
- pH is helpful for the identification of crystals.
- pH is helpful for the acid-base status.
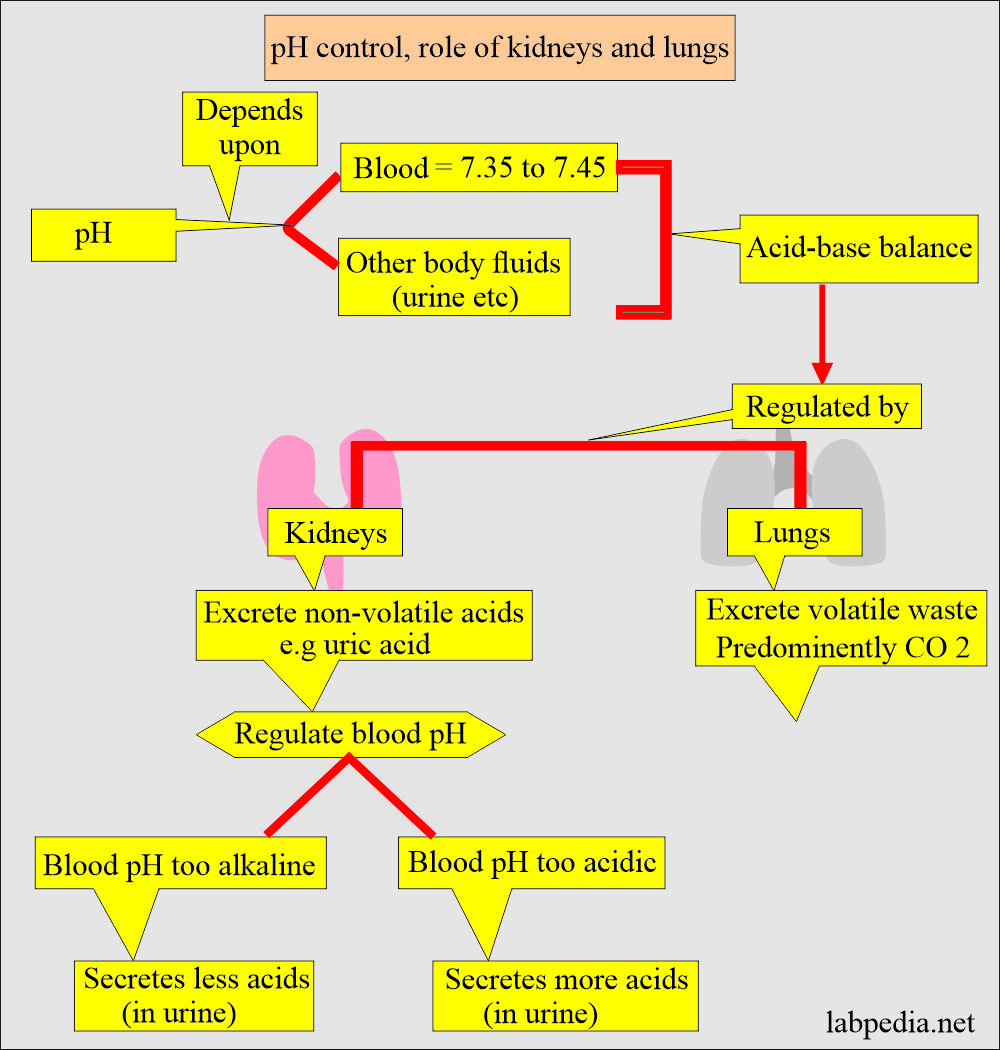
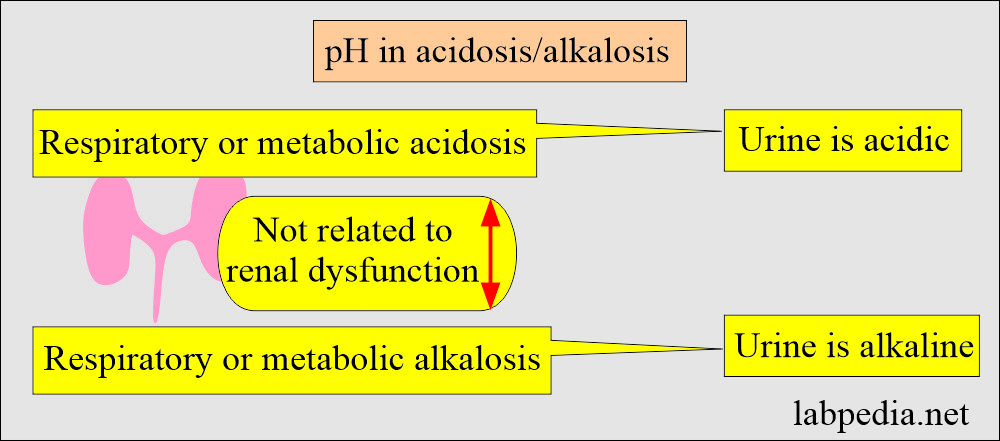
What are the factors affecting the urine pH?
- Acidic urine is produced in the following ways:
- High protein diet.
- Lung diseases occur when CO2 is retained in the body.
- Diabetes mellitus in uncontrolled diabetics.
- Alkaline urine is produced in the following ways:
- Urinary tract infection.
- Bacterial contamination of the urine.
- A diet high in vegetables, citrus fruits, or dairy products makes more alkaline urine.
- Hyperventilation and loss of CO2.
- When treated with NaHCO3 and K citrate and antibiotics in treating the urinary tract infection.
What are the causes of abnormal urine pH?
- Some foods (citrus fruit and dairy products) and medicines (such as antacids) can affect urine pH.
| The pH of the urine | Etiology (causes) |
|
|
|
|
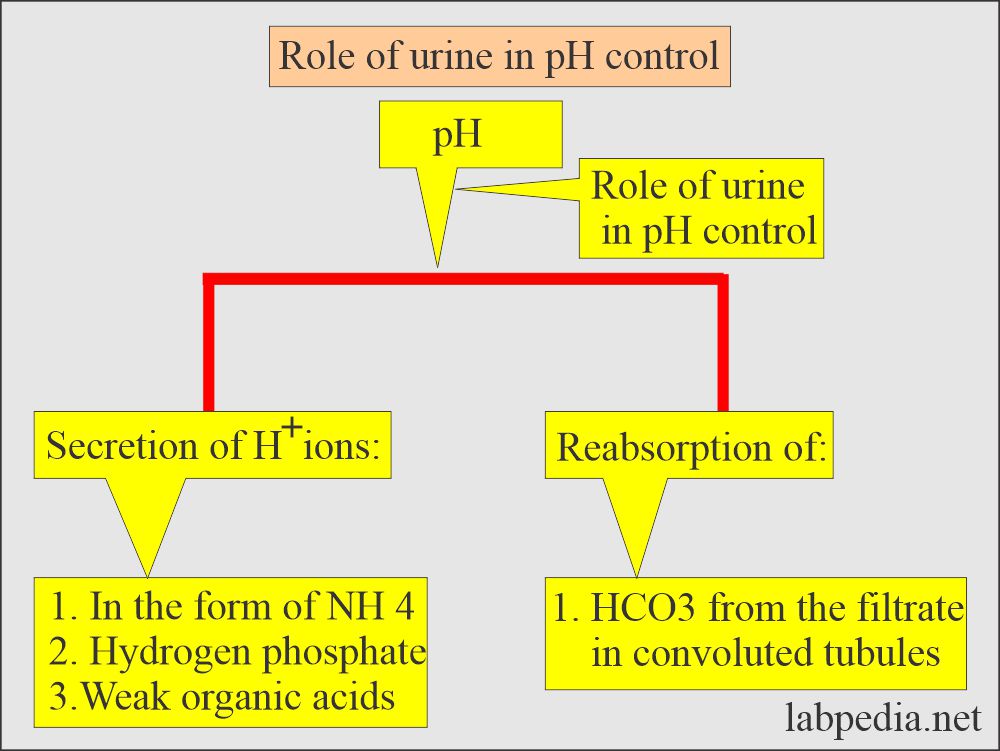
What is the significance of urine pH?
- Maintenance of acidic urine can be good for treating urinary tract infections caused by urea-splitting microbes because these bacteria can not grow in an acid medium.
- People on a high-protein diet produce acidic urine, and people on a vegetarian diet produce alkaline urine.
- The exception is cranberry produces acidic urine, and it can be used as a home remedy for urinary tract infections.
- Alkaline urine is seen in patients with renal calculi, made of calcium phosphate or magnesium-ammonium phosphate.
How will you measure urine pH?
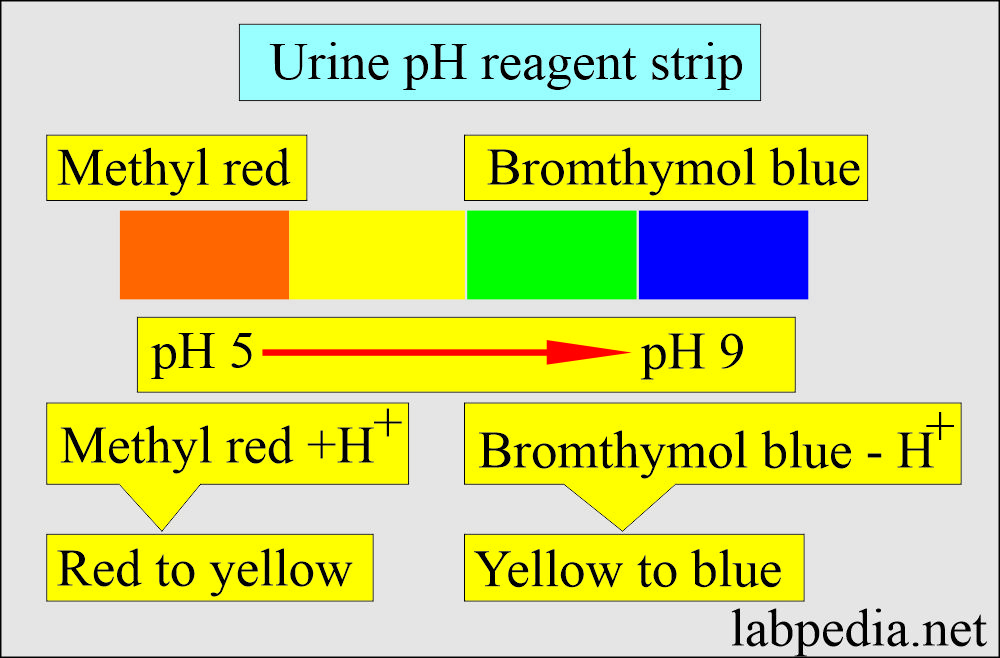
- There are various commercially available urine reagent strips to measure pH; these measure pH between 5 to 9.
