Thyroid:- Part 1 – Thyroid Function Tests (Thyroid Hormones) T4, T3, TSH
Thyroid Function Tests
What sample is needed for the Thyroid Function Test?
- The serum of a patient is needed.
- TSH sample is stable for 5 to 7 days at 4 °C.
- T4 and T3 samples are stable for 7 to 14 days at room temperature (37 °C) or 2 to 8 °C.
What are the precautions for the Thyroid Function Test?
- Sample with hemolysis or lipemia is rejected.
- Centrifuge the turbid sample before performing the test.
What are the Thyroid function tests?
- T3 uptake.
- Free T3.
- Total T3.
- Total T4.
- Free T4.
- Free thyroxine index.
- TSH.
- Thyroglobulin (Tg)
What are the indications for Thyroid Function Test?
- These tests are done to evaluate thyroid dysfunction.
- T3 is advised to diagnose hyperthyroidism.
- T3 and T4 are advised to monitor replacement and suppressive therapy.
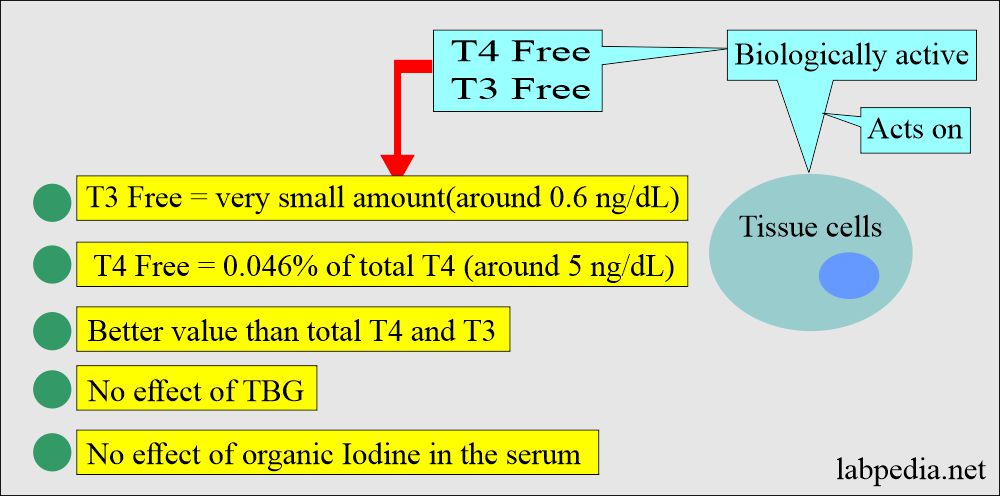
- Free T4 is advised to evaluate the thyroid function in a patient with protein abnormality, which will affect total T4.
- The thyroid function test differentiates between:
- Euthyroid (thyroid function is normal).
- Hyperthyroidism (Increased thyroid function).
- Hypothyroidism (decreased thyroid function).
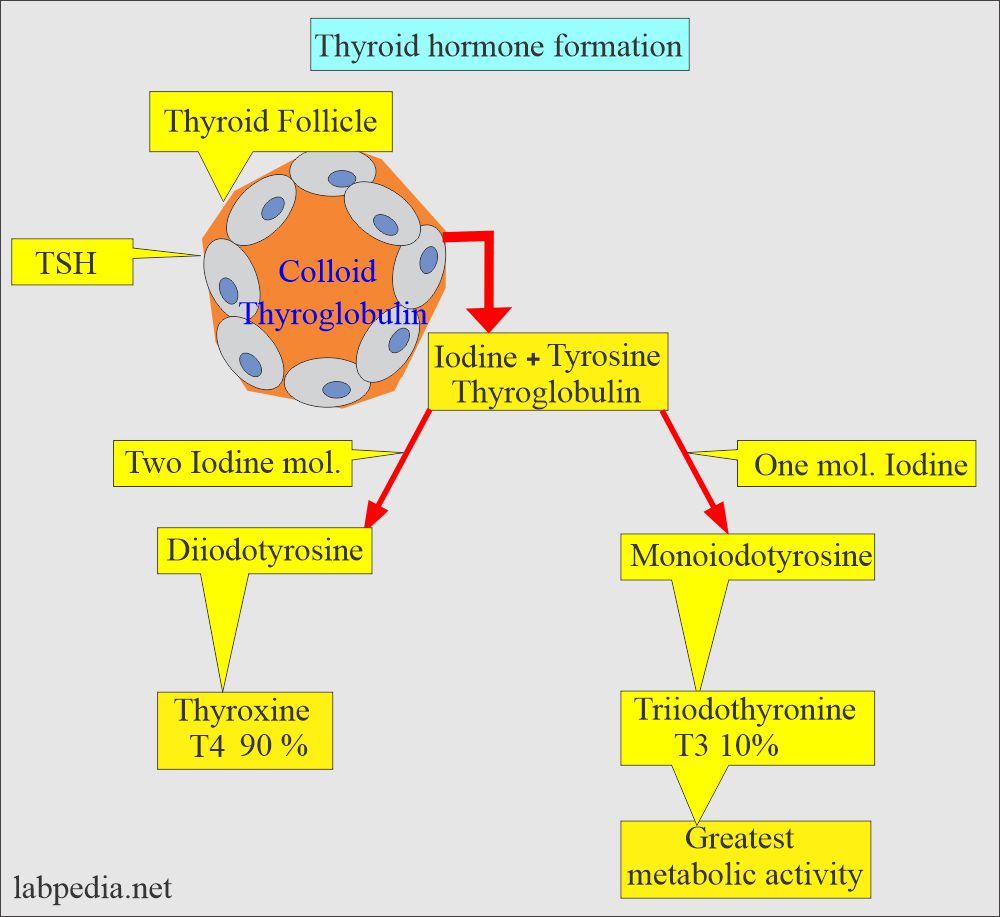
What is the pathophysiology of thyroid hormone?
