TORCH Profile:- Part 1 – Rubella virus (German Measles)
Rubella virus (German Measles)
What sample is needed for the TORCH profile?
- Venous blood is collected to prepare the serum.
- The other samples used are urine and spinal fluid for evidence of the infections for TORCH.
- Diagnosis can be confirmed by the culture of one of the specific pathogens or by increased levels of IgM against the specific pathogen.
What are the Indications for the Rubella virus?
- TORCH profile is done to find the cause of premature birth or abortion.
- TORCH profile is used to screen infants for infections such as toxoplasmosis, cytomegalovirus, herpes simplex, rubella, and syphilis.
How will you define the TORCH profile?
- TORCH profile includes the following tests:
- Toxoplasmosis antibody.
- Rubella antibody.
- Herpes Simplex.
- Cytomegalovirus
- Some people include syphilis as well.
- These infections may lead to birth defects, growth delays, and problems in the baby’s brain and nervous system.
- If TORCH screening on infants is positive, more testing will be needed to confirm the diagnosis. The mother will also need to be checked.
- The test is ordered when a pregnant woman is suspected of having any of the TORCH infections.
- These infections can be serious during pregnancy because they can cross the placenta from the mother to the developing fetus and cause congenital defects in the newborn.
What are the complications of TORCH infection?
- The TORCH infections cause a syndrome characterized by:
- Microcephaly.
- Sensorineural deafness.
- Chorioretinitis.
- Hepatosplenomegaly.
- Thrombocytopenia.
What are the signs/symptoms of TORCH infection?
- Fever and poor feeding.
- The newborn is often small for gestational age.
- A petechial rash on the skin may be present, with small reddish or purplish spots due to bleeding from capillaries under the skin.
- An enlarged liver and spleen (hepatosplenomegaly) are common, such as jaundice.
- Hearing impairment, eye problems, mental retardation, autism, and death can be caused by TORCH infections.
- The mother often has a mild infection with few or no symptoms.
- The examiner may test blood, urine, and spinal fluid for evidence of the infections for TORCH.
- Diagnosis can be confirmed by the culture of one of the specific pathogens or by increased levels of IgM against the pathogen.
Rubella Virus
What sample is needed for the Rubella virus?
- The virus may be isolated from CSF, urine, amniotic fluid, and other sites.
How will you define the Rubella virus?
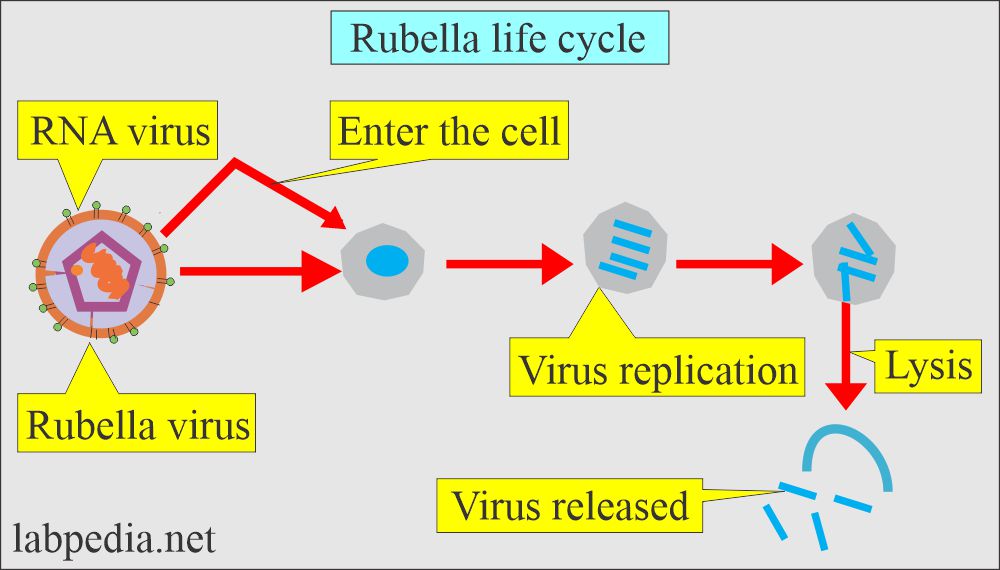
- This is a single-stranded RNA virus (Rubivirus).