- Indicators are methyl red and bromthymol blue.
- Methyl red changes color from red to yellow with a pH of 4 to 6.
- Bromthymol blue changes from yellow to blue with the change in pH from 6 to 9.
Protein in the urine
How will you define Proteins in the urine?
- Normally, urine is negative.
- It is <10 mg/dL or
- Around 100 mg/24 hours.
- The protein consists of primarily low molecular weight serum proteins filtered by the glomeruli.
- Albumin is the major protein found in normal urine.
- The tubules reabsorb the majority of the albumin.
- Proteinuria may be seen after vigorous exercise, dehydration, and fever.
- Benign proteinuria is postural and intermittent; this accounts for 5% of people.
How will you classify the proteinuria?
- Proteinuria may be classified based on the origin of the protein into:
What is the Prerenal proteinuria?
- This is not indicative of kidney disease.
- This is due to the increased low-molecular-weight plasma proteins such as hemoglobin, myoglobin, and acute-phase protein.
- Nonrenal diseases cause this and is transient; it is seen in:
- Hemoglobinuria.
- Myoglobinuria.
- Acute phase proteinuria.
- This is usually not detected by the routine urine reagent strips.
What is the Renal proteinuria?
- This is due to renal diseases involving glomeruli or tubules.
- In glomerular damage, selective filtration is impaired, and an increased amount of albumin, red blood cells, and white cells are excreted in the urine.
- It is seen in the following conditions:
- SLE.
- Streptococcal glomerulonephritis.
- Strenuous exercise (reversible condition).
- Pre-eclampsia and hypertension. (reversible condition).
- Toxic heavy metals.
- Severe viral infection.
- Microalbuminuria is seen in diabetic nephropathy, indicating kidney damage in diabetes mellitus.
What is the postrenal proteinuria?
- Proteins can be added as the urine passes through the ureter, urinary bladder, urethra, prostate, and vagina.
- Bacterial and fungal infection of the lower urinary tract,
- Menstrual contamination also contains proteins.
- Prostatic fluid and spermatozoa.
- Bacterial and fungal infections and inflammation produce exudate-containing protein from the interstitial fluids.
- Blood resulting from injury or menstrual contamination, prostatic fluid, and a large number of spermatozoa contribute to protein.
What is Orthostatic or postural proteinuria?
- This is a persistent benign condition frequently seen in young patients.
- It appears when the person is upright and disappears when the patient lies down.
- How do you check or confirm the diagnosis of orthostatic proteinuria?
- These patients are advised to empty their bladders before going to bed.
- Take the first urine sample when patients get up.
- Take another sample when patients are upright for several hours.
- The first sample will be negative, and the second will be positive in orthostatic proteinuria.
How will you discuss the Microalbuminuria?
- This is seen in diabetic nephropathy.
- This microalbuminuria indicates diabetic complications.
- The further complications of diabetes can be prevented by controlling diabetes.
- This is also associated with an increased risk of cardiovascular diseases.
- Microalbuminuria is reported as albumin excreted as µg/min or in mg/24 hours.
- The level is significant from 20 to 200 µg/min Or 30 to 300 mg/24 hours.
- In these cases, the albumin/creatinine ratio is >3.4 mg/mmol.
- The first-morning specimen is recommended.
What is the Bence Jones proteinuria?
- It is seen in multiple myeloma patients.
- These are monoclonal light-chain immunoglobulins.
- This is a low molecular weight protein and is excreted in the urine.
- How will you detect BJ protein?
- Heat the urine, and these proteins coagulate at 40 to 60 °C.
- Dissolve when the temperature reaches 100 °C.
- Reading the result: Urine turbid at 40 to 60 °C and clear at 100 °C is considered positive.
How will you summarize proteinuria?
| Type of proteinuria | Etiology of the proteinuria |
|
|
|
Glomerular disorders:
Tubular diseases:
|
|
|
What are the possible methods to detect proteinuria?
Please discuss the urine dipstick method?
- The urine dipstick reagents detect urine protein. This is a semiquantitative test.
- Trace positive reaction = 15 to 30 mg/dL.
- When 4+ positive reaction = 2.0 g/dL.
- Trace proteinuria = 10 to 30 mg/dL.
- 1+ = 30 mg/dL.
- 2+ = 100 mg/dL
- 3+ = 300 mg/dL
- 4+ = >1000 mg/dL
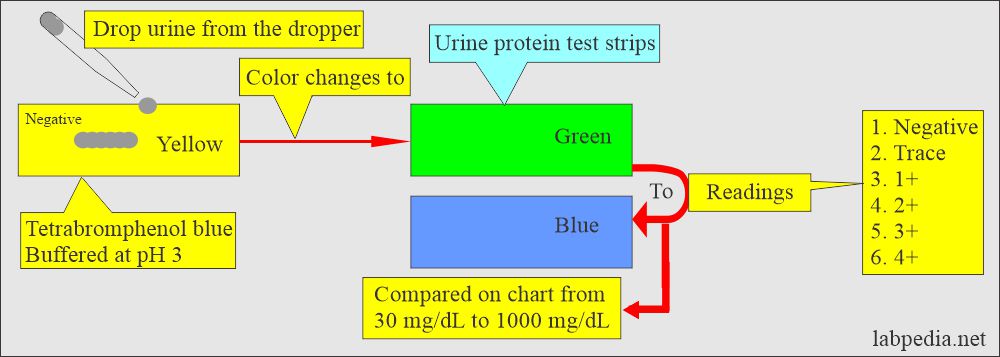
Urine protein reagent strips
How will you describe the sulfosalicylic acid method?
- It is a precipitation method.
- What is the sulfosalicylic acid Procedure?
- Transfer 3 mL of centrifuged urine into a test tube.
- Add 3 drops of sulfosalicylic acid (250 g/L) along the side of the test tube.
- The acid will form a layer underneath the urine.
- Do not mix, and let it remain for one minute.
- Reading:
- There is barely perceptible turbidity = reported as traces or ± (roughly 5 mg/dL).
- The heavier turbidity graded = 1+ to 4+.
- No turbidity = 0 mg/dL (<6 mg/dL)
- Slightly turbid = Traces, 20 mg/dL (6 to 30 mg/dL)
- 1+ = 50 mg/dL (Print visible through the specimen, 30 to 100 mg/dL).
- 2+ = 200 mg/dL (Print invisible, 100 to 200 mg/dL).
- 3+ = 500 mg/dL (Flocculation, 200 to 400 mg/dL).
- 4+ = >1000 mg/dL (Dense precipitate, >400 mg/dL).
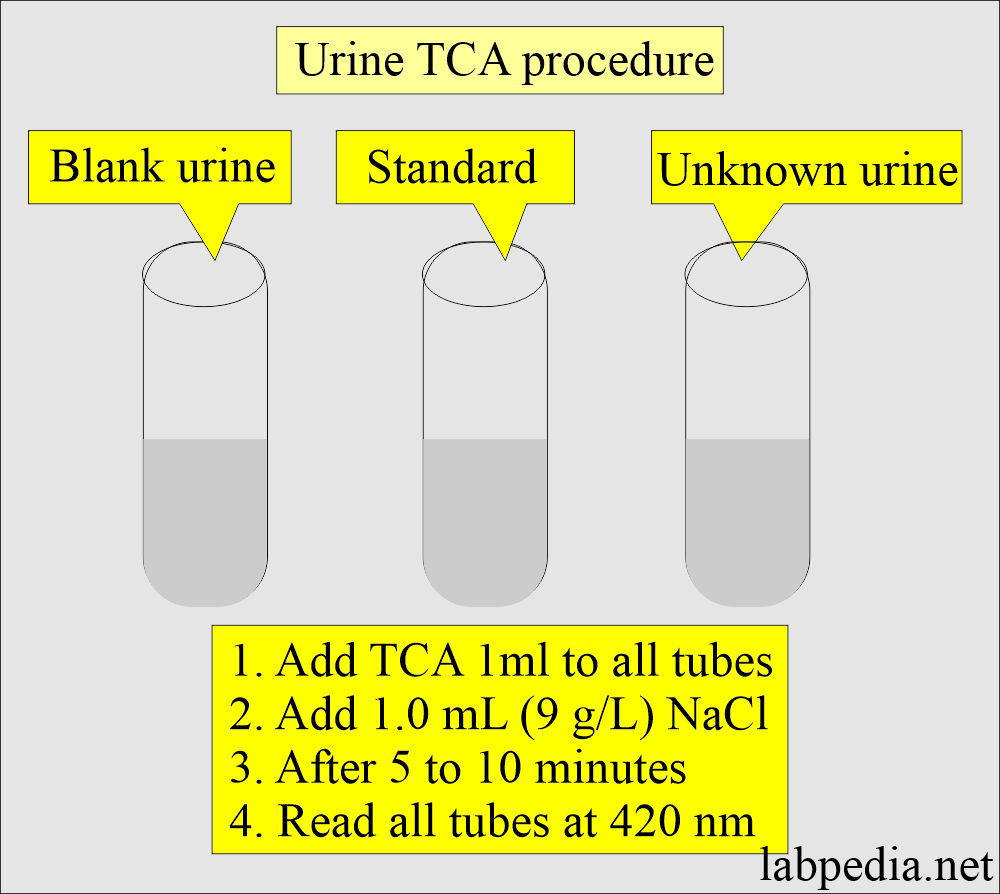
How would you describe Trichloroacetic acids (TCA)?
- This is also a precipitation method. This method is used in automation.
- TCA precipitates urine proteins as a fine suspension. The turbidity of the urine suspension is proportional to the amount of proteins in the urine.
- Procedure:
- Take TCA 12.5 g/dL.
- Dissolve it in the distle water and make up to 100 mL.
- Prepare the solution fresh every month.
- Make the standard protein solution in sodium chloride.
- Take the urine clear of the turbidity; if needed, you can centrifuge the urine.
- Take 4 mL of urine, 4 mL of the standard, and 4 ml of urine as blank.
- Add TCA 1.0 mL.
- Add 1.0 mL of NaCl (9 g/L) to all three test tubes.
- After 5 to 10 minutes, read all three tubes at 420 nm.