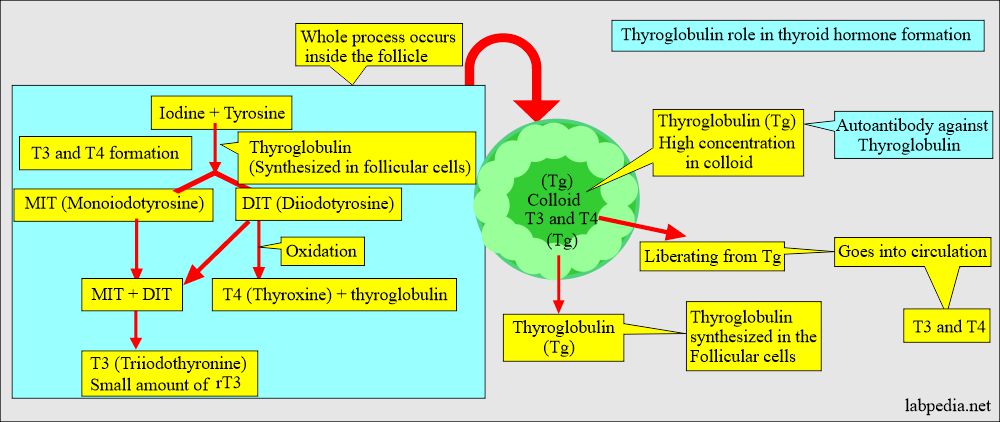
- Thyroid follicles are the basic secretory unit of the thyroid gland.
- The follicle has an outer epithelial cell layer surrounding the amorphous colloid material.
- Colloid mainly consists of thyroglobulin and a small amount of thyroalbumin.
- The thyroid gland has another cell, the parafollicular or C cell, present within the follicular basement or interfollicular spaces. These cells produce a hormone known as Calcitonin.
- The thyroid gland produces thyroxine (T4) and Triiodothyronine (T3).
- Diiodothyronine is the precursor of T3 and T4.
- T4 changes into T3 and reverse T3 (rT3) by deiodination.
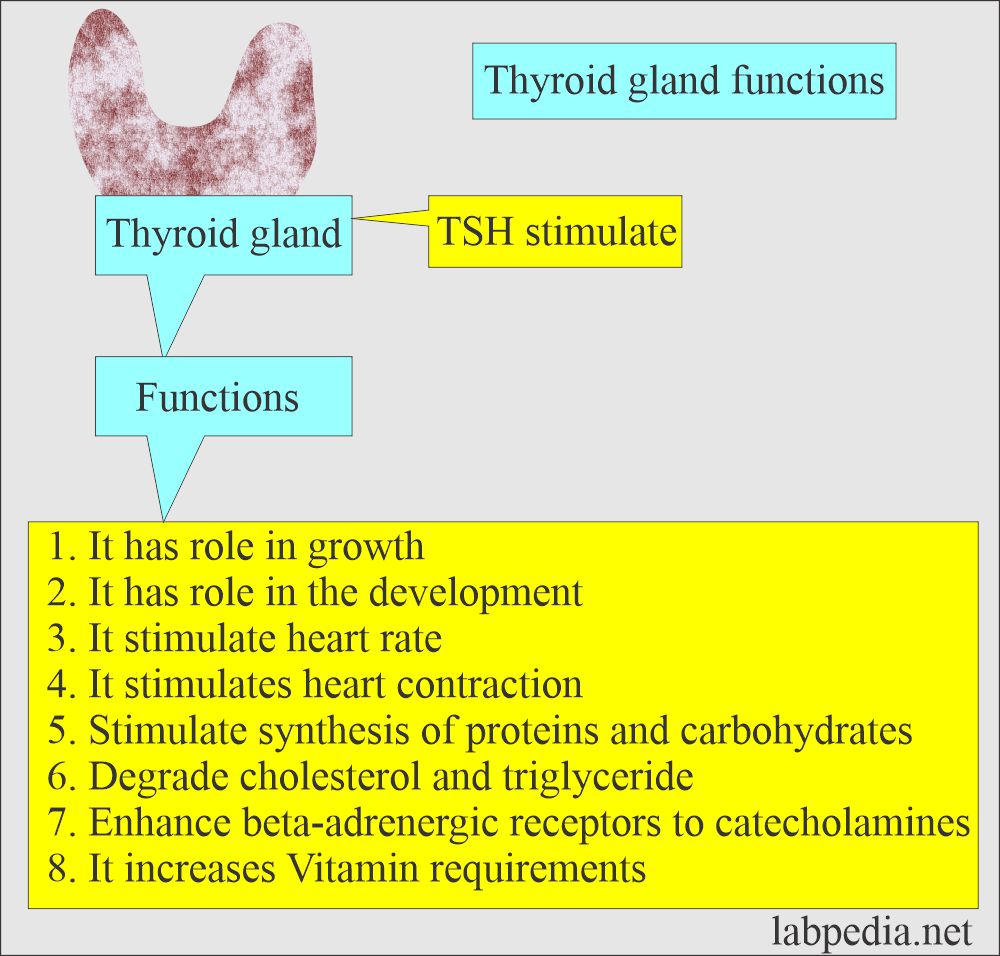
What are the functions of the thyroid?
- Control energy expenditure of the body.
- Stimulate heart contraction and heart rate.
- Stimulate carbohydrate and protein metabolism.
- Increase in the synthesis and degradation of cholesterol and triglycerides.
- It increases the sensitivity of the beta-adrenergic receptor