TORCH Profile:- Part 3 – Herpes simplex (Herpesvirus type 1 and type 2)
Herpes simplex (Herpesvirus Type 1 and Type 2)
What sample is needed for the TORCH profile?
- The venous blood is collected to prepare the serum.
- The other samples used are blood, urine, and spinal fluid for evidence of the infections for TORCH.
- Diagnosis can be confirmed by the culture of one of the specific pathogens or by increased levels of IgM against the specific pathogen.
What are the Indications for the TORCH profile?
- TORCH profile is done to find the cause of premature birth or abortion.
- TORCH screens infants for toxoplasmosis, cytomegalovirus, herpes simplex, rubella, and syphilis.
What is the Pathophysiology of TORCH?
- TORCH profile includes the following tests :
- Toxoplasmosis antibody.
- Rubella antibody.
- Herpes Simplex.
- Cytomegalovirus
- Some people include syphilis as well.
- These infections may lead to birth defects, growth delays, and problems in the baby’s brain and nervous system.
- If TORCH screening on infants is positive, more testing will be needed to confirm the diagnosis. The mother will also need to be checked.
- The test is ordered when a pregnant woman is suspected of having any of the TORCH infections.
- These infections can be serious during pregnancy because they can cross the placenta from the mother to the developing fetus and cause congenital defects in the newborn.
- The TORCH infections cause a syndrome characterized by:
- Microcephaly.
- Sensorineural deafness.
- Chorioretinitis.
- Hepatosplenomegaly.
- Thrombocytopenia.
- TORCH infection signs/symptoms are:
- Fever and poor feeding.
- The newborn is often small for gestational age.
- A petechial rash on the skin may be present, with small reddish or purplish spots due to bleeding from capillaries under the skin.
- An enlarged liver and spleen (hepatosplenomegaly) are common, as jaundice.
- Hearing impairment, eye problems, mental retardation, autism, and death can be caused by TORCH infections.
- The mother often has a mild infection with few or no symptoms.
- The examiner may test blood, urine, and spinal fluid for evidence of the infections for TORCH.
- Diagnosis can be confirmed by the culture of one of the specific pathogens or by increased levels of IgM against the pathogen.
Herpes simplex virus (HSV)
What sample is needed for the diagnosis of Herpes simplex?
- A blood sample to prepare the serum is needed.
- Can take the swab for culture from the vesicles.
- Direct cytologic scrapings of the lesion (Wright-Giemsa stain).
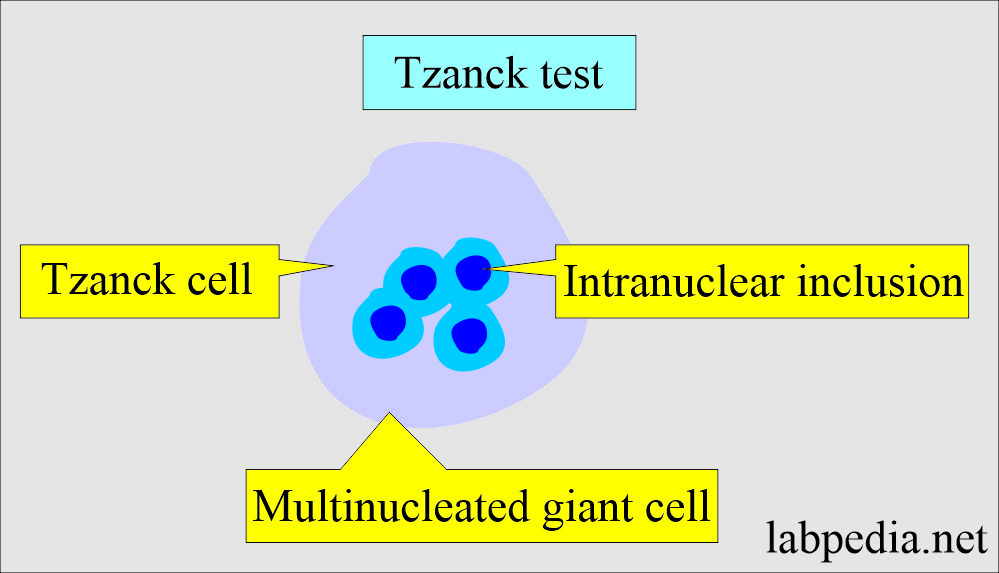
- There are multinucleated giant cells with intranuclear inclusions (Tzanck test).
- Antigen detection (EIA or direct fluorescence) from vesicles and ulcers.
- PCR to find DNA in tissue, CSF, or cell samples.
How will you define Herpes Simplex?
- Herpes is a Greek word meaning creep, referring to spreading skin lesions.
- The Herpes virus is a double-stranded DNA virus. The Herpes family is Herpesvirdae.
- The natural habitat is human, and this disease is present worldwide.
- Herpes simplex infection is characterized by a primary infection that is usually asymptomatic.
- This virus settles in the dorsal root ganglia and remains dormant.
- The absence of a pre-existing antibody characterizes primary infection.
- Primary infection is contracted by close contact with the infected person.