- It is quite a common infection in childhood.
- It is important due to its infection in the first trimester of pregnancy and fetus abnormalities.
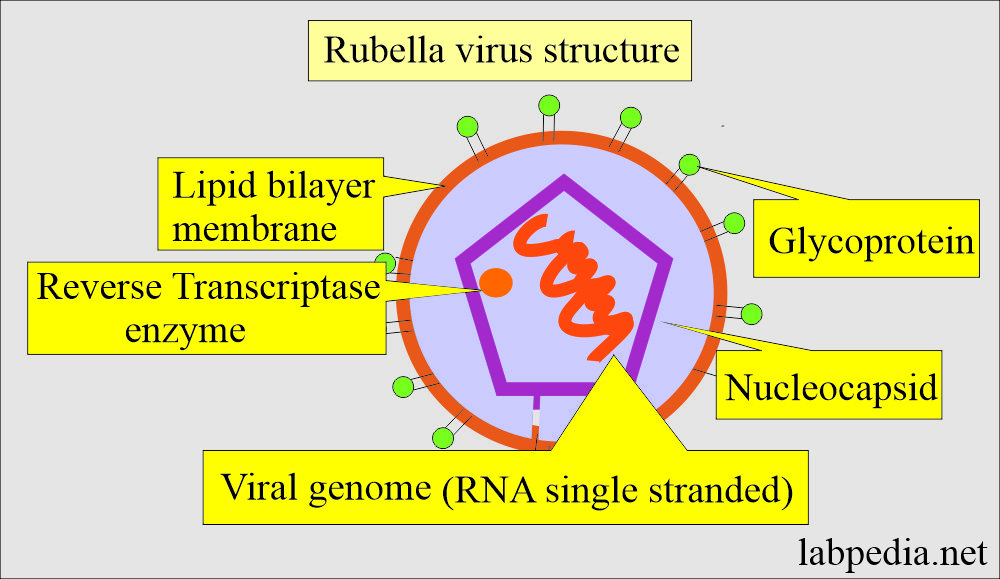
What is the structure of the Rubella virus?
- It is a single-stranded RNA virus.
- Rubella Viron is spherical with a diameter of 60 to 70 nm.
- It comprises capsid protein (C) and two glycoproteins (E1 and E2).
- E1 molecular weight is 58,000, and E2 has 42,000 to 47,000.
- These E1 and E2 are glycosylated and located on the viral surface membrane.
- The incubation period is about 14 days, and the range is 10 to 23 days.
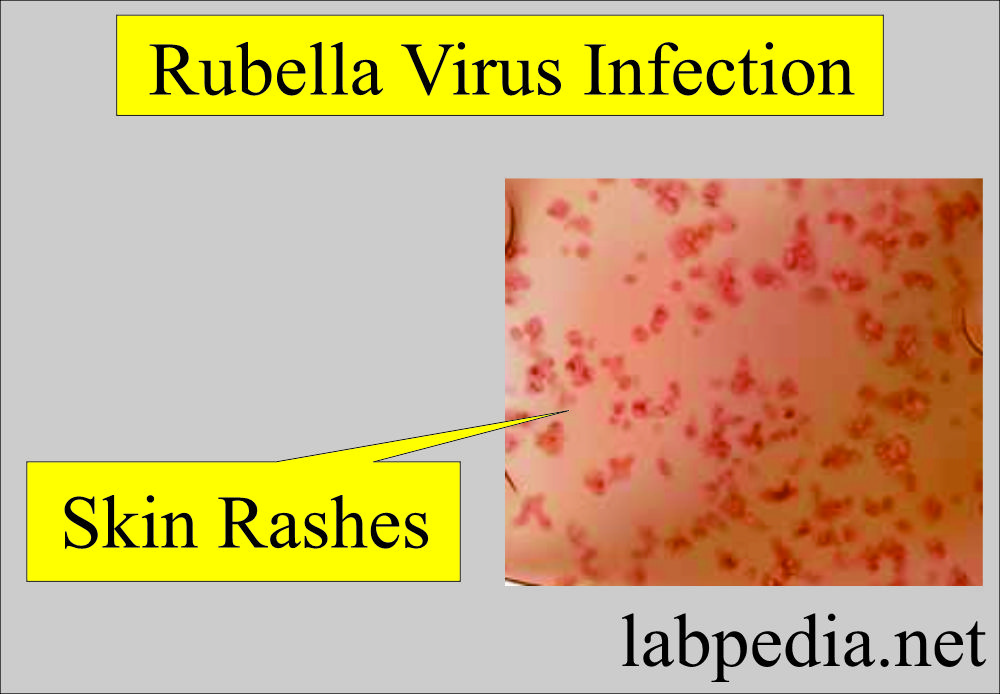
- It is followed by a rash that lasts about three days.