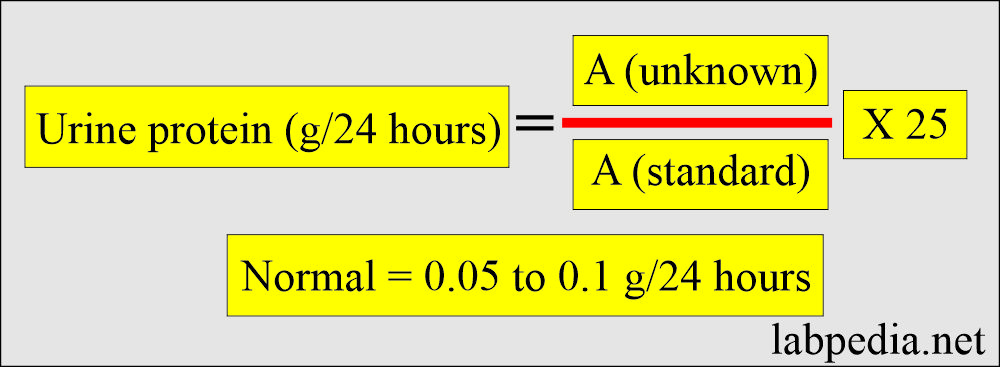
Calculation formula:
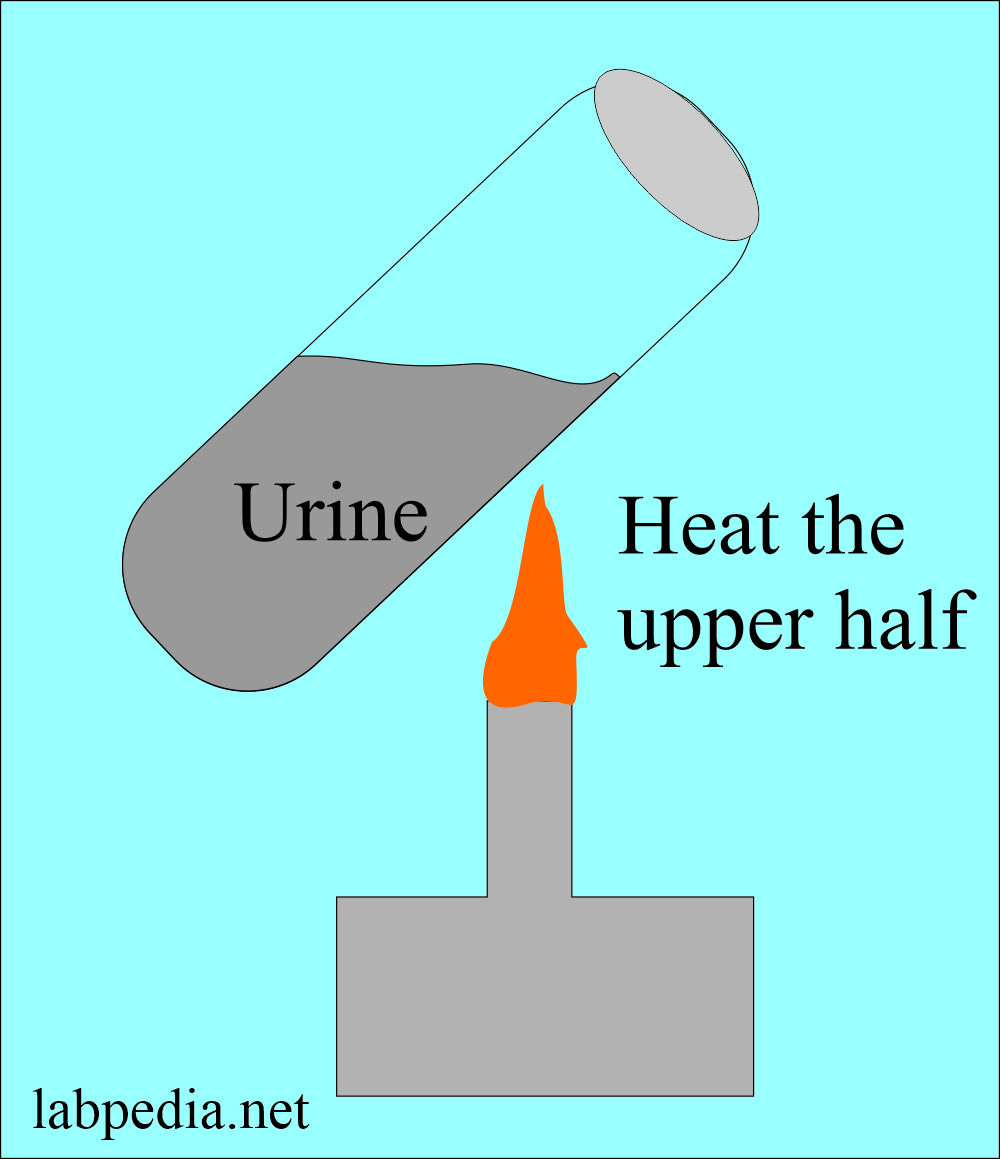
How would you perform the Heat coagulation test?
- Centrifuge the urine, and make urine clear.
- Take 7.5 mL of urine in a heat-resistant test tube.
- Add 3 drops of 5 M acetate buffer (pH 4.0 ).
- Make this buffer by mixing 24 ml of glacial acetic acid and 7.5 g of anhydrous sodium acetate in 100 ml of distle water and mixing well.
- Reading the result:
- If precipitate forms at this stage, it will indicate mucin (a mucoprotein).
- Centrifuge and remove this precipitate.
- Now heat the upper half of the urine and bring it to boiling.
- Now, examine for turbidity, comparing the upper half to the lower half.
- Hardly visible turbidity = 1+ (10 to 30mg/dL) or ±.
- Moderate turbidity = 2+ (40 to 100 mg/dL).
- Heavy turbidity = 3+ (200 to 500 mg/dL).
- A flocculant precipitate = 4+ (>500 mg/dL).
Orthostatic proteinuria
How will you test Postural (Orthostatic) proteinuria?
- Procedure:
- Ask the patient to empty the bladder before going to bed.
- Collect the urine immediately after getting up in the morning.
- Get a second sample after the patient is in the vertical position for several hours.
- Check the protein in both samples.
- Postural (Orthostatic) proteinuria-positive cases will show:
- First-morning sample = negative for urine proteins.
- The second sample = Positive for urine protein.
How will you grade proteinuria?
-
The degree of proteinuria Protein excreted per 24 hours - Mild
- <1.0 g /24 hours
- Moderate
- 1.0 to 3 or 4 g /24 hours
- Severe
- > 3 g / 24 hours
What are the various methods for proteinuria?
| Characteristics | Heat and acid | Reagent strip | Salfosalicylic acid |
|
|
|
|
|
|
||
|
|
|
Highly alkaline urine |
|
|
|
|
How will you classify proteinuria?
| Type of proteinuria | Amount of protein excreted in urine | Characteristic features |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the causes of Protein in the urine?
- Kidney damage.
- Infection.
- Cancer.
- High blood pressure.
- Diabetes.
- The Systemic lupus erythematosus (SLE).
- Glomerulonephritis.
- Heart failure.
- Leukemia.
- Poison (lead or mercury poisoning).
- High blood pressure during pregnancy (preeclampsia).
- Protein in the urine may mean :
- Kidney damage.
- Infection.
- Cancer.
- High blood pressure.
- Diabetes.
- The Systemic lupus erythematosus (SLE).
- Glomerulonephritis.
- Heart failure.
- Leukemia.
- Poison (lead or mercury poisoning).
- High blood pressure during pregnancy (preeclampsia).
- Proteinuria can be classified into different grades according to the amount of protein in the urine.
What is Beta-2-Microglobulin?
- It is structurally related to Immunoglobulin. It is used to differentiate Glomerular from tubular dysfunction.
Glucose in the urine
How will you define glucose in the urine?
- The healthy individual has a blood glucose of 100 mg/dL or less.
- This condition may be benign due to emotional stress or ingesting a large meal.
- When due to a pathological condition, then it is seen in diabetes.
- Normally, urine is negative.
- Urine glucose is detected by:
- The dipstick.
- The copper sulfate method (Clinitest).
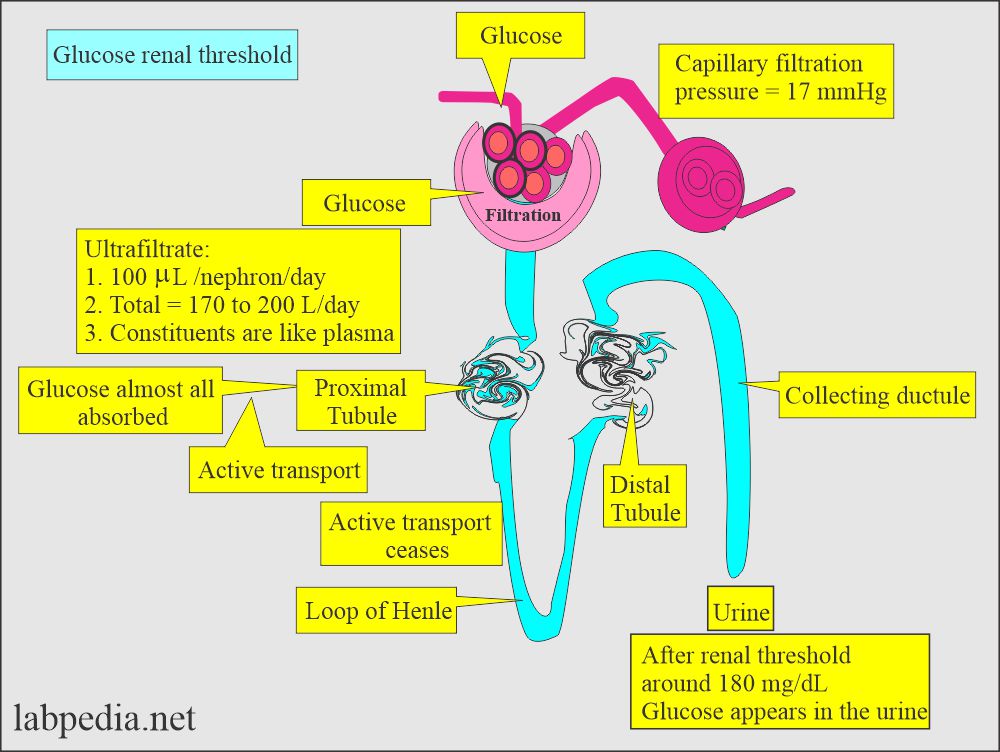
- Under normal circumstances, almost all glucose filtered by the glomerulus is reabsorbed in the proximal convoluted tubules.
What is the renal threshold of glucose?
- The level at which the tubular reabsorption is stopped for glucose is 160 to 180 mg/dL, called the renal threshold. But mostly,
it is considered around 180 mg/dL.
- The main function of insulin is to convert glucose to glycogen for storage (glycogenesis).
- The opposing hormone causes glycogen to break down into glucose (glycogenolysis), leading to an increased circulating glucose level in the blood.
- Epinephrine is a strong inhibitor of insulin secretion.
- Epinephrine is secreted in response to severe stress, cerebrovascular trauma, and myocardial infarction.
