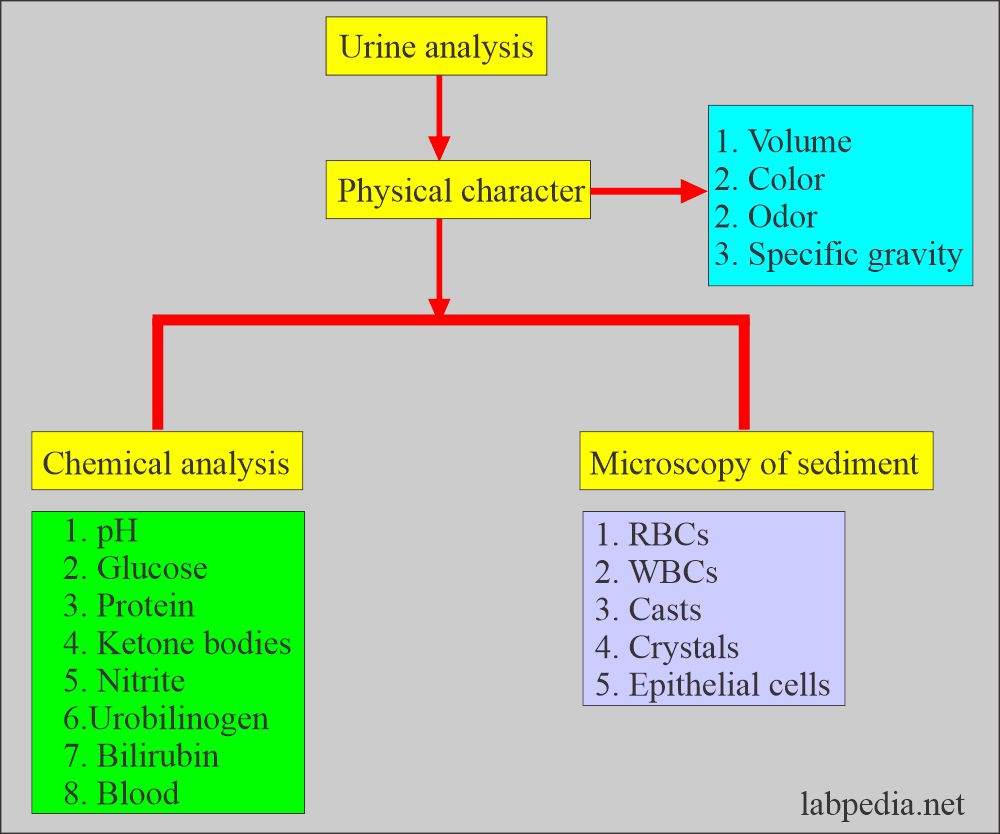
Urine Analysis:- Part 4 – Urine Chemical Examination and Interpretations
Urine Chemical Examination
What sample is needed for the urine analysis?
- Preferably use freshly voided urine.
- If there is a delay, then refrigerate the urine.
- The morning sample is concentrated urine.
What are the precautions for urine analysis?
- Preferably examine the urine within the first 30 minutes.
- Reject unlabelled urine sample.
- Avoid fecal or menstrual blood contamination.
What does urine chemical examination include?
- Urine protein.
- Glucose.
- Ketone bodies.
- Bilirubin.
- Urobilinogen.
Protein in the Urine:
How will you define normal urine protein?
- A normal, healthy person will have a daily protein exertion of 100 mg/day. This is a very small proportion of the total plasma protein.
- Because of its smaller size, it is mostly albumin, with a small fraction of globulin as well.
- The proximal tubules reabsorb most of the protein filtered in the glomerular filtrate.
What is the mechanism of proteinuria?
- As a result of increased filtration from the glomerulus.
- Or it is decreased reabsorption from the tubules.
- Proteinuria is the first indicator of renal disease.
- The random sample is negative.
What are the types of proteinuria?
- Prerenal proteinuria:
- Nonrenal diseases cause this and is transient; it is seen in:
- Hemoglobinuria.
- Myoglobinuria.
- Acute phase proteinuria.
- This is usually not detected by the routine urine reagent strips.
- Renal proteinuria:
- This is due to renal diseases involving glomeruli or tubules.
- Albumin appears in the urine in glomerular damage, followed by the WBCs and RBCs.
- It is seen in:
- SLE.
- Streptococcal glomerulonephritis.
- Strenuous exercise (reversible condition).
- Pre-eclampsia and hypertension. (reversible condition).
- Toxic heavy metals.
- Severe viral infection.
- Postrenal proteinuria:
- Proteins can be added as the urine passes through the ureter, urinary bladder, and urethra.
- Bacterial and fungal infection of the lower urinary tract,
- Menstrual contamination also contains proteins.
- Prostatic fluid and spermatozoa.
How will you define Orthostatic or postural proteinuria?
- This is a persistent benign condition frequently seen in young patients.
- It appears when the person is upright and disappears when the patient lies down.
- Procedure to confirm the diagnosis:
- These patients are advised to empty their bladders before going to bed.
- Take the first urine sample when patients get up.
- Take another sample when patients are upright for several hours.
- The first sample will be negative.
- The second sample will be positive in orthostatic proteinuria.
How will you discuss Microalbuminuria?
- This is seen in diabetic nephropathy.
- This microalbuminuria indicates diabetic complications.
- The further complications of diabetes can be prevented by controlling diabetes.
- This is also associated with an increased risk of cardiovascular diseases.
- Microalbuminuria is reported as albumin excreted as µg/min or in mg/24 hours.
- The level is significant from 20 to 200 µg/min Or 30 to 300 mg/24 hours.
- In these cases, the albumin/creatinine ratio is >3.4 mg/mmol.
- The first-morning specimen is recommended.
How will you define Bence Jones proteinuria (BJ)?
- It is seen in multiple myeloma patients.
- These are monoclonal light-chain immunoglobulins.
- This is a low molecular weight protein and is excreted in the urine.
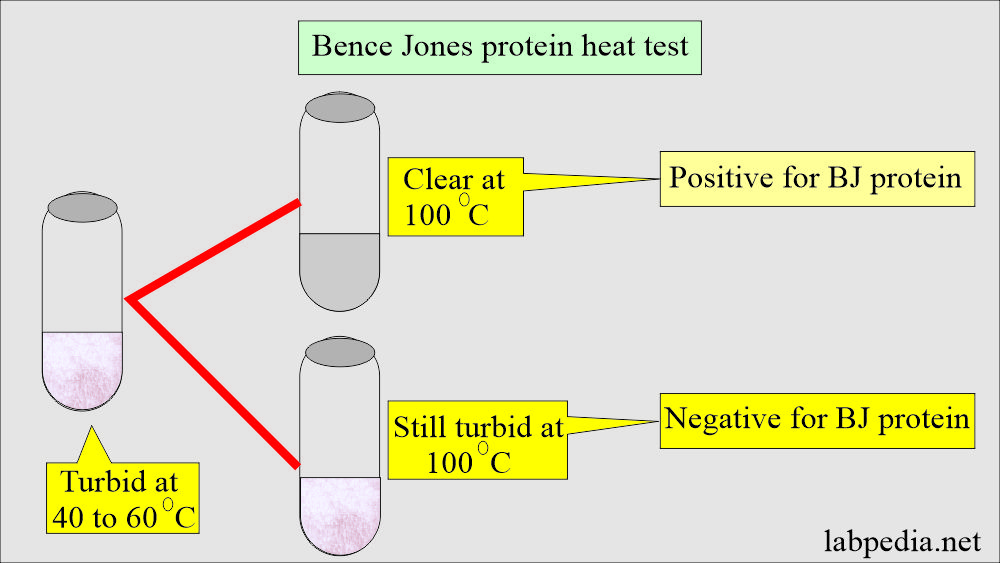
How will you detect BJ protein?
- Heat the urine, and these proteins coagulate at 40 to 60 °C.
- Dissolve when the temperature reaches 100 °C.
- Reading the result: Urine turbid at 40 to 60 °C and clear at 100 °C is considered positive.