How will you interpret the Rubella virus infection?
- Rubella is not a serious disease and is also called German measles.
- This is also called 3-day measles.
- The incubation period is around 14 days.
- These patients are contagious for about two weeks, ranging from 12 to 21 days.
- There are fever and transient rashes in children and adults.
- The illness may be subclinical in about 25% of the cases. This stage is also infective.
- Infection during the first 16 weeks of pregnancy presents major risks for the unborn baby.
- When a pregnant woman has a rash and other symptoms of rubella, laboratory tests are required to make the diagnosis.
- This is effective in the first trimester of pregnancy.
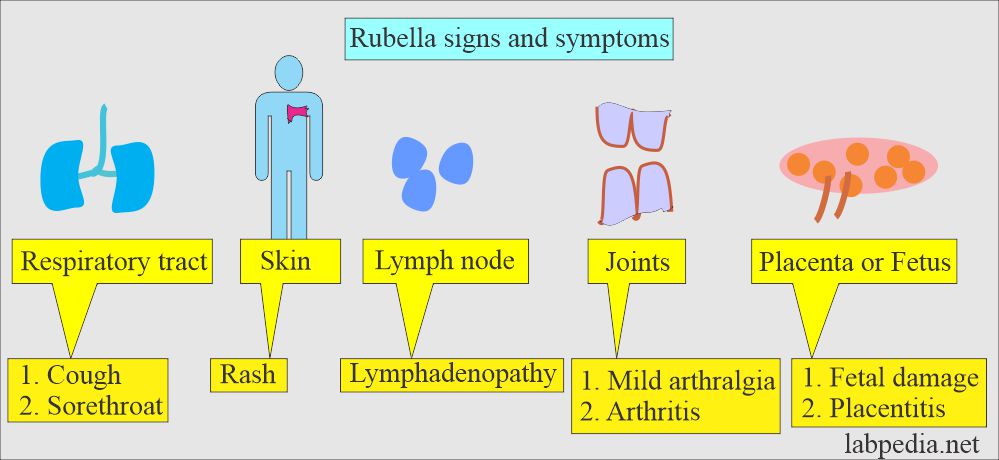
What are the signs and symptoms of Rubella virus infection?
- 25% to 50% of the Rubella infection is asymptomatic.
- There is exposure to the infected patient with Rubella 14 to 21 days before the onset.
- There are lymphadenopathy and postauricular and cervical lymph nodes before the rash appears.
- Post-natal Rubella:
- It is usually asymptomatic in 50% of the cases.
- The post-natal infection has a fever and malaise.
- There is suboccipital adenitis.
- Polyarthritis occurs in 25% of cases. It usually subsides in one week but may persist for weeks. Rarely, chronic arthritis develops.
- A fine, pink maculopapular rash appears on the face, trunk, and extremities. It fades quickly and may be lost in one day in each area.