- Renal glycosuria may be seen when the renal tubule absorption of glucose is compromised; this may be seen in:
- End-stage renal disease.
- Osteomalacia.
- Fanconi’s syndrome.
What are the methods to detect glucose in the urine?
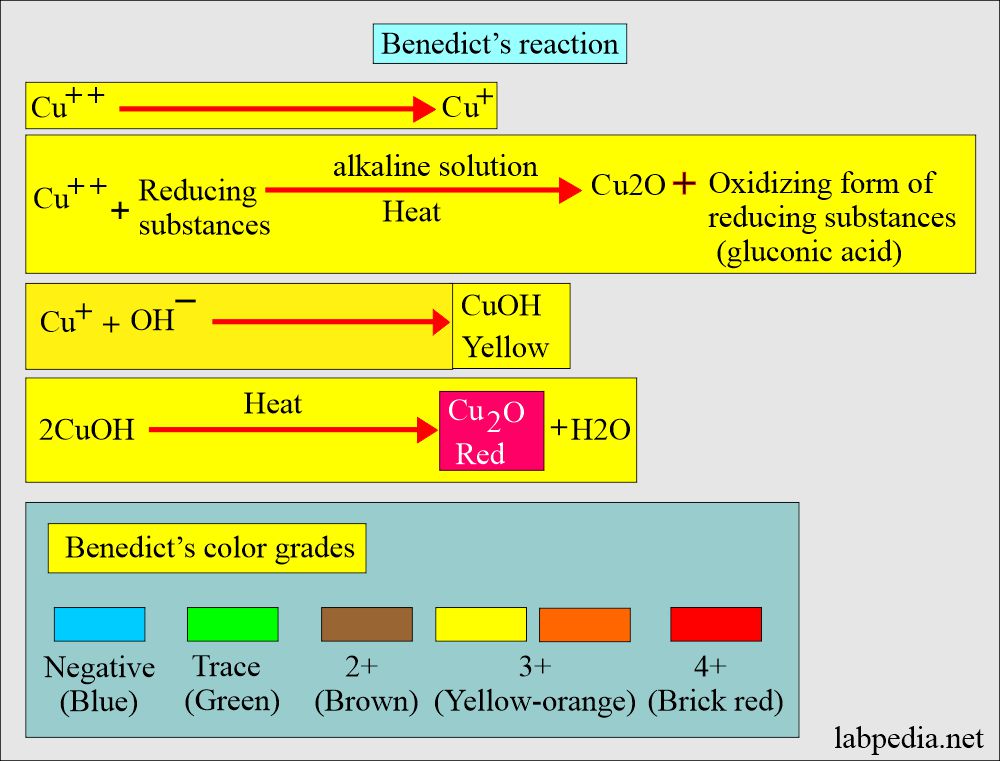
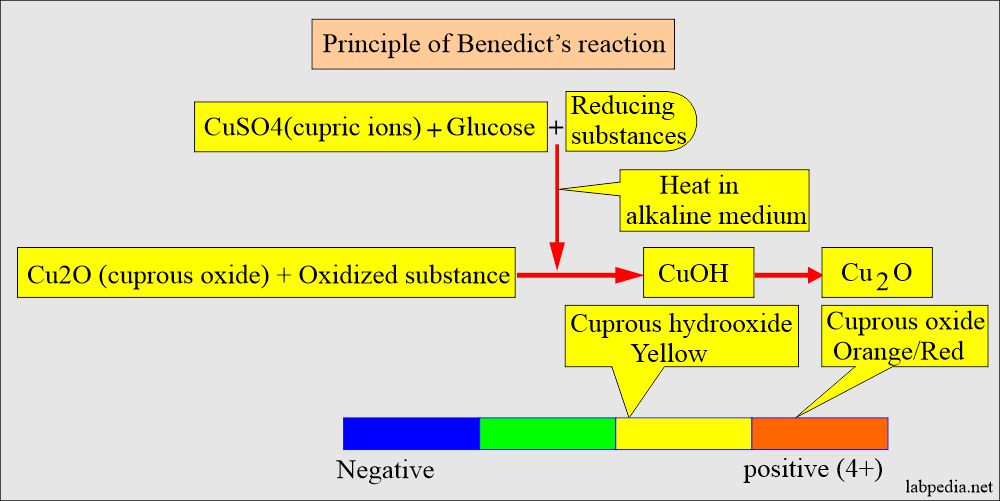
How will you describe the Copper reduction method?
- This test was used in the early days.
- This test involves reducing copper sulfate (CuSO4) to cuprous oxide in the presence of an alkali and heat.
- Reading: The color changes from blue (negative = CuSO4) to green, yellow, orange/red (CuO).
- Urine glucose benedict reaction:
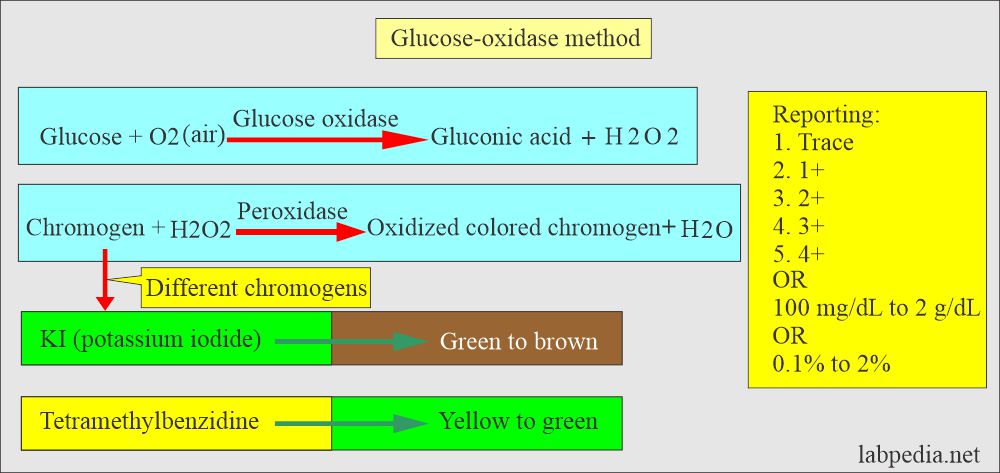
How would you describe Glucose-oxidase reagent strips?
- Glucose-oxidase only detects specific glucose in the urine, while copper reduction detects other reducing substances.
- The result is reported as 1+, 2+, 3+, and 4+, and these colors also provide quantitative measurements ranging from 100 mg/dL to 2000 mg/dL or 0.1% to 2%.
How would you compare the Benedict reaction and the Oxidase method?
| Characteristics | Benedict reaction (CuSO4) | Glucose oxidase |
|
|
|
|
|
|
|
|
|
|
|
What are the causes of Glucose in urine?
- Intravenous (IV) fluids.
- Uncontrolled diabetes.
- Adrenal gland diseases.
- Liver damage.
- Brain Injury.
- Poisoning.
- Kidney diseases.
- Pregnant women can have glucose in their urine, which is normal during pregnancy.
How would you define Hyperglycemia?
- It may be seen in nondiabetic cases where hormones act against the insulin, seen in conditions like:
- Pancreatitis.
- Pancreatic cancers.
- Cushing’s syndrome.
- Acromegaly.
- Hyperthyroidism.
- Pheochromocytoma.
Ketones in urine:
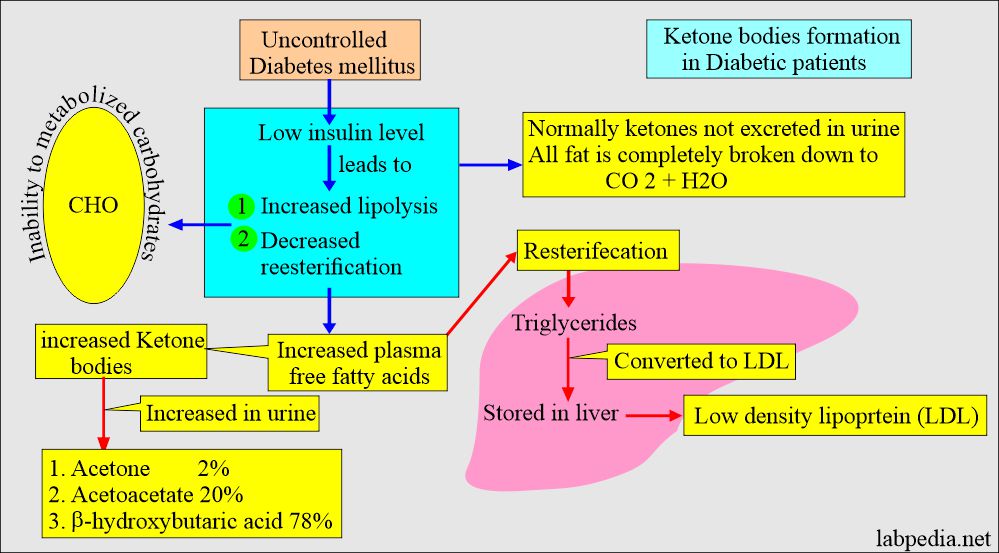
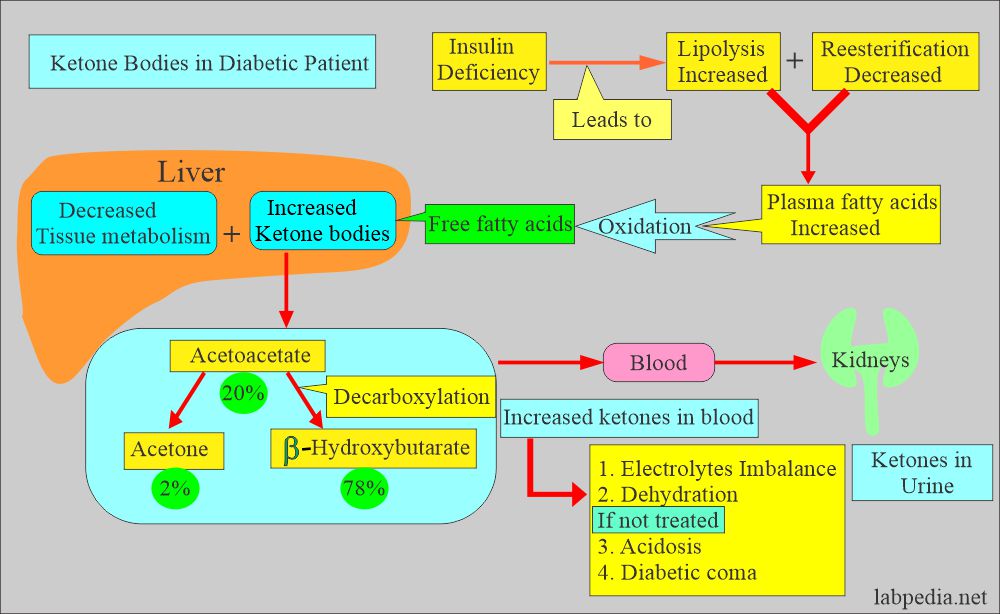
How will you define ketones in the urine?