How will you classify proteinuria?
| Degree of proteinuria | Amount of protein excreted in the urine | Etiology |
|
|
|
|
|
|
|
|
1. Chronic pyelonephritis 2. Polycystic kidneys 3. Renal tubular diseases |
|
|
|
|
|
|
What is the normal urine protein?
- In 24 hours of urine, 150 mg or 20 mg/dL ( another source = 0 to 0.1 gm).
- Another source: Protein in the urine is <10 mg/dL or 100 mg/24 hours.
- This protein consists mainly of low-molecular-weight serum proteins, so the major protein is the albumin seen in the urine.
- Other proteins include serum and tubular microglobulins, Tamm Horsfall protein produced by the tubules, and proteins from the prostate and vaginal secretions.
How to check proteinuria?
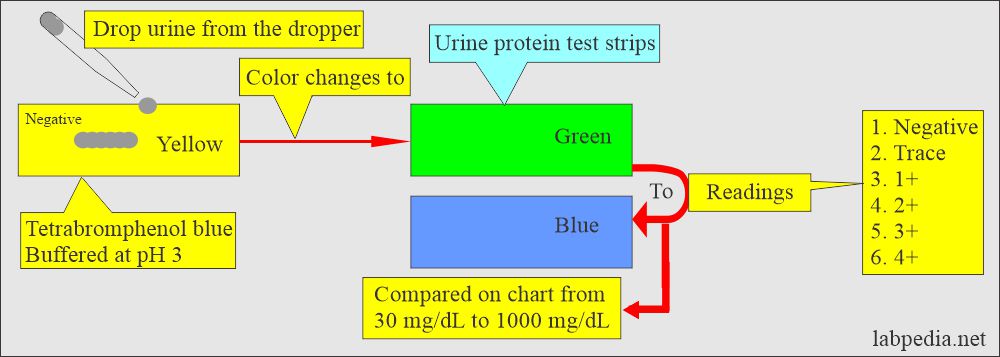
Urine strips:
- These are mostly used to screen for proteinuria. These strips are specific for albumin.
- False-positive results are seen in the following:
- In alkaline urine.
- In highly buffered urine.
How will you perform a reagent test strip test for protein in the urine?
What are the tests used to detect urine protein?
| Characteristics | Heat and acid | Reagent strip | Salfosalicylic acid |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
What are the clinical types of proteinuria and its etiology?
| Clinical type of proteinuria | Etiology of proteinuria |
|
|
|
|
|
|
|
|
Glucose in the urine:
What is the significance of glucose in the urine?
- Because of the diagnosis of diabetes mellitus, a glucose test in the urine is very commonly advised.
- The blood glucose and urine glucose tests are part of a routine check-up.
- Early diagnosis of diabetes mellitus helps improve the prognosis and complications of diabetes mellitus.
Write briefly glucose metabolism?
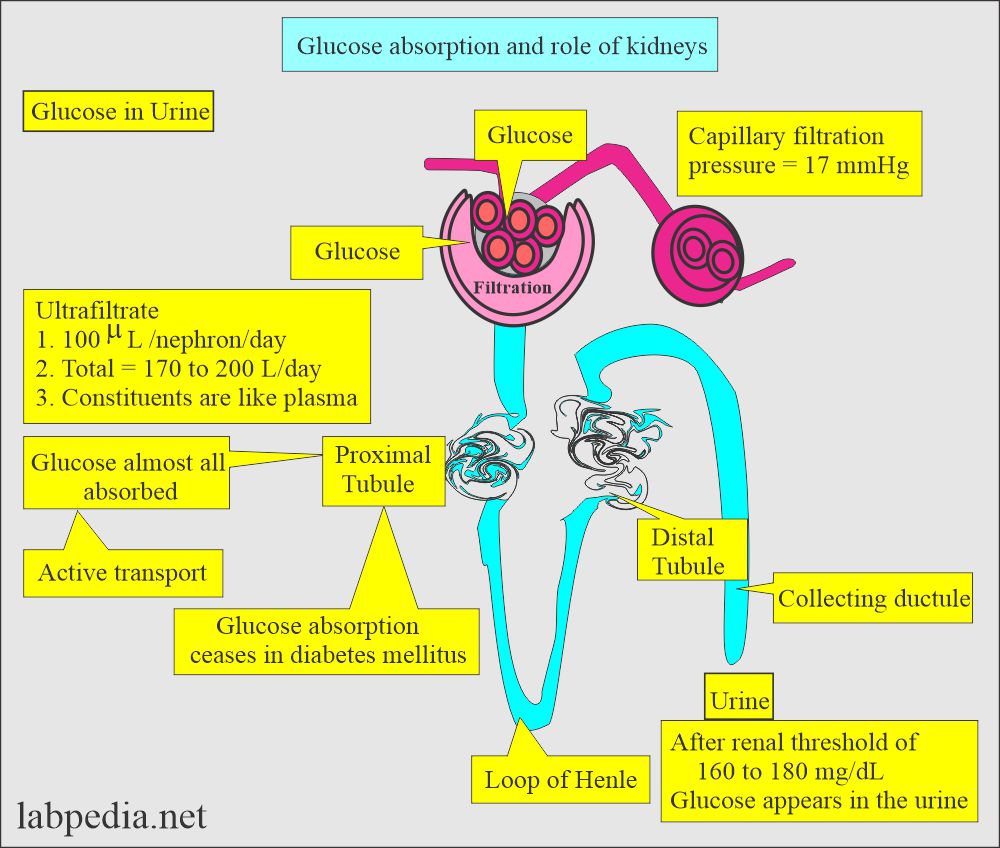
- The proximal convoluted tubules almost all absorb glucose filtered in the glomerular filtrate; therefore, there will be a negligible amount of glucose in the urine.
- Tubular absorption of glucose is an active process that depends upon the body’s needs.
- In diabetes mellitus, tubular glucose transport ceases, and glucose appears in the urine.
- In hyperglycemia, the tubular transport of glucose stops, and glucose starts appearing in the urine.
- To test for diabetes mellitus, take it after 2 hours of the meal.
- The first-morning sample does not give a real picture of the last evening meal. Void the first sample and then collect the next sample.
- The renal glucose threshold is 160 to 180 mg/dL.
What is the normal glucose in the urine?
- A random sample is negative (qualitatively, it is negative).
- In 24 hours, urine glucose is 0 to 0.3 grams.
- Another source, glucose in random urine, is <30 mg/dL.
- Glucose in urine during pregnancy is called gestational diabetes.
- This is usually seen around the 6 months of pregnancy.
- Hormones secreted by the placenta during pregnancy are believed to block insulin’s action and lead to hyperglycemia.
What is Renal glycosuria?
- It is seen when the blood glucose level is normal and glucose appears in the urine.
- Renal tubules’ absorption of glucose by the tubules is compromised.
- It is usually seen in end-stage kidney diseases, osteomalacia, and Fanconi’s syndrome.
- Glucose false tests are seen in urine with a high specific gravity and a large amount of ascorbic acid.