What are the diseases caused by the Herpes virus group?
| Type of the virus | Geus of the virus | Clinical diseases |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you discuss the microbiology of Herpes simplex virus (HSV)?
- There are five human herpesviruses:
- Herpes simplex 1.
- Herpes simplex 2.
- Varicella-zoster.
- Epstein-Barr virus.
- Cytomegalovirus.
- Another reference divides herpes viruses into:
- Alpha virus:
- Herpes simplex virus (HSV-1).
- Herpes simplex 2 (HSV-2).
- Varicella zoster
- Beta virus:
- Cytomegalovirus (CMV).
- Gamma virus:
- Epstein-Barr virus (EBV)>
- Human Herpes virus-6 (HHV-6).
- Herpes simplex exists in two forms :
- Herpes Simplex type 1.
- Herpes Simplex type 2.
- Virtually all adult sera are positive for Herpes antibodies to one of the types.
- Even antibody-positive individuals may experience repeated infection attacks, so antibodies are not a useful indicator of immunity.
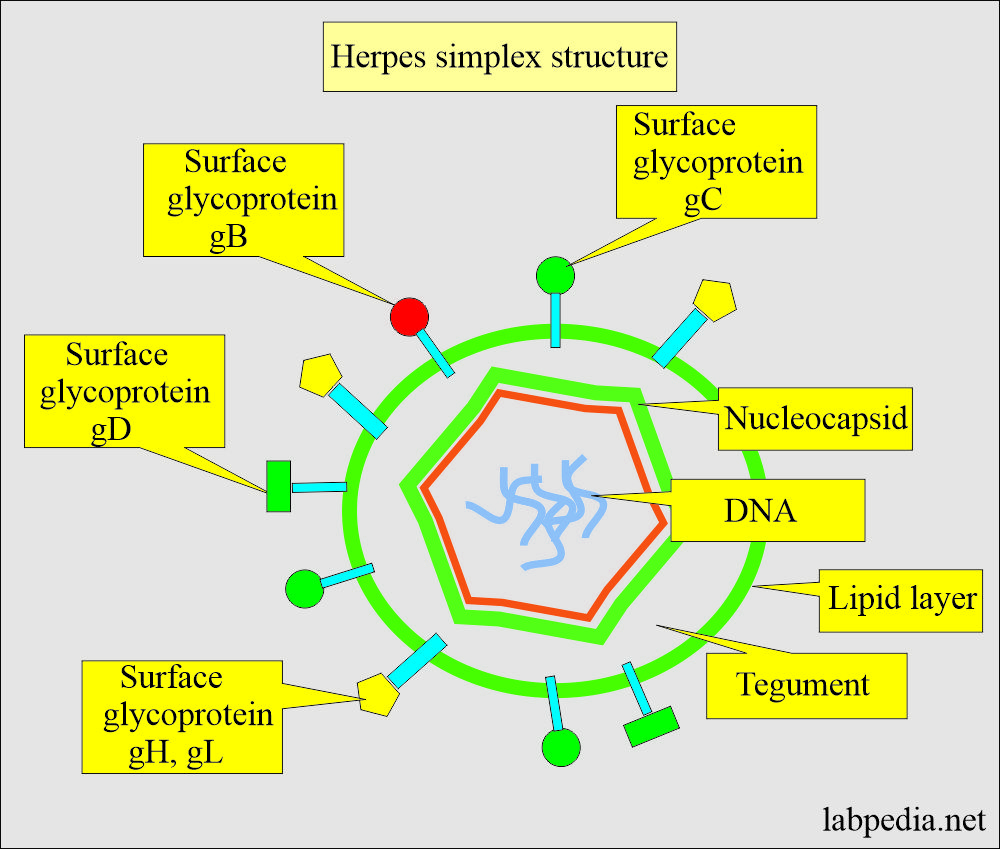
What is the structure of Herpes Simplex (HS)?
- The size of the virus is 100 to 200 nm.
- These are double-stranded DNA viruses.
- These are icosahedral in shape.
- There is a lipid envelope.
What is the mechanism of the damage by Herpes simplex?
- Herpes virus (DNA) integrates with the host cells.
- Produce latent infection in lymphoid cells and ganglia of the brain.
- The virus keeps latency within nerve cells after primary infection, which may activate when the patient is stressed.
- Congenital infection due to HSV-2 may occur in the newborns of mothers who have genital herpes.
What is the pattern of Herpes infection?
- The portal of the virus entry is respiratory, cutaneous, intravascular, and transplacental.
- Herpes infection presentation is:
- Neonatal sepsis.
- Local skin lesions.
- Pharyngitis.
- Oesophagitis.
- Pneumonia.
- Cervicitis.
- Hepatitis.
- Congenital infection.
- Herpesvirus 1 (HSV-1):
- HSV 1 is primarily responsible for oral lesions and blisters on the mucus membrane of the lip, which are called ” cold sores or canker sores.”
- Also, there may be a corneal lesion like keratitis.
- There may be a focal lesion of the finger called whitlow.
- There may be encephalitis, most frequently involving the temporal lobe.