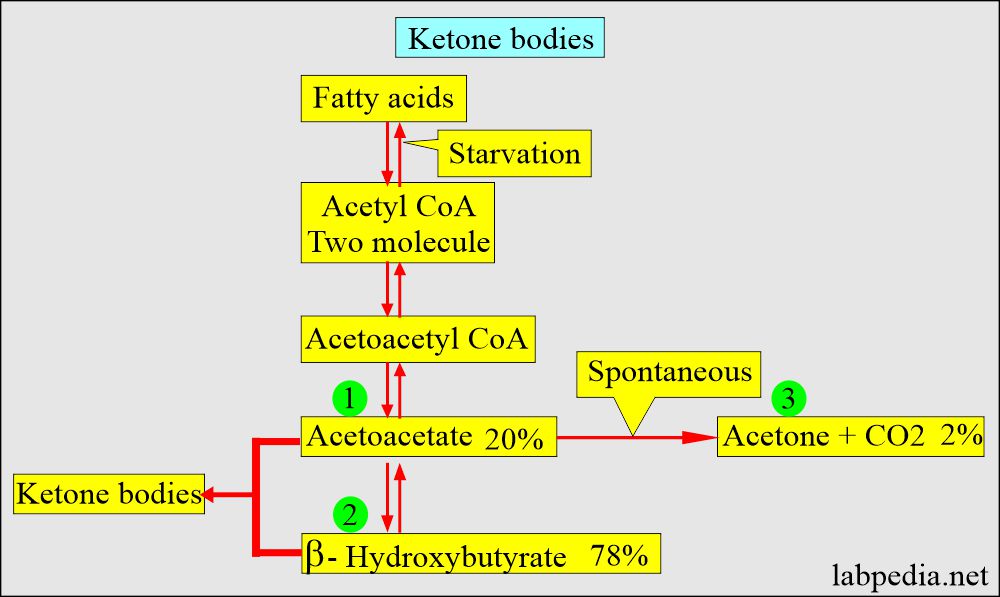
- Ketone bodies are mainly three intermediate products from lipolysis, and these are excreted in the urine:
- Acetone 2%.
- Acetoacetate 20%.
- β-hydroxybutyric acid 78%.
- Normally, the measurable amount of ketones doesn’t appear in the urine. All metabolized fat is broken down into carbon dioxide (CO2) and water (H2O).
- When the body lacks carbohydrates for energy, fat stores are metabolized to supply energy, and ketone bodies appear in the urine.
- The reason for the fat metabolism is the inability to metabolize carbohydrates, as seen in the following:
- Diabetes Mellitus.
- Vomiting.
- Inadequate intake of carbohydrates as in starvation.
- Ketonuria indicates a deficiency of insulin and can regulate the dose of insulin.
- Ketones are excreted in combination with basic ions (Na+, K+. and Ca++), so ketonuria produces ketoacidosis.
- These patients have a fruity odor on their breath because acetone is very volatile and blown off from the lungs.
- Normally, urine is negative.
- It is important in diabetes mellitus and particularly in uncontrolled diabetes mellitus patients.
What is the procedure to detect ketone bodies?
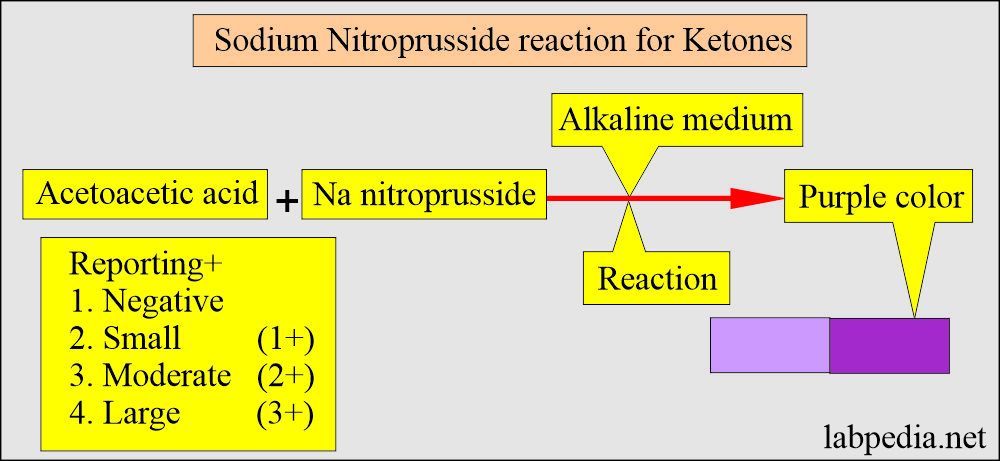
How will you report Ketone test strips or tablets?
- These are used based on sodium nitroprusside (nitroferricyanide) reaction to measure ketone bodies.
- This will detect acetoacetic acid or acetone in alkaline conditions.
- β-hydroxybutyric acid does not react with this reagent.
- Reporting of the result:
- The color changes from lavender to maroon (purple).
- Acetoacetate + acetone is expressed as:
- Negative = 0 mg/dL
- Small amount = 10 mg/dL
- Moderate amount = 30 mg/dL
- Large amount = 80 mg/dL
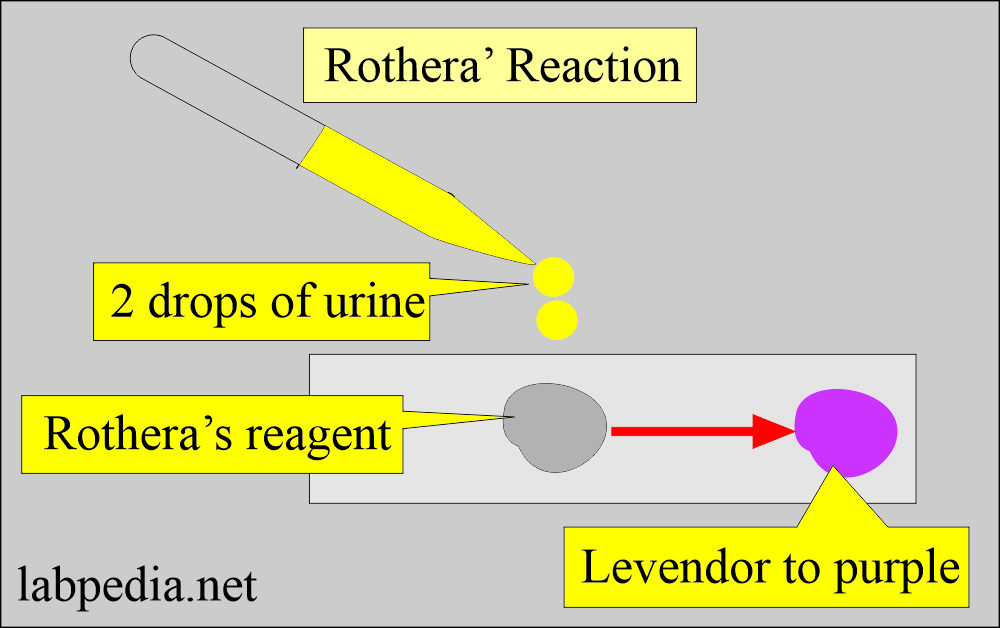
How will you discuss the Rothera’s test?
- Grind fine powder of :
- 10 g Na2CO3 (anhydrous).
- 20 g (NH4)2SO4.
- 0.5 g sodium nitroprusside.
- Mix the powder completely and stopper it tightly.
- Procedure: Take about 0.5 g of the above powder on a flat surface.
- Add 2 drops of urine to the powder.
- Ketone-positive urine will change color from lavender to purple in 30 seconds.
What are the causes of Abnormal Ketonuria?
- Uncontrolled diabetes.
- Very low-carbohydrate diet.
- Starvation.
- Eating disorders, e.g., anorexia nervosa or bulimia.
- Alcoholism.
- Poisoning from drinking rubbing alcohol (isopropanol).
- Ketones are often found in the urine during fasting for 18 hours or longer.
- The sick person cannot eat or vomit for several days.
- Low levels of ketones are sometimes found in the urine of healthy pregnant women.