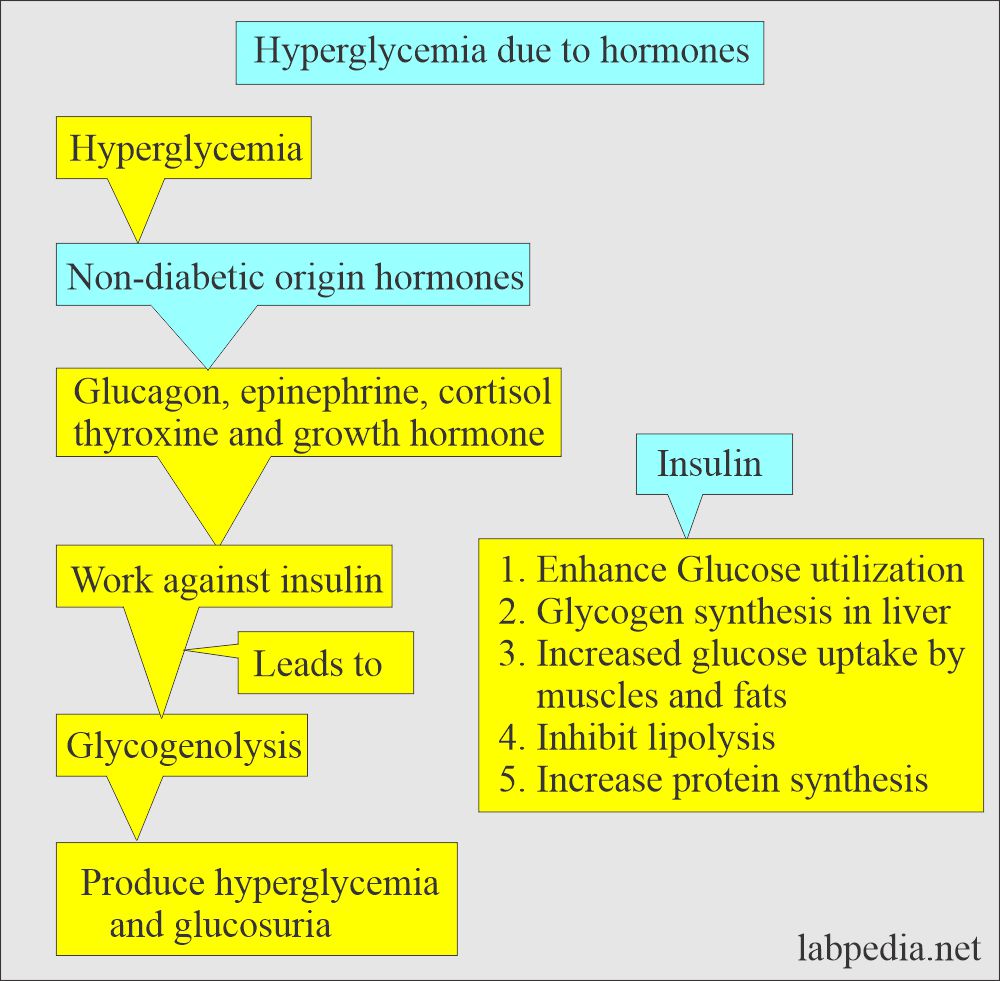
What are the causes of Hyperglycemia of nondiabetic origin?
- It is seen in the following conditions:
- Pancreatitis.
- Pancreatic cancer.
- Acromegaly.
- Cushing’s syndrome.
- Hyperthyroidism.
- Pheochromocytoma.
- The above conditions produce hormones like glucagon, epinephrine, cortisol, thyroxine, and growth hormone.
- These hormones act against insulin and lead to glycogenolysis.
How will you check Glucose in the urine?
- Reagents strips, glucose oxidase reaction.
- Copper reduction method.
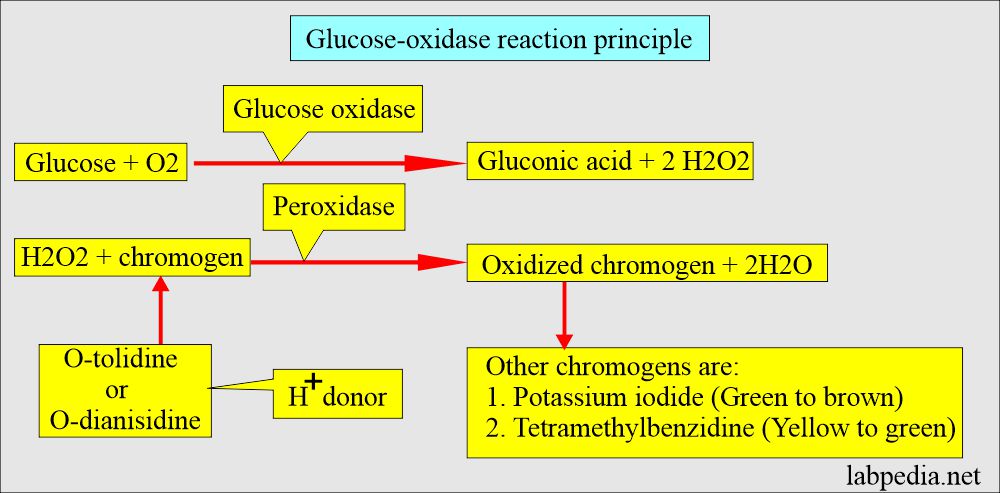
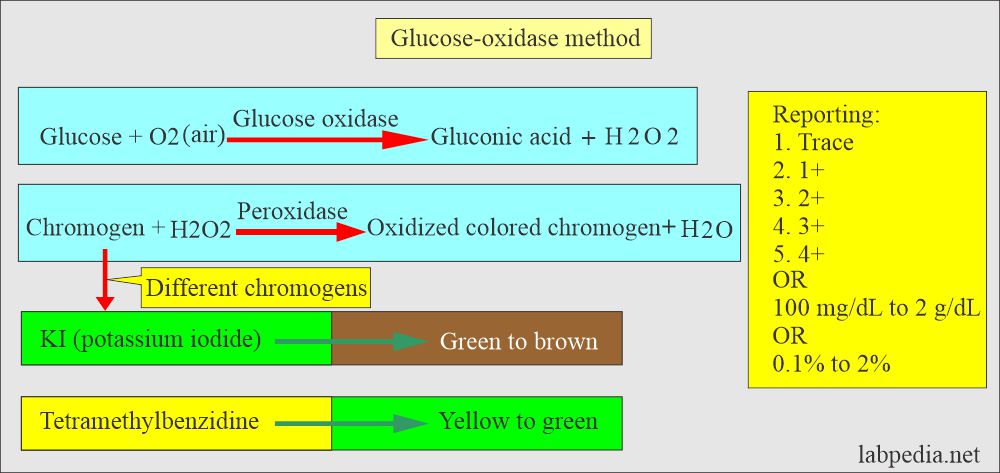
How will you describe Glucose-oxidase reagent strips?
- This test is specific for the β-isomer of glucose.
- It converts glucose in the presence of oxygen to gluconic acid and hydrogen peroxide.
- The serum glucose concentration is proportional to the oxygen consumed in the reaction or the H2O2 produced.
- In the second step, peroxidase catalyzes the reaction between H2O2 and chromogen to form the oxidized colored compound, indicating the presence of glucose in the urine.
- The result is reported as follows:
- Trace, 1+, 2+, 3+, 4+
- These colors also provide quantitative measurements ranging from 100 mg/dL to 2000 mg/dL or 0.1% to 2%.
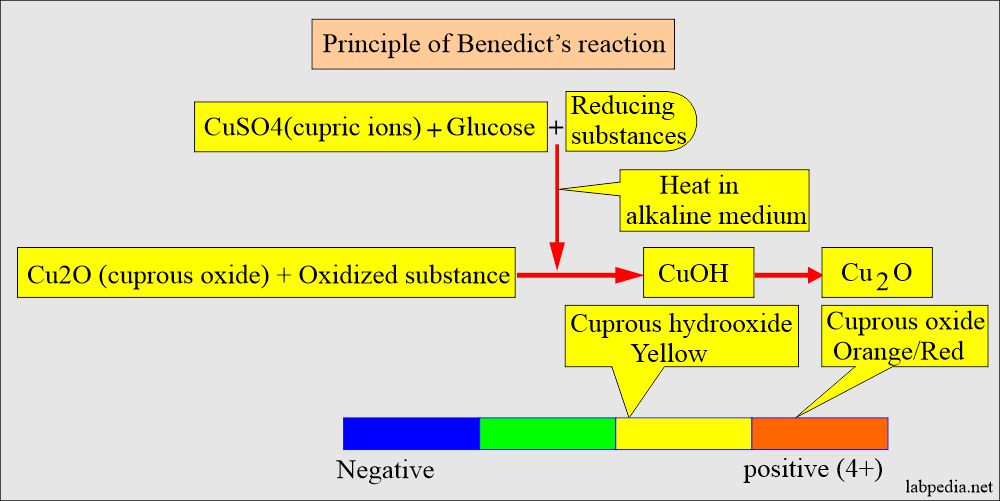
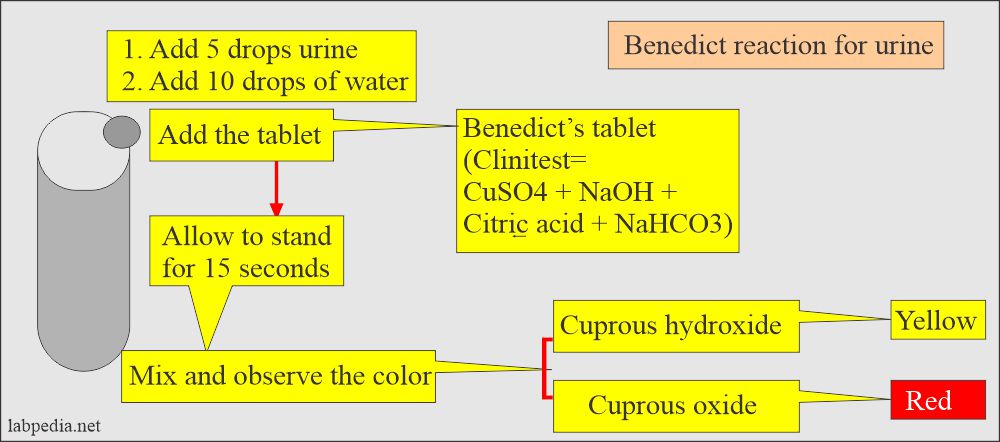
How will you perform the Copper reduction method (Benedict’s reaction)?