What are the complications of Rubella virus infection?
- The first trimester of the infection is associated with congenital abnormalities, abortion, or stillbirth in 30% of the patients.
- <80% of patients show this association during the first month.
- 25% to 50% of the cases are subclinical.
- Affected infants show various pathologies like cataracts, microcephaly, deafness, and heart defects.
- There is a chance of spontaneous abortion and stillbirth.
Congenital Rubella virus infection (Rubella syndrome):
What are the Signs and symptoms of congenital Rubella infection?
- The infant may be asymptomatic at birth.
- Later on, these babies may have cataracts and glaucoma.
- They may have microphthalmia.
- There is a hearing defect.
- There is psychomotor retardation.
- There may be heart anomalies like patent ductus arteriosus.
- The patient may have organomegaly.
- There are maculopapular rashes.
- The earlier a newborn gets an infection, the more severe the signs and symptoms.
- Deafness is seen when a fetus gets an infection in the second trimester.
- There may be cerebral damage.
- There may be abortion or stillbirth.
How will you diagnose congenital Rubella infection?
- Infants with congenital rubella infection can produce both IgM and IgG antibodies before birth.
- These antibodies appear in the second trimester of fetal life.
- In addition, fetuses get passive maternal IgG antibodies.
- When infants get to the age of 6 to 8 months, maternal antibodies disappear. The presence of antibodies IgM or IgG indicates congenital or neonatal infection.
- The presence of IgM antibodies is diagnostic of intrauterine life infection.
How will you diagnose Rubella virus infection?
- ELIZA tests for IgM and IgG are >97% positive and are sensitive and specific.
- ELIZA IgG titer 1:10 confirms immunity. It is present in>90% of the American population.
- ELIZA lower titer is considered nonimmunie.
- After vaccination, high levels last for 8 to 12 weeks.
- This virus can be cultured from the nasopharynx; the best place is the posterior end of the nose.
- After the onset of the rash, no need for culture. Now, serological tests are enough.
- Commercial antigen kits are not available.
- Antibodies kits are available as:
- Hemagglutination inhibition.
- Indirect hemagglutination.
- ELISA. This test is more reliable.
- Most IgG kits are available. Few companies are making for IgM.
- Few kits detect both IgG and IgM.
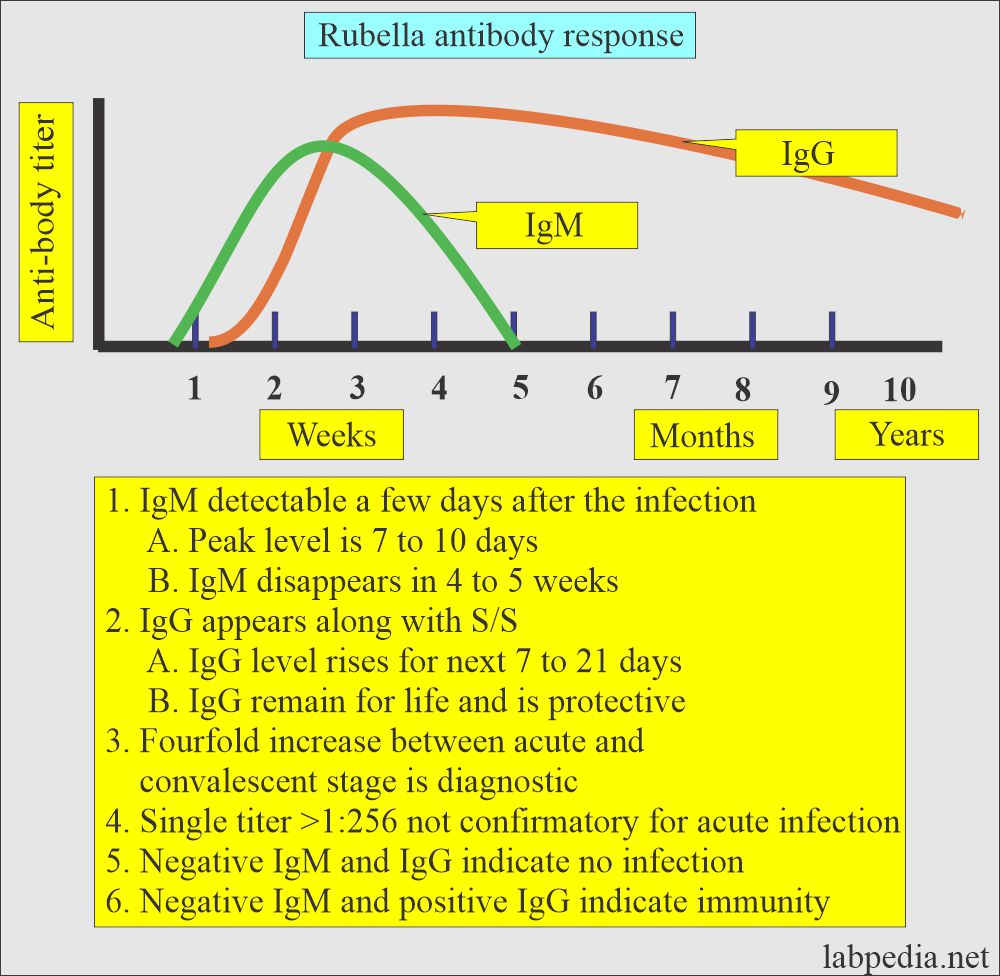
- IgM antibody:
- It is diagnostic in the newborn.
- Congenital rubella in the first trimester is associated with congenital fetal abnormalities, like heart defects, brain damage, and deafness.