- Immunocompromised patients may develop disseminated disease.
- In the past, 90% of the population tested positive for HSV-1 antibodies. Now, this incidence has fallen.
- Herpesvirus 2 (HSV-2)
- It involves genital areas.
- The incubation period is 5 to 7 days (the range may be 1 to 45 days).
- It is also called venereal disease.
- This is a sexually transmitted viral infection of the urogenital area.
- A vesicular lesion exists on the penis, scrotum, vulva, perianal region, perineum, vagina, and cervix.
- In the USA, in sexual clinics, HSV-2 is found in 20% to 50% of genital ulcerations.
- 85% of the cases with genital lesions have a recurrence.
- The patients develop systemic symptoms like fever, myalgia, malaise, and headache.
- Herpes simplex 2 (HSV-2) can be cultured from the cervix in 80% to 90% of cases.
- 80% of the patients develop inguinal lymphadenopathy in the second or third week.
- Acute disease:
- The acute disease presents as acute gingivostomatitis (Aphthous stomatitis).
- This is seen in early childhood. There are vesicular lesions and fever.
- The dormant stage is when the virus is dormant after the primary infection.
- The virus remains dormant in the sensory ganglia of the trigeminal nerve.
- Eczema Herpeticum will complicate infantile eczema.
- Keratoconjunctivitis is due to a primary or recurrent infection.
- Aseptic meningitis or encephalitis. The majority of these patients have high mortality, reaching 70%.
- Herpetic whitlow occurs when accidental injuries injure doctors, nurses, and dentists.
- Hass’s disease or disseminated Herpes of the newborn.
- It occurs in the mother from the infected birth canal lesions.
- Or it may get an infection from the transplacental spread.
- Mortality is very high, and infants may die in a few days.
- Vulvovaginitis is seen in children and adults.
- Herpes type- 2 may cause genital herpes.
- This remains dormant in the ganglia of the sacral plexus.
- Congenital infection:
- 70% to 80% of neonates who are infected are born to mothers who are asymptomatic at the time of delivery.
- These neonates may develop the following:
- Microcephaly.
- Chorioretinitis.
- Mental retardation.
- Disseminated neonatal herpes viral infection leads to a high incidence of mortality.
- In the case of herpes infection in pregnant women, avoid vaginal delivery, and a cesarean section is advised.
What is the normal Herpes simplex?
- Culture shows no virus.
- Negative Herpes antigen or antibody.
How will you diagnose Herpes simplex?
Cytologic examination:
- Tzanck test:
- Make a smear by scraping from the lesion.
- Or make the smear from the vesicle fluid.
- The skin vesicle is positive at 66%, and the fluid culture is 100% positive.
- Stain it with Wright-Giemsa stain.
- Look for multinucleated giant cells with intranuclear inclusions.
- Tzanck test gives a quick diagnosis but does not differentiate between Herpes simplex type 1 and 2 and Zoster cells.
- Viral testing should be done on the couple to rule out the presence of herpes infection.
- Although accuracy is not great.
- The smear stained with PAP from the urethra and cervical canal shows viral inclusions and multinucleated giant cells.
- It can isolate the virus from the vesicles, ulcers, saliva, and CSF.
What are the serological tests to diagnose herpes simplex infection?
- These are easy and more convenient.
- The advantage of these antigen tests is that the results are available daily.
- While the antibody tests are cumbersome, they require a repeat blood test in acute and convalescent patients.
- If the titer increases, it is significant. A fourfold rise in the titer indicates acute infection.
- These patients always have high titers.
- The peak level after the infection is between 4 to 6 weeks.
- Later on, the level is low.
- In the USA, >50% of the population is positive for herpes antibodies.
- Methods used are:
- Enzyme immunoassay (EIA).
- Indirect immunofluorescence (IIF).
- Indirect hemagglutination test.
What are the culture tests to confirm the Heerpes Simplex virus?
- It is the best method to confirm herpes infection.
- Culture is 90% positive in the positive cases.
- Culture-positive cases are only 85% for the serological tests.
- The culture of the vesicle and ulcer area is a more accurate method.
- Method to take a sample:
- Sample from the urethra for culture:
- Insert the sterile swab in the urethra and rotate gently.
- Keep the patient in a lying position and check the Blood pressure, bradycardia, sweating, nausea, and weakness.
- Sample from the cervix for culture:
- A sterile speculum is inserted in the lithotomy position in the vagina.
- Remove the cervical mucus with a sterile cotton swab.
- Take a sample from the endocervical canal for culture.
How will you diagnose Herpes simplex virus in pregnant women?
- The cervix is cultured weekly, beginning 4 to 6 weeks before the due date.
- Vaginal delivery is possible if:
- The two most recent cultures are negative.
- There is no lesion in the vagina and vulva.
- There are no clinical symptoms in the pregnant lady.
- If, throughout the pregnancy, the lady has had no more than one culture-positive and no symptoms.
Questions and answers:
Question 1: What disease will be caused by Herpes simplex type 1?
Question 2: What disease will be caused by Herpes simplex type 2?