- This test was used in the early days.
- An alkaline cupric sulfate solution oxidizes all reducing sugars, such as glucose, galactose, fructose, maltose, xylulose, arabinose, and ribose.
- It forms a brick-red to yellow precipitate of Cu2O.
- This test involves reducing copper sulfate (CuSO4) to cuprous oxide in the presence of an alkali and heat.
- The color depends upon the amount of Cu2O.
- Reading:
- The color changes from blue = Negative (CuSO4).
- Green, yellow, orange/red = Positive 4+ (CuO).
- Greenish = 1+ to Yellow = 4+
- The positive reaction of 1+ = Roughly 50 mg/dL.
- The positive reaction of 4+ = 2 or more g/dL.
What is the principle of Benedict’s reaction?
How will you compare Benedict’s reaction and the Oxidase method?
| Characteristics | Benedict reaction (CuSO4) | Glucose oxidase |
|
|
|
|
|
|
|
|
|
|
|
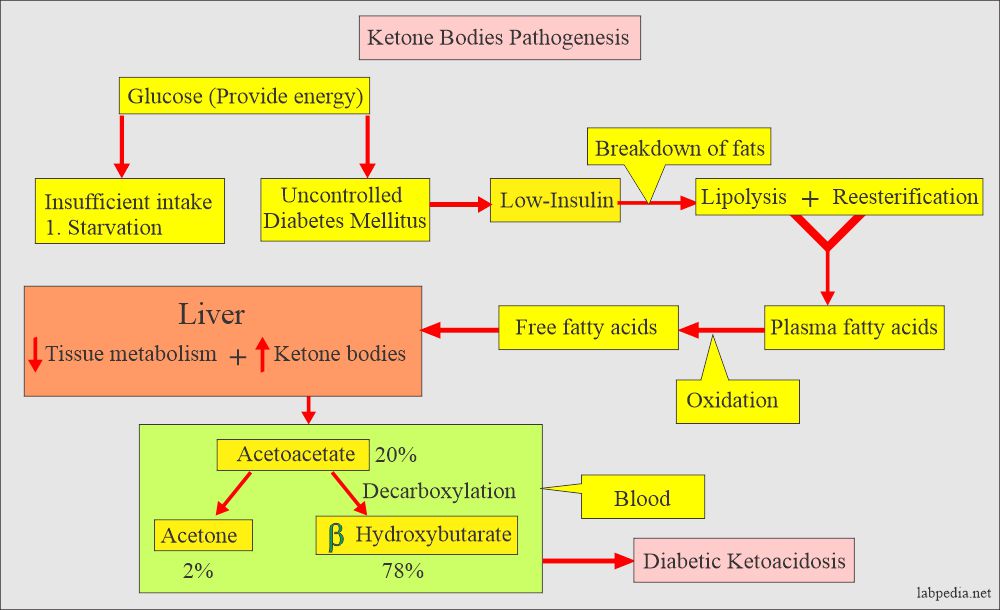
Ketones Bodies in the urine:
How will you define ketone bodies in the urine?
- Ketone bodies are absent in the normal person.
- These are seen in patients with uncontrolled diabetes mellitus.
- These can also be seen in person on a low carbohydrate diet.
- These are seen in people on a high-fat diet.
What are the causes of the ketone bodies?
- Diabetic acidosis.
- Starvation.
- Vomiting.
- Malabsorption syndrome.
- Pancreatic disorders.
- Insulin dosage monitoring.
- Strenuous exercise.
- Inborn error of amino acid metabolism.
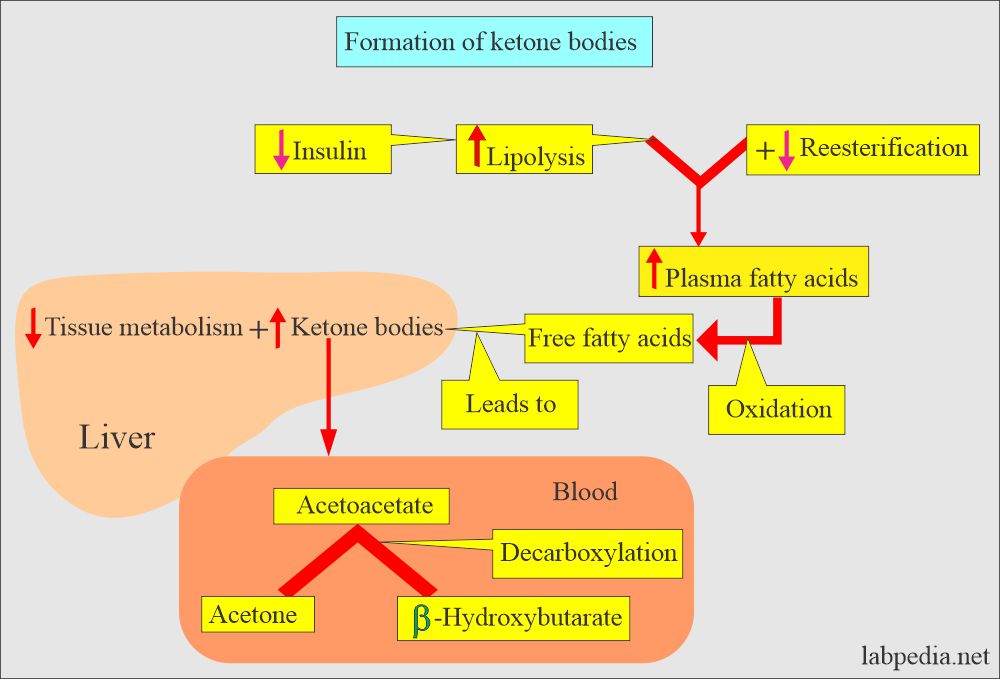
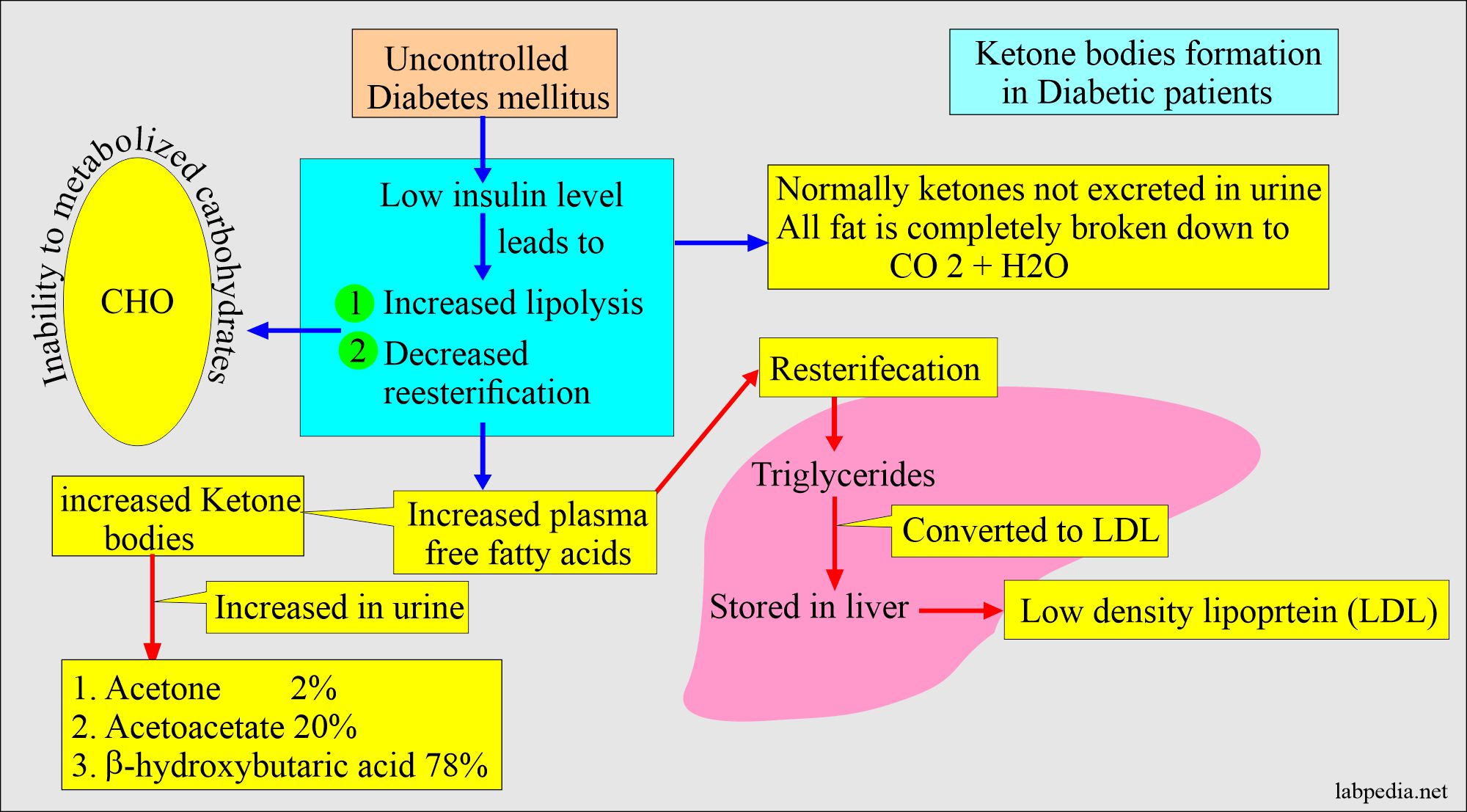
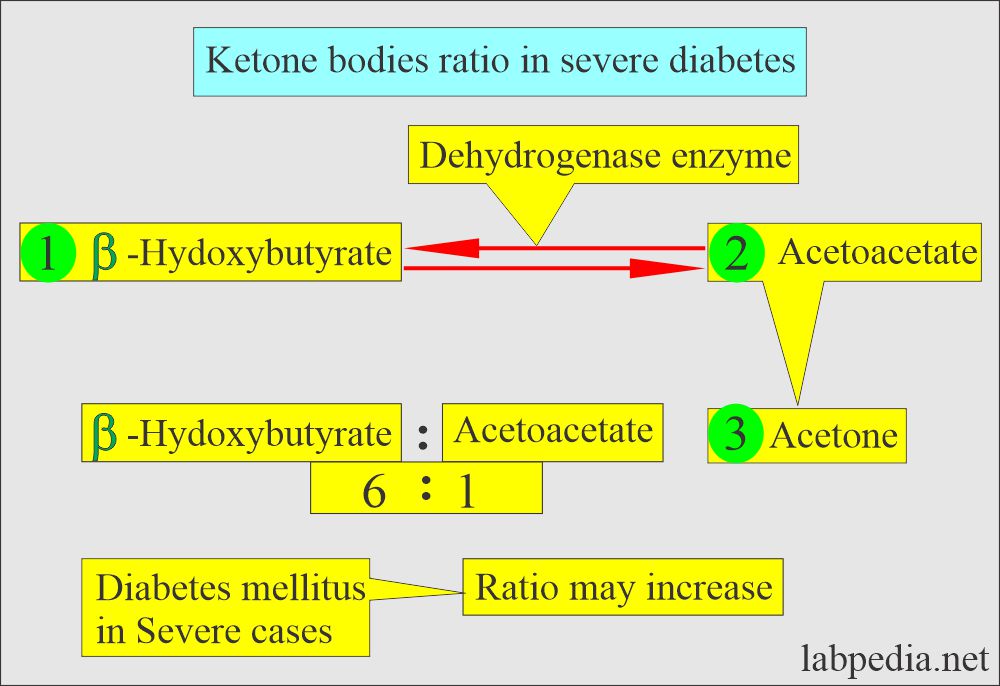
What are the types of ketone bodies?