- Evidence of active infection in the mother.
- IgM appears 11 to 25 days after the onset of skin rash in all patients, and it persists for <1 year.
- IgM is detected 15 to 25 days after vaccination in <80% of the cases.
- In congenital infection, IgM can be detected at birth and persists for <6 months in 90% of newborns.
- During the first 6 months of a newborn, IgM is the best test for congenital or recent infection.
- After 7 months, the patient is assessed for persistent IgG level.
- IgG antibody:
- IgG appears after 15 to 25 days of the infection.
- It appears after >25 to 50 days of the vaccination.
- <1/3 of the cases may not show IgG antibodies after 10 years of infection.
- The absence of IgG antibodies in newborns excludes congenital infection by Rubella.
- Summary of antibody tests:
- If a woman’s titer is greater than 1:10 to 1:20, she is not susceptible to rubella infection.
- If the titer is <1:8, it indicates she has no immunity to the rubella virus.
- A fourfold rise in the titer in 2 weeks indicates acute infection.
- A negative rubella antibody test indicates susceptibility to rubella infection.
- Low levels of IgM may occur in infectious mononucleosis.
Various antibodies in Rubella virus infection:
| Type of antibody test | Antibodies Appear | A peak level of antibodies | When antibodies disappear |
|
|
|
|
|
|
|
|
|
|
|
|
How will you summarize the Rubella virus infection?
- Single IgG antibodies that test positive indicate immune status.
- Advise IgM antibody for acute infection.
- If negative, repeat after 2 weeks.
- Advise IgM antibodies on the fetus and mother to diagnose congenital rubella virus infection.
- For reinfection, advise IgG antibodies.
- If a person develops a rash and there is doubt about rubella infection, get one immediate blood sample for the test and another after two weeks of the rash.
- Or advise IgM antibodies test for rubella after one week of the rash.
What is the mechanism of the vaccination of the rubella virus infection?
- Vaccination produces an immune response by producing antibodies (IgM + IgG) in around 95% of the cases.
- Antibodies appear after 10 to 28 days of the vaccination.
- Few people may take up to 8 weeks to show adequate antibodies.
- In the case of non-responders, revaccination can produce an immune response.
- IgG antibodies decline over time and may not be detectable after ten years of time.
Questions and answers:
Question 1: What is the other name of rubella infection?
Question 2: Which antibody is diagnostic of acute rubella infection?