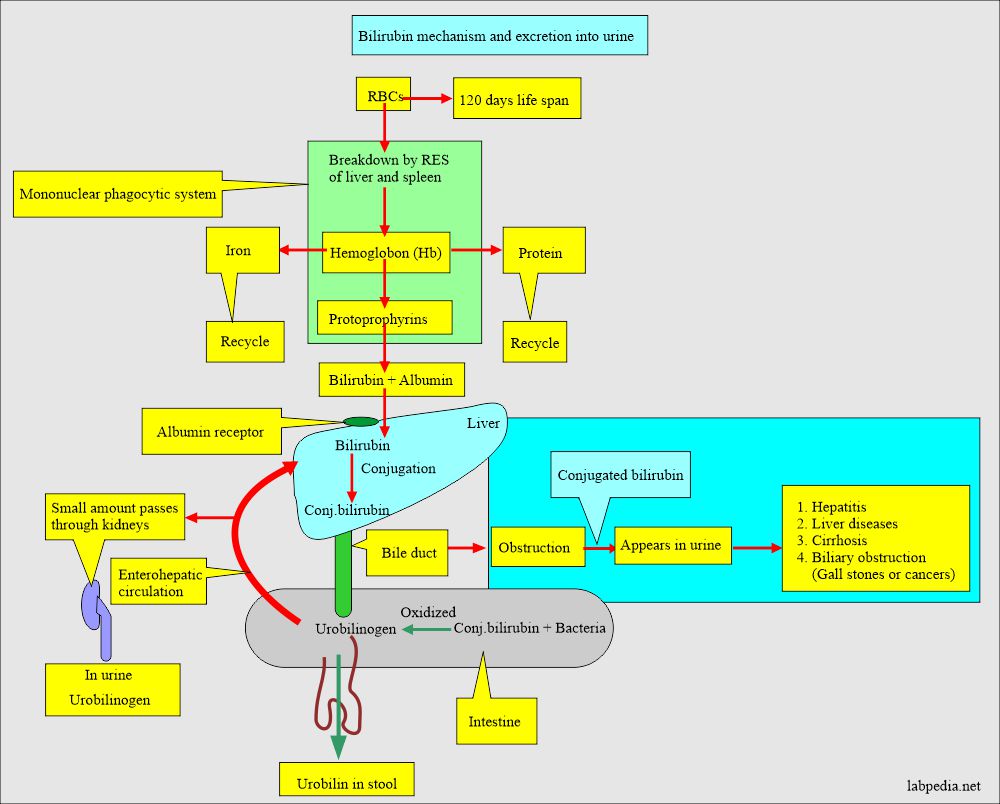
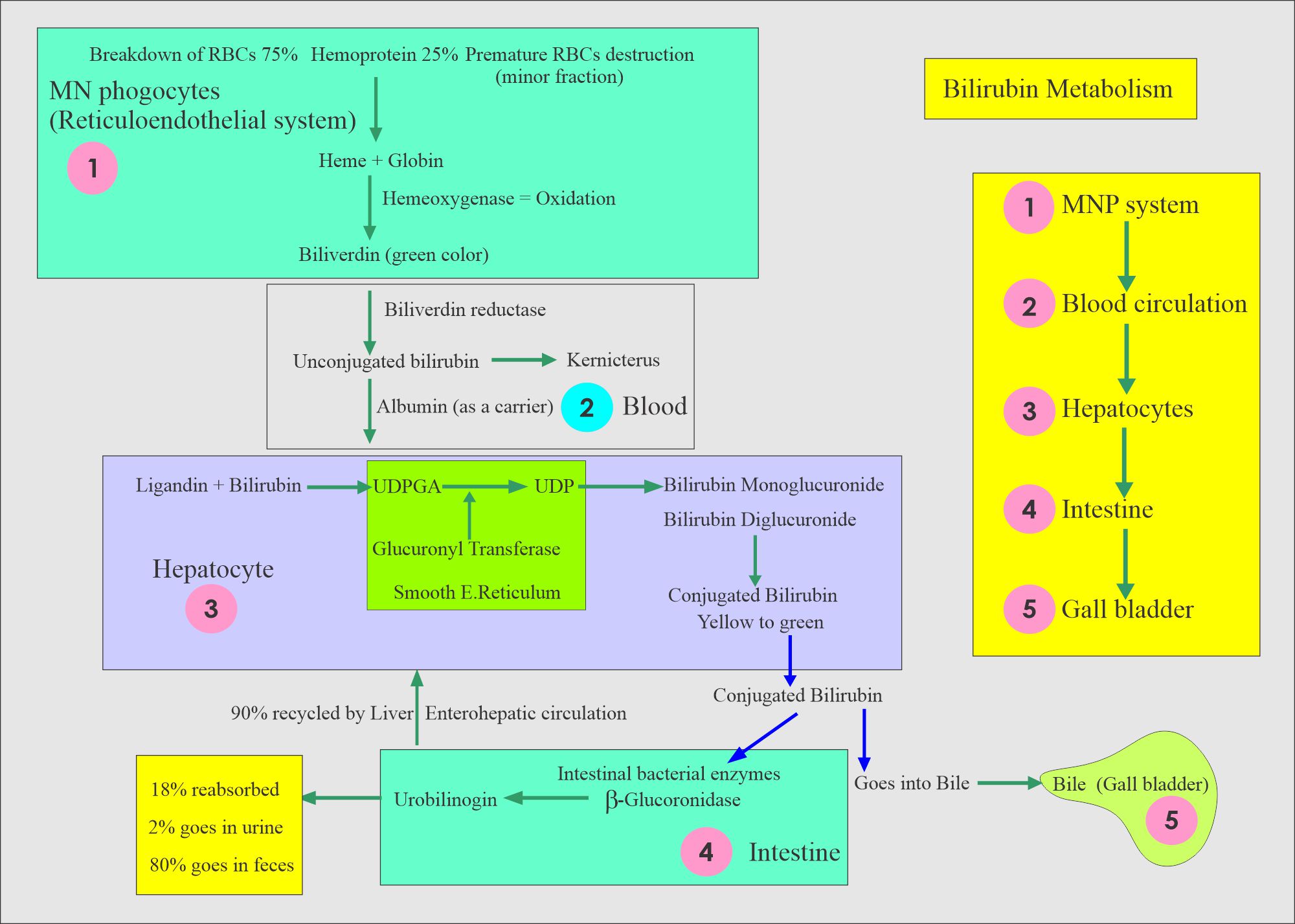
Bilirubin in urine
How will you define bilirubin in the urine?
- Bilirubin is a yellow-orange bile pigment compound formed when RBCs are hemolysed or ruptured.
- The appearance of bilirubin in the urine indicates a liver disease called bilirubinuria.
- Bilirubin is a pigmented yellow compound, a degradation product of hemoglobin.
- It is detected long before jaundice clinically appears.
- It is negative in normal urine.
- Negative in hemolytic jaundice.
- Increased bilirubinuria is seen in the hepatic and obstructive jaundice.
What type of bilirubin appears in the urine?
- Conjugated bilirubin appears in the urine when the normal degradation cycle is disrupted by obstruction of the bile duct, such as gallstones or cancer.
- Another possibility is when the liver cells are damaged, which allows the leakage of bilirubin directly into the circulation.
- Hepatitis and cirrhosis are common causes of liver cell damage and result in bilirubinuria.
- Increased hemolysis does not produce bilirubinuria.
- Bilirubin in the urine is detected only if the urine sample is fresh because bilirubin decomposes rapidly in bright light.
- If the urine is left in the lab, then bilirubin is converted into biliverdin, a green compound by the light not detected by the bilirubin strips.
What is the clinical importance of bilirubin in the urine (bilirubinuria)?
- Hepatitis (infectious).
- Liver diseases.
- Cirrhosis.
- Gallbladder stones (cholelithiasis) or cancer-causing obstruction.
- Normal:
- Urine bilirubin is negative (0 to 0.2 mg/dL (0 to 0.34 µmol/L).
- Bilirubin can be detected in urine by the Foam test.
How will you describe the Procedure for the foam test?
- Place a small volume of the urine in the test tube, cap it, and shake it vigorously.
- Result:
- The foam at the top is white, which means bilirubin is negative.
- If the foam is orange, the color means bilirubin is present.
- Other methods to detect bilirubin in the urine are:
- Diazo reaction is in the form of tablets or dipsticks.
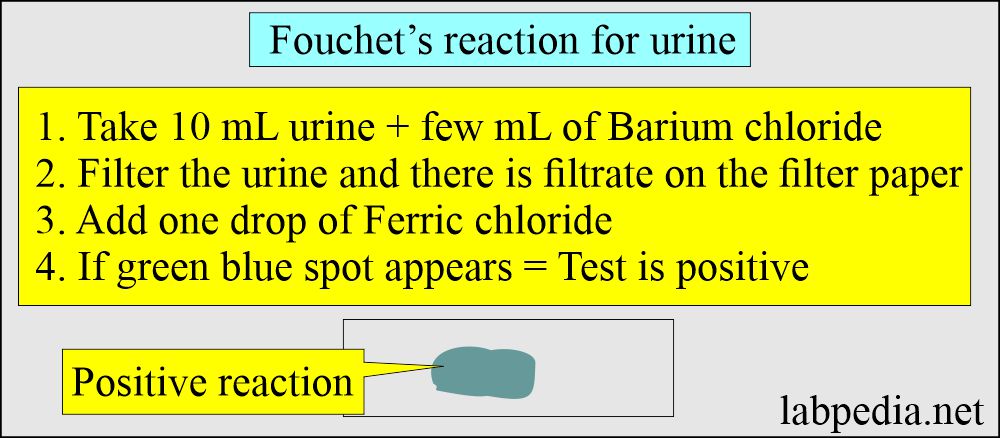
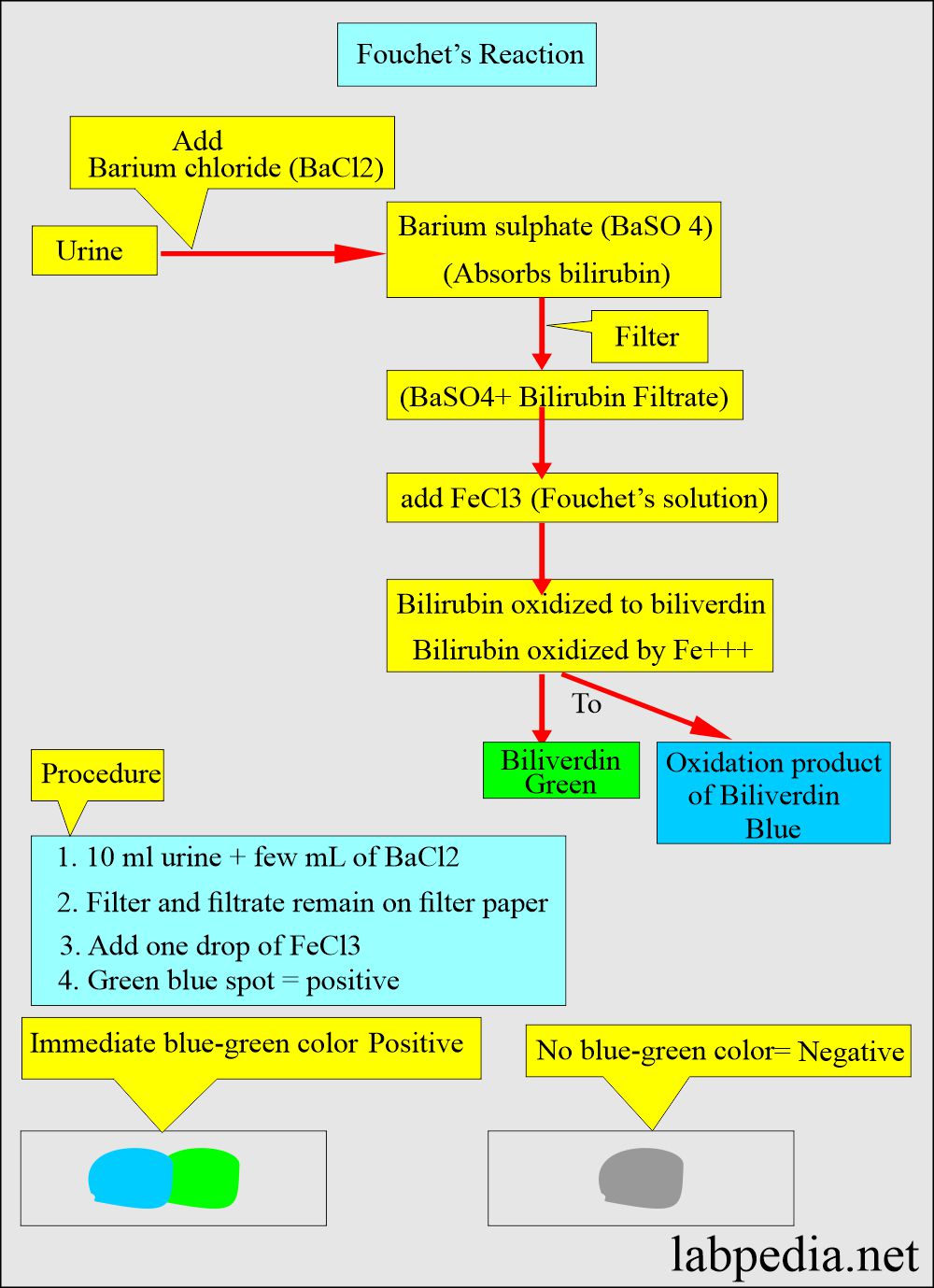
How will you describe Fouchet’s test (Ferric chloride test.)?
- This is basically an oxidizing reaction.
What is another modification of Fouchet’s test for urine bilirubin?
- Composition of Fouchet’s reagent:
- Trichloracetic acid = 25 g
- Ferric chloride = 10% aqueous solution.
- Distle water = 100 mL
- procedure: Take 10 mL of urine.
- Add 1 g barium chloride.
- Mix and filter.
- Leave the precipitate on filter paper and let it dry.
- Add Fouchet’s reagent or yellow nitric acid to the precipitate.
How will you compare Fouchet’s (Ferric chloride) and Diazo’s reactions for Bilirubin?
| Characteristic feature | Fouchet’s test (Ferric chloride test) | Diazo reaction (tablet or dipstick) |
|
|
|
|
|
|
|
|
|
Urobilinogen in urine
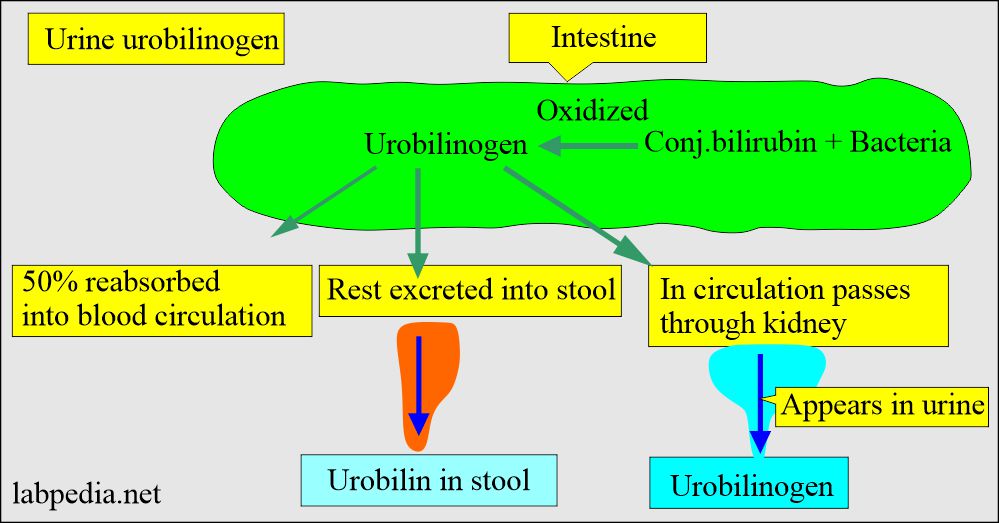
How will you define urobilinogen in the urine?
- Urobilinogen is like bilirubin bile pigment, resulting from the hemoglobin degradation product.
- Urobilinogen is a colorless compound derived from bilirubin. It is excreted into the bile and partially hydrogenated by bacteria in the intestine.
- As shown in the above diagram, bacterial action on the bilirubin produces it in the intestine.
- The intestine reabsorbs approximately 50% of urobilinogen.
- Rest excreted in the feces.
- A small amount of enterohepatic circulation passes from the kidney and is excreted in the urine as urobilin.
- This is why urobilinogen is positive normally in the urine.
- Urobilirubin excreted from 0.5 to 4 mg /24 hours.
- <1 mg/dL is normally found in the urine.
- At least 0.1 mg/dL is needed for the detection.
How to check Urobilinogen in the urine:
- The reagent strip for urobilinogen involves the Ehrlich aldehyde reaction. This will form the red azo dye.
- This test must be done on the fresh sample because urobilinogen is an unstable compound that breaks down into urobilin on standing.
What is the significance of urobilinogen in the urine?
- It helps in the early detection of liver diseases.
- It is an increase in hemolytic disorder.
- In hepatic jaundice, liver disorder, hepatitis, cirrhosis, and cancers.
- It is absent in obstructive jaundice.
What is the amount of Urobilinogen in the urine sample?
| Time | Value of urobilinogen |
|
|
|
|
|
|
|
|
|
|
What are the causes of increased levels of urobilinogen in urine?
- Hemolytic anemia.
- Pernicious (megaloblstic) anemia.
- Malarial attack.
- Excessive bruising.
- Pulmonary infarction.
- Cirrhosis.
- Acute hepatitis.
- Cholangitis.
What are the causes of decreased levels of urobilinogen in the urine?
- Complete or partial obstruction of the biliary tract.
- Cholelithiasis.
- Biliary duct inflammation.
- Cancer of the head of the pancreas.
- Antibiotic therapy will suppress intestinal bacterial flora.
How will you differentiate between Bilirubin and urobilinogen in the urine?
| Chemical | In normal condition | Hepatic diseases | Biliary obstruction | Hemolytic disease |
| Urine bilirubin | Negative | positive or negative | Positive (+++) | Negative |
| Urine urobilinogen | Normal | Increased (++) | Absent or low (normal) | Increased (+++) |
Microscopic Urine analysis:
What are the normal microscopic findings of the urine?
- Normally, Very few or no red or white blood cells or casts are seen.
- No bacteria, yeast cells, or parasites are present.
- A few crystals are normally seen.
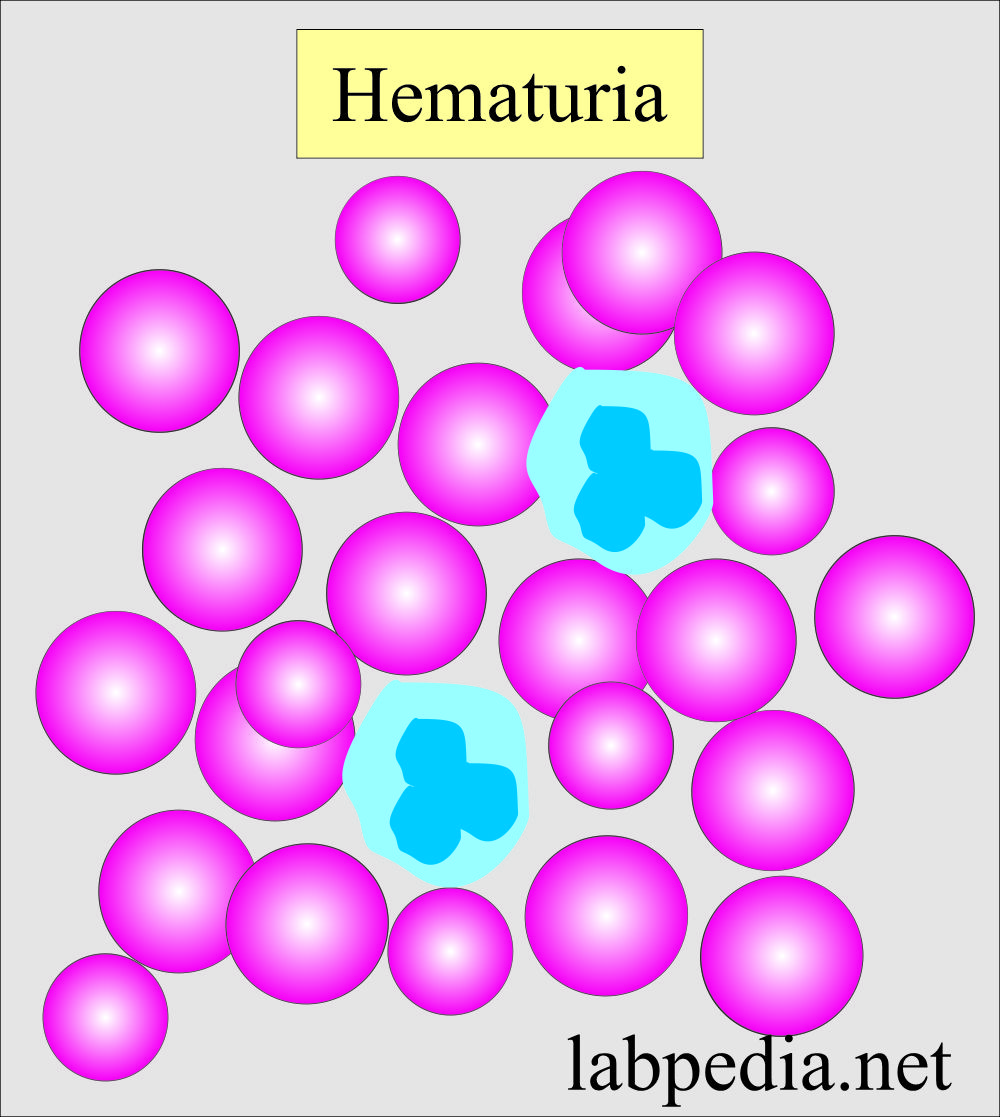
RBCs in the urine
What do RBCs in urine indicate?
- The positive blood test indicates the presence of RBCs.
What are the causes of Hematuria?
- It is a disorder of renal or genitourinary origin where the bleeding is due to trauma or damage to the organs.
- The main causes are:
- Renal calculi.
- Glomerular diseases.
- Malignancies.
- Pyelonephritis.
- Trauma.
What are the causes of Hemoglobinuria?
- This may result from the lysis of RBCs. There will be mixed hemoglobinuria and hematuria.
- There may be lysis of RBCs in the urinary tract in alkaline urine.
- In intravascular hemolysis, no RBCs are seen in the urine.
What are the causes of Myoglobinuria?
- It is a heme-containing protein found in the muscles. This is seen in Rhabdomyolysis like :
- Trauma.
- Crush syndrome.
- Convulsions.
- Muscle-wasting disease.
- Heroin abuse.
- Prolonged come.
- Extensive exertion.
What are the causes of Red blood cells in the urine?
- Kidney or bladder injury.
- Kidney stones.
- Urinary tract infection (UTI).
- Inflammation of the kidneys (glomerulonephritis).
- Kidney or bladder tumor.
- An autoimmune disease like systemic lupus erythematosus (SLE).
| Lab test | Myoglobinuria | Hemoglobinuria |
|
|
|
|
|
|
|
|
|
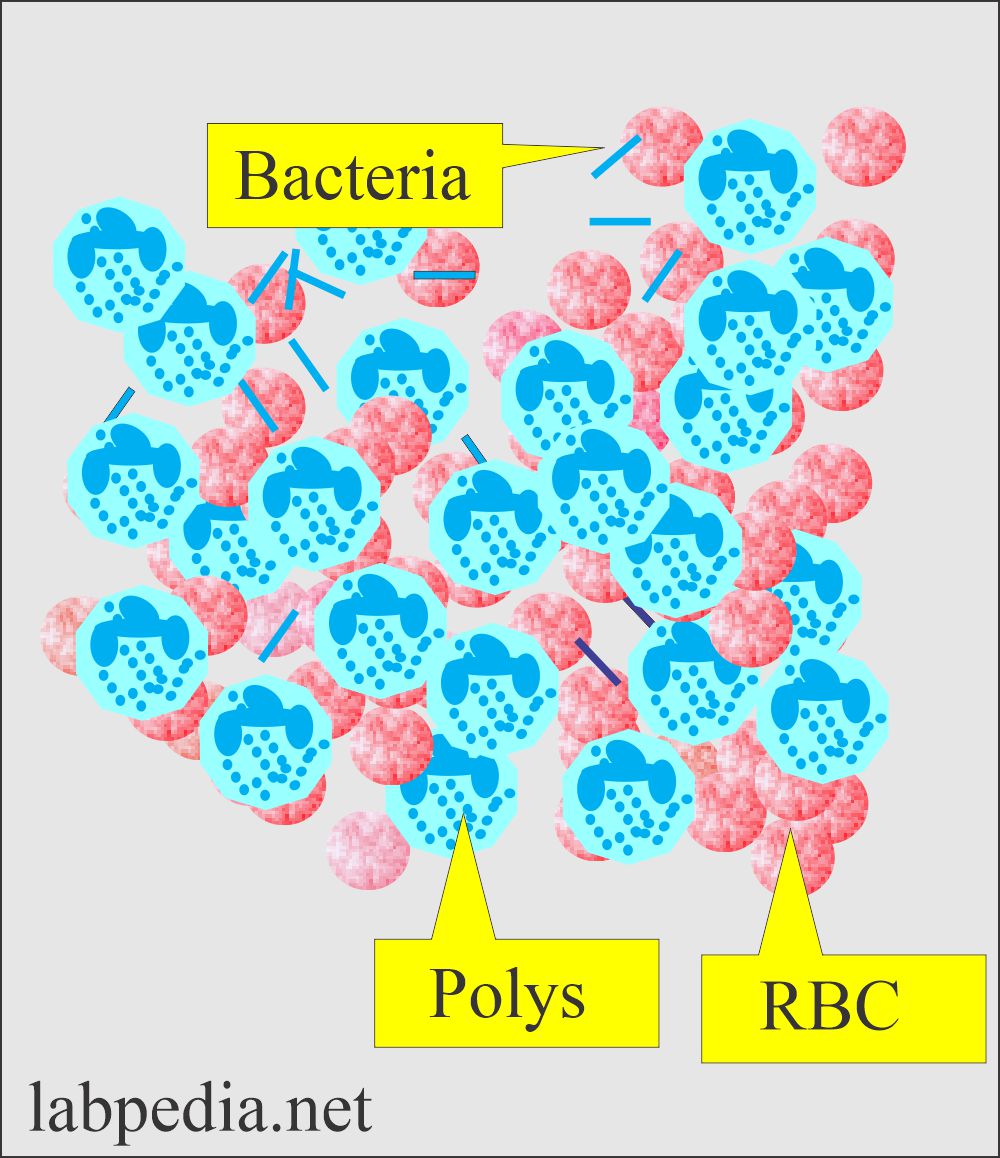
White blood cells in urine:
What are the causes of Pus cells in the urine?
- Pus cells in the urine may be caused by :
- Urinary tract infection.
- Urinary bladder tumor.
- Inflammation of the kidneys.
- The Systemic lupus erythematosus (SLE).
- Inflammation in the vagina or under the foreskin of the penis.
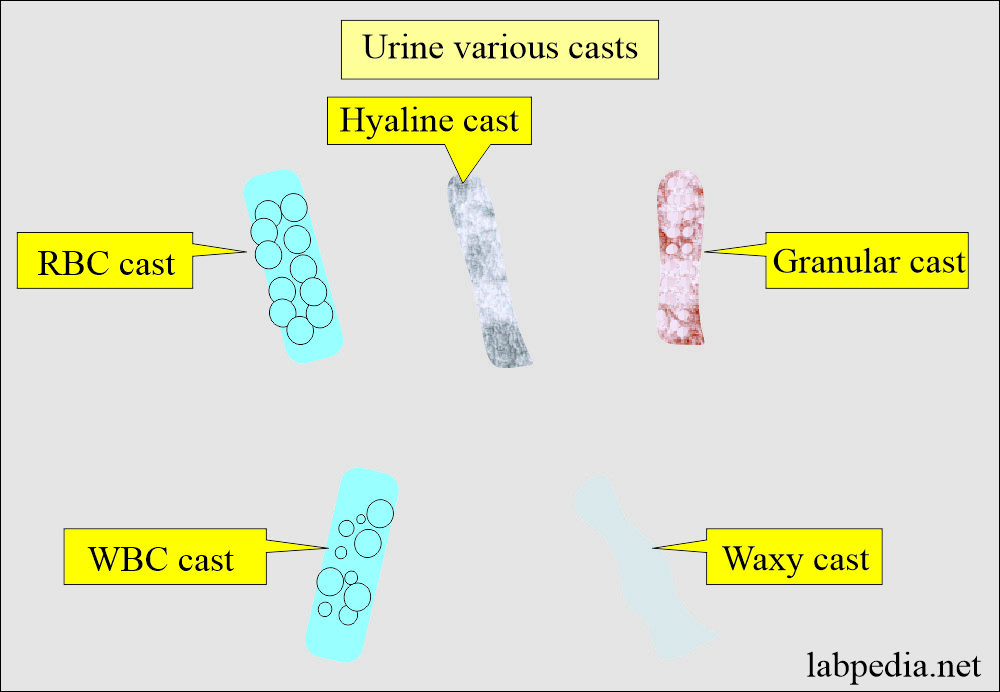
Cast in the urine
What are the causes of CASTs in urine?
- Urine sediment after the centrifugation shows the crystals and casts.
- Casts are formed in the collecting tubules.
- Various types of urine casts have different significance.
- Depending upon the various reasons, there are the following types of casts:
- Granular cast:
- Granular casts appear homogenous, coarsely granular, and very dense.
- These casts are colorless.
- Granular casts are found in:
- Acute tubular necrosis.
- Pyelonephritis.
- Advanced glomerulonephritis.
- Hyline cast:
- These are clear and colorless and form when the tubules contain precipitated proteins.
- Hyaline casts may be seen in physiologic states like strenuous exercise and mild renal disease.
- These are not associated with any particular disease.
- Hyaline casts are found in:
- Malignant hypertension.
- Chronic renal diseases.
- Diabetic nephropathy.
- Congestive heart failure.
- Pyelonephritis.
- Glomerulonephritis.
- Cellular cast:
- These are WBC cell casts.
- WBC casts can originate from any place in the urogenital tract.
- WBC casts always come from the renal tubules.
- WBC casts are found in:
- Lupus nephritis.
- Acute glomerulonephritis.
- Pyelonephritis.
- Acute glomerulonephritis.
- Epithelial cast:
- Renal epithelial cell casts formed from the shedding of the renal tubular cells.
- These shed cells undergo degenerative changes.
- These casts are first coarse and then become fine granular.
- Epithelial cell casts are found in:
- Acute tubular necrosis.
- Pyelonephritis.
- Acute glomerulonephritis.
- Viral infection like CMV.
- Drug intoxication like salicylate overdose.
- Waxy cast:
- Waxy casts formed from the degeneration of the granular cast.
- Waxy casts are found in:
- Nephrotic syndrome.
- Severe renal failure.
- Renal amyloidosis.
- Malignant hypertension.
- Diabetic nephropathy.
Crystals in urine:
What are the causes of crystals in the urine?
- Crystals in the urine are identified by their specific shapes.
- These crystals are also identified by their solubility.
- Mostly, there are no symptoms due to these crystals.
- Sometimes, these crystals may be associated with renal stone formation, leading to obstruction.
- The presence of large amounts of crystals or certain types of crystals indicates :
- Kidney stones.
- Damaged kidneys.
- Problems with metabolism.
- Medicines.
- Some types of urinary tract infections can also increase the number of crystals in the urine.
| Types of crystals | Color of the crystals | Acidic urine | Alkaline urine | Soluble with heat |
| Amorphous urates | Pink to brick red | present | absent | yes |
| Uric acid crystals | Mostly yellow brown | present | absent | yes |
| Contrast media | White | present | ||
| Amorphous phosphates | White | absent | present | |
| Amorphous carbonates | Colorless | absent | present |
Bacteria in urine:
What are the causes of bacteria in the urine?
- A urine nitrite test is done to confirm the bacteria in the urine.
- Nitrie is a rapid and indirect method of detecting urinary infections.
- Gram-negative bacteria produce enzymes that reduce the nitrate into nitrite.
- To check the bacterial infection, a nitrate test is advised:
- Pregnant women.
- School-going children, especially girls.
- Old people.
- Diabetic nephropathy.
- Patient with recurrent urinary infection.
- Mostly, the infection starts in the urinary bladder and goes upwards to the kidneys.
- A bacteria-positive test in the urine means a urinary tract infection (UTI).
Yeast cells or parasites:
What are the causes of yeast and parasites in the urine?
- Such as the parasite that causes trichomoniasis, which means an infection of the urinary tract.
Normal urine picture:
What is the normal urine picture?
| Physical features | Chemical features | Microscopic findings |
|
|
|
Questions and answers:
Note: The details of urine microscopy are seen in urine part 2.


Sir,
Do you have any notes or pdf for biomedical waste management … please help sir😟
Hello Doctors, I have sent a comment through your contact page but not sure if you will receive it.
I love your work and have worked my way through the three Urinalysis pieces. I develop presentations for nurses and find how you describe the science so easy to understand and interpret.
I need to reference the test and charts I may use correctly. Therefore can I ask you to let me know the actual authors names for the Urinalysis articles, I would hate to offend by not citing the author correctly. I will also need the date of last updates to the articles.
I am sorry to ask you to do this form me, as I admire you for taking the time and energy to produce such wonderful work and then kindly going on to share it with the nursing and medical world.
Thank you. Kind regards Denise Gamblin xx
Please write labpedia.net by Prof. Riaz A. Bhutta, last updated in April. 17, 2023.