- Acetone.
- Acetoacetate.
- β-hydroxybutyric acid.
- Ketone bodies are not normally found in urine because all the metabolized fats are completely broken down to CO2 and H2O.
- When the carbohydrate energy source is unavailable, body fat stores are mobilized to supply energy, and ketones are found in the urine.
- Ketone body formation in diabetic patients:
- In diabetic patients, ketonuria shows a deficiency of insulin.
- Adjusting the dose of insulin in diabetic patients is needed.
- The increased amount of ketones in the blood leads to electrolyte imbalance and dehydration.
- If this is not corrected, it leads to acidosis, and ultimately, the patient goes into a coma.
- These ketone bodies’ ratios differ: acetoacetate 20%, acetone 2%, and β-hydroxybutyrate 78%.
What is the normal ketone bodies in the urine?
- These are negative in the random sample.
- Qualitatively, it is also negative.
Urobilinogen in the urine:
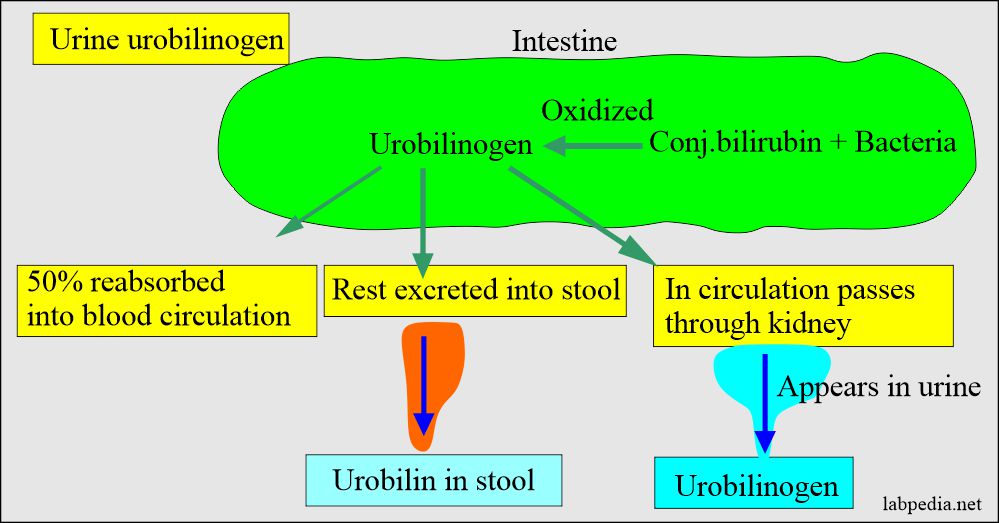
How will you define urobilinogen in the urine?
- It is a colorless compound that forms in the intestine by the bacterial enzyme from the reduction of bilirubin action.
- Normal urine contains small traces of urobilinogen.
- Because of fewer intestinal bacteria, infants have decreased urobilinogen in the urine.
- It is decreased after antibiotic therapy because of the reduced number of intestinal bacteria.
- Urobilinogen is a bile pigment like bilirubin, and hemoglobin degradation forms it.
- It is formed in the intestine from the bilirubin by the action of the intestinal bacteria.
- Most of the urobilinogen is reabsorbed into the blood circulation (enterohepatic circulation), and some of this is excreted through the kidney into the urine.
- It is oxidized to urobilin in the feces and gives a characteristic brown color to stool.
- So, usually, a urine test for urobilinogen is positive. The urine normally contains <1 mg/dL or Ehrlich unit. So, testing for bilirubin and urobilinogen is necessary to diagnose liver diseases.
- Absent urobilinogen in the urine and feces is diagnostic of biliary duct obstruction.
What are the indications for urobilinogen in the urine?
- Early detection of liver diseases.
- Hemolytic diseases.
- Hepatitis and Cirrhosis.
- In carcinomas.
What sample is needed to test the urobilinogen in the urine?
- A fresh urine sample is needed (because it is light-sensitive).
- An ideal sample for detecting or quantitating is a 2-hour early afternoon specimen.
- Keep in mind the diurnal variation.
What will the position of Urobilinogen be in different conditions?
| Urine test | Hemolytic disease of the newborn | Hemolytic anemia | Acute liver cell injury | Chronic liver cell injury | Intrahepatic cholestasis | Biliary obstruction | Cirrhosis |
| Urobilinogen in urine | Mostly absent | Increased (+++) | Increased (+) | Increased(+) | Normal or increased | Decreased or absent (pale stool) | Normal or increased |
Differential diagnosis of urobilinogen in the urine:
| Urine test | In normal person | In liver diseases | In biliary obstruction | In hemolytic anemia |
| Bilirubin | Negative | Positive or negative | Positive (+++) | Negative |
| Urobilinogen | Normal level | Increased (++) | Absent or low | Increased (+++) |
How will you perform the Ehrlich aldehyde reaction for urine?
- This is the test for urobilinogen.
- Perform this test on the fresh urine sample because it is unstable and breaks down into urobilin while keeping the urine.
- This test detects urobilinogen at least at the level of 0.1 mg/dL.
- What is the procedure for the Ehrlich aldehyde reaction?
- The reagent strip is impregnated with p-dimethylamino benzaldehyde and an acid buffer.
- This method may give a false-positive result due to the presence of porphobilinogen.
- Another method uses the Diazonium compound, and it forms a red color.
- Result: Red color in positive cases.
What is the normal urobilinogen in the urine?
- Its level with this method is 0.1 to 1.0 mg/dL.
- The 2 mg/dL level is the cut-off point for the result to be abnormal.
- These are 0 to 4 mg /24 hours.
- Random urine = 0.1 to 1 Ehrlich U/dL or <1 mg/dL.
- 2 hours urine = 0.1 to 1.0 Ehrlich U/2 hours or <1 mg/2 hours.
- 24-hour urine = 0.5 to 4.0 Ehrlich U/24 hours or 0.5 to 4.0 mg/24 hours.
What are the causes of Increased levels of urobilinogen in the urine?
- Hemolytic anemia.
- Pernicious (megaloblstic) anemia.
- Malarial attack.
- Excessive bruising.
- Pulmonary infarction.
- Cirrhosis.
- Acute hepatitis.
- Cholangitis.
What are the causes of a decreased level of urobilinogen in the urine?
- Complete or partial obstruction of the biliary tract.
- Cholelithiasis.
- Biliary duct inflammation.
- Cancer of the head of the pancreas.
- Antibiotic therapy will suppress intestinal bacterial flora.
Bilirubin in the urine:
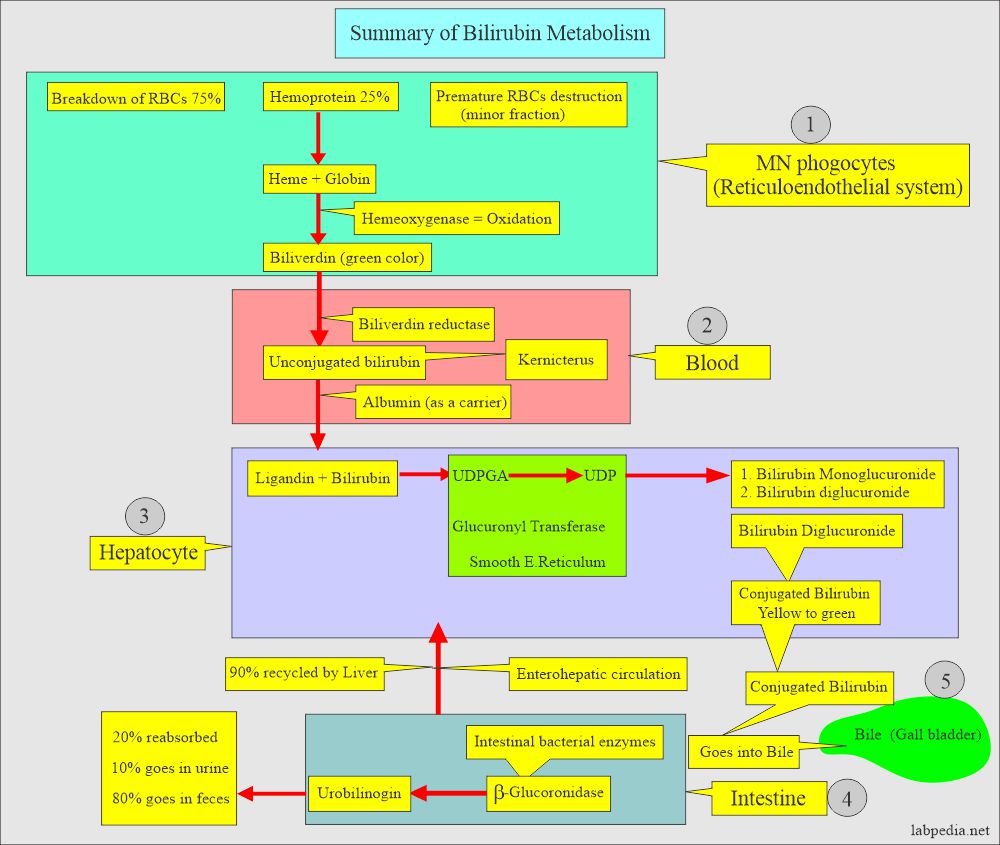
How will you define bilirubin in the urine?
- Bilirubin in the urine is called bilirubinuria.
- This will appear in the urine before the appearance of jaundice.
- Bilirubin is a pigmented yellow compound, a degradation product of hemoglobin.
- The following diagram explains how bilirubin is formed. When production is increased, it may appear in the urine.
- Conjugated bilirubin appears in the urine when the normal degradation cycle is disrupted by obstruction of the bile duct, such as gallstones or cancer.
- Another possibility is when the liver cells are damaged, which allows the leakage of bilirubin directly into the circulation.
- Hepatitis and cirrhosis are common causes of liver cell damage and result in bilirubinuria.
- Increased hemolysis does not produce bilirubinuria.
- Bilirubin in the urine is detected only if the urine sample is fresh because bilirubin decomposes rapidly in bright light.
- If the urine is left in the lab, bilirubin is converted into biliverdin, a green compound by the light not detected by the bilirubin strips.
What is the normal bilirubin level in urine?
- Urine bilirubin is negative (0 to 0.2 mg/dL (0 to 0.34 µmol/L).
- Bilirubin can be detected in urine by the Foam test.
How will you perform the foam test for bilirubin in the urine?
- Place a small urine volume in the test tube, cap it, and shake it vigorously.
- Result:
- The foam at the top is white, which means bilirubin is negative.
- If the foam is orange in color, it means bilirubin is present.
What are the other methods to detect bilirubin in the urine?
- Diazo reaction is in the form of tablets or dipsticks.
- Fouchet’s test.
- Ferric chloride test.
How will you compare Fouchet’s, Ferric chloride, and Diazo’s reactions for Bilirubin?
|
|
|
|
|
|
|
|
|
|
|
|
What are the causes of Increased bilirubin in the urine?
- Hepatitis and liver diseases.
- Obstructive biliary tract disease.
- Liver or biliary tract tumors.
- Septicemia.
- Hyperthyroidism.
Hemoglobinuria:
What are the causes of Hemoglobinuria?
- It may result from the hemolysis of RBCs in the urinary tract, which occurs in dilute and alkaline urine.
- This can also occur in intravascular hemolysis, where hemoglobin filters out through the glomeruli. No RBCs will be seen in the urine.
What is the pathogenesis of hemoglobinuria?
- Under normal conditions, the hemoglobin+haptoglobin complex can not filter out of the glomeruli.
- This happens when the free hemoglobin exceeds the haptoglobin, e.g.
- Hemolytic anemia.
- Transfusion reactions.
- Infection.
- Severe burns.
- Strenuous exercise.
- Malarial infection.
What is the normal hemoglobinuria?
- This is negative.
Myoglobinuria:
How will you define myoglobinuria?
- Myoglobin is a heme-containing protein found in muscle tissue.
- This is seen in the case of rhabdomyolysis.
- The heme portion of myoglobin is toxic to the renal tubules; an increased concentration can lead to renal failure.
- The blood hemolytic transfusion reaction may cause damage to the kidneys and lead to renal failure.
What are the causes of Causes myoglobinuria in the urine?
- Crush syndrome.
- Muscle wasting diseases.
- Trauma.
- Alcoholism.
- Convulsion.
- Extensive exertion.
- Heroin abuse.
How will you summarize hemoglobinuria and myoglobinuria?
| Clinical parameters | Hemoglobinuria | Myoglobinuria |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
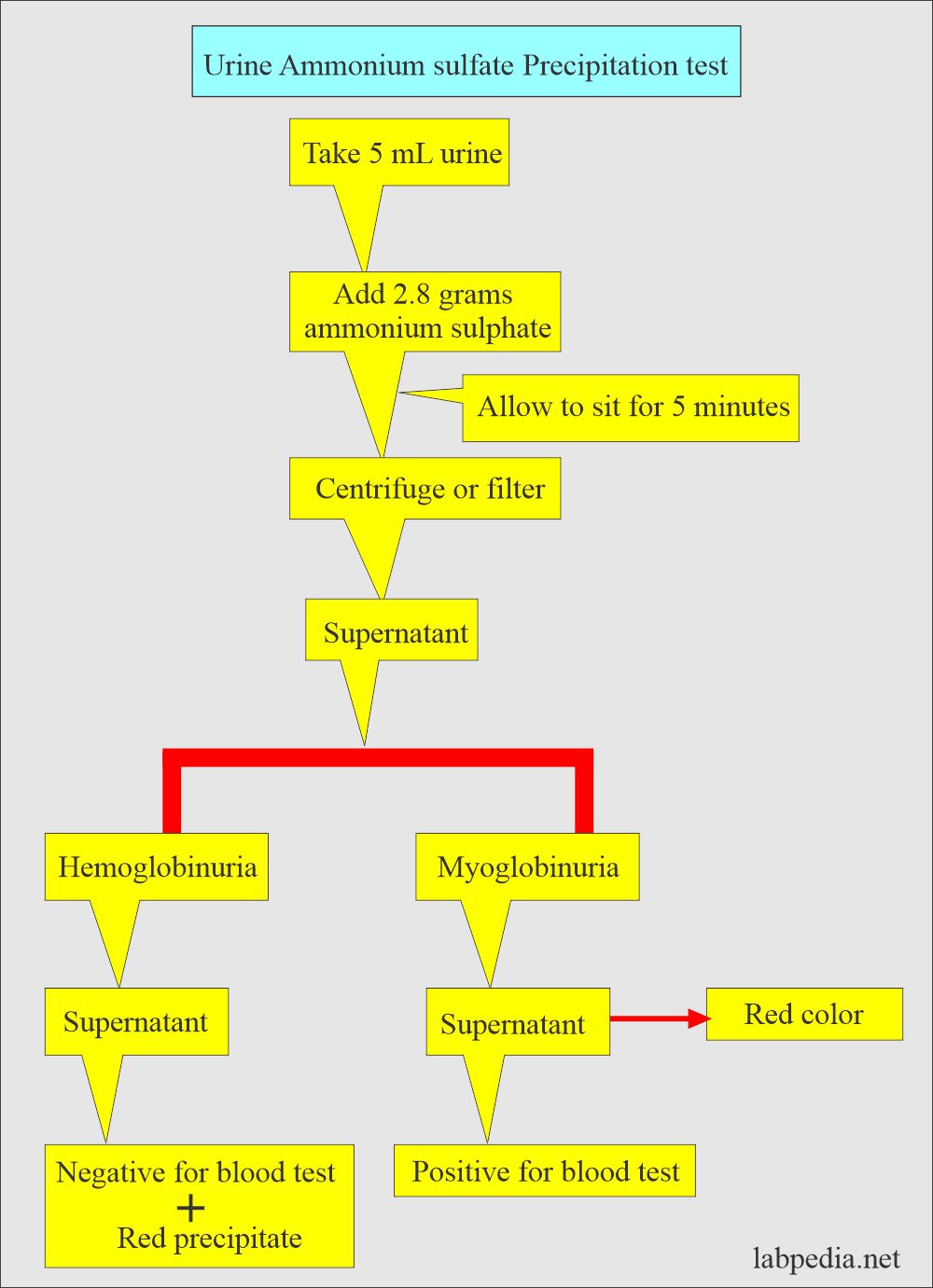
How will the Ammonium sulfate (NH4)2SO4) concentration test be performed?
- It is done to differentiate hemoglobinuria and myoglobinuria:
Phosphorus in the urine:
How will you define Phosphorus in the urine?
- Most of the body’s phosphorus is combined with the calcium in the bones.
- About 15% is present in the blood, making the main intracellular anions.
- The human body contains 620 g of phosphorus, mainly in the form of phosphate.
- The urine HPO4-2: H2PO4– ratio varies widely, from 1: 100 at pH 4.5 to 90:10 at pH 8.0.
- Urine for phosphorus for 24 hours collections needs acid-washed detergent-free containers.
What are the indications for urinary 24-hour phosphorus?
- In hyperparathyroidism.
- In hypoparathyroidism.
- In case of renal loss.
What are the functions of Phosphorus in the body?
- It has a role in glucose and lipid metabolism.
- It helps in the storage and transfers the energy in the body.
- It generates bony tissue.
- It maintains the acid-base balance in the body.
What is the normal phosphorus in urine?
- Serum level = 2.4 to 4.1 mg/dL (0.78 to 1.34 mmol/L).
- Urine = 1 gram /24 hours.
- This also depends on the diet.
- Inorganic phosphate = 20 to 40 meq/L.
Creatinine/Creatine in the urine:
How will you define creatinine in the blood and urine?
- Creatine is synthesized in the liver, pancreas, and kidneys from the amino acids arginine, glycine, and methionine.
- It is transported from blood to muscles, the brain, and other organs, converted to phosphocreatine, and acts as an energy reservoir like ATP.
- Creatinine is the waste product of creatine and phosphocreatine.
- Most of the creatinine is produced in the muscles, proportional to the muscle mass.
- Creatinine enters the blood and is excreted through the kidney.
What are the indications for creatinine in the urine?
- To evaluate kidney diseases.
- During 24- hours of urine collection, refrigerate the urine, and no preservative is needed.
What is normal creatinine in urine?
- 1.0 to 1.6 gm/24 hours.
- Or 15 to 25 mg/ kg body weight/24 hours.
Nitrites/Nitrates in the urine:
How will you define Nitrites/Nitrate in the urine?
- Some of the bacteria from the urinary tract convert Nitrates into nitrite.
- Bacteria containing the enzyme reductase will convert nitrate to nitrite.
- NO3 →NO2 in the presence of a reductase enzyme.
- This test is negative in yeast and gram-positive bacteria.
What is the mechanism of conversion of nitrite to nitrate?
- The reductase enzyme is found in gram-negative bacteria like Enterobacteriaceae.
- This is available as urine reagent strips and detects urinary tract infections.
- Most infections start in the urinary bladder, and from there, it travels to the ureters, tubules, and renal pelvis and reaches the kidneys.
- This is useful for detecting the initial urinary bladder infection called cystitis.
- Cystitis will lead to pyelonephritis as a complication of cystitis, and the result is:
- Renal tissue damage.
- Impairment of renal functions.
- Hypertension.
- Sometimes, it leads to septicemia.
- So, detection of bacteriuria in the early stages and timely treatment will prevent all these complications.
What are the Indications for Nitrate test?
- Cystitis.
- Pyelonephritis.
- Monitoring of the patients who are at high risk for urinary tract infection.
- Monitoring of antibiotic therapy.
- Screening of the urine culture specimens.
- These are negative.
- A negative result does not rule out bacteriuria.
- A gram-positive pathogen does not produce a nitrate-reducing substance like:
- Staphylococcus.
- Enterococcus.
- Streptococcus.
Sodium in the urine:
How will you define sodium in the urine?
- Sodium is the primary regulator for retaining or excreting water and maintaining acid-base balance.
- Sodium also maintains the normal electrolytes’ intracellular and extracellular balance.
- This will take place along with potassium under the effect of aldosterone.
What are the Indications for urinary sodium?
- Electrolytes imbalance.
- Acute renal failure.
- Hyponatremia.
- Oliguria.
- Na+ excreted for diagnosis of renal and adrenal imbalance.
- No preservative is needed for the collection for 24 hours; only refrigerate during the collection.
What are the causes of increased sodium in urine?
- Addison’s disease (adrenal failure, primary and secondary).
- Renal tubular acidosis.
- Diabetic acidosis.
- Tubulointerstitial disease.
- Salt-losing nephritis.
- Barrter’s syndrome.
What are the causes of decreased urinary sodium?
- Excessive sweating and diarrhea.
- Prerenal azotemia.
- Cushing’s syndrome.
- Primary aldosteronism.
- Congestive heart failure.
- Nephrotic syndrome with acute oliguria.
What is the normal sodium in urine?
- Adult = 40 to 220 meq/24 hours urine (40 to 220 mmol/day)
- Child = 41 to 115 meq/24 hours urine (41 to 115 mmol/day)
- Value is dependent on salt intake.
Potassium in the urine:
How will you define Potassium in the urine?
- Potassium acts as a body buffer system and plays an important role in maintaining electrolyte balance.
- The potassium study is helpful for the study of renal and adrenal disorders.
- Potassium in the urine is in the form of KCL, K2SO4, and K2PO4 salts.
- K+ values <20 meq/L are associated with nonrenal causes.
- K+ >20 meq/L are associated with renal causes.
What are the indications for K+ estimation in the urine?
- To evaluate the electrolyte imbalance.
- Renal disorders.
- Adrenal glands disorder.
- No preservative is needed for urine collection for 24 hours; only refrigerate the sample during collection.
What is the normal potassium in urine?
- Adult = 25 to 125 meq/24 hours urine (25 to 125 mmol/day).
- Child = 10 to 60 meq/24 hours urine (10 to 60 mmol/day)
- Values are diet-dependent.
What are the causes of increased urinary K+?
- Diabetic and renal tubular acidosis.
- Primary renal diseases.
- Cushing’s syndrome.
- Starvation.
- Primary and secondary aldosteronism.
- Fanconi’s syndrome.
- The onset of metabolic alkalosis.
What are the causes of decreased urinary K+?
- Addison’s disease.
- In patients with K+ deficiency.
- Pyelonephritis and glomerulonephritis.
Calcium in the urine:
How will you define Calcium in the urine?
- The parathyroid gland hormones maintain calcium hemostasis.
- An adequate amount of calcium is excreted in the stool, and a small amount is in the urine.
- Calcium absorption is dependent upon dietary calcium intake.
What are the indications for calcium in the urine?
- To evaluate the calcium intake.
- To assess the rate of absorption from the intestine.
- To find resorption from the bone.
- To evaluate the renal loss.
What is the normal calcium in urine?
- Normal diet = 100 to 300 mg/24 hours (2.50 to 7.50 mmol/day)
- Low calcium diet = 50 to 150 mg/24 hours (1.25 to 3.75 mmol/day)
- Another source:
- 5 to 12 meq/L
- < 150 mg/ 24 hours on a low-calcium diet.
- Or o.3 g/24 hours of urine.
What is the mechanism of increased calcium in urine?
- Increased intestinal absorption.
- A lake of renal tubular reabsorption.
- Resorption or loss of calcium from the bones.
- Or a combination of the above mechanisms.
- Calcium is present in urine as CaCl2, CaSO4, and CaPO4 salts.
- Urinary calcium does not have much value in the differential diagnosis of diseases.
What are the causes of increased urine calcium?
- Hyperparathyroidism in 30 to 80% of the cases.
- Paget’s disease.
- Renal tubular acidosis.
- Vitamin D intoxication.
- Fanconi’s syndrome.
- Idiopathic hypercalciuria.
- Osteoporosis.
- Osteitis deforms.
- Sarcoidosis.
- Bone metastasis in osteolytic type.
- Multiple myeloma.
- Thyrotoxicosis.
What are the causes of decreased urinary calcium?
- Hypoparathyroidism.
- Vitamin D deficiency.
- Metastatic carcinoma of the prostate.
- Preeclampsia.
- Malabsorption syndrome:
- Celiac disease.
- Steatorrhea.
- Sprue disease.
- Renal osteodystrophy.
- Renal failure, acute nephrosis, and nephritis.
- Vitamin-D resistant Rickets.
Chloride in the urine:
How will you interpret chloride in the urine?
- Chloride is most often associated with sodium balance and fluid changes.
- Mostly, urinary excretion of chloride is parallel to the dietary intake.
- This also reduces dietary salt intake, especially in patients with cardiovascular, hypertension, kidney, and liver diseases.
What are the indications for chloride in the urine?
- It is advised in electrolyte imbalance.
- In the case of dehydration.
- In metabolic alkalosis.
- No preservative is needed to collect the urine; only refrigerate the samples.
What is the normal chloride in urine?
- Children’s values are much lower than adult values.
- The values vary with the salt intake and perspiration.
- The values vary from different lab values.
Age Value in 24 hours of urine - Child <6 years
- 15 to 40 meq/day (15 to 40 mmol/day)
- Children 10 to 14 years
- 64 to 176 meq/day (64 to 176 mmol/day
- Adult
- 140 to 250 meq/day (140 to 250 mmol/day)
Magnesium in the urine:
How will you interpret magnesium in the urine?
- Magnesium excretion through the urine controls the blood magnesium level.
- Urinary excretion of magnesium is dependent upon dietary intake.
- If somebody takes 200 to 500 mg/day, urinary excretion of magnesium is 75 to 150 mg/24 hours (3 to 6 mmol/day).
What are the indications for magnesium in the urine?
- It is advised in magnesium metabolism.
- Electrolytes balance.
- Advised in nephrolithiasis.
- For the 24-hour urine sample, 20 mL of 6N HCL in a metal-free container is needed. The sample should also be refrigerated.
What is the normal magnesium in urine?
- Urine = 75 to 150 mg/24 hours
- urine = 3.0 to 6.0 meq/24 hours (3.0 to 6.0 mmol/day)
- 2 to 12 meq/L
What are the causes of increased urine magnesium?
- Chronic glomerulonephritis.
- Increased level of blood alcohol.
- Bartter’s syndrome.
What are the causes of decreased urine magnesium?
- Magnesium deficiency.
- Malabsorption.
- Chronic renal diseases.
- Hypoparathyroidism.
- Hypercalciuria. It is seen in long-term parenteral therapy.
- Decreased renal function like Addison’s disease.
Amino acids in the urine:
How will you interpret amino acids in the urine?
- Free amino acids are found in the urine and acid filtrate of the protein-containing fluids.
- This test is advised when there are suspected genetic abnormalities, patients with mental retardation, reduced growth, or unexplained symptoms.
What are the indications for an amino acid in urine?
- This is advised for the screening of the inborn error of metabolism.
- Advised for genetic abnormalities.
- No preservative is needed to collect the 24 hours of urine; only refrigerate while collecting the samples.
What are the normal amino acids in urine?
- Negative.
The details are seen in part 1, complete urine analysis.



Ethiopia
Your question is not clear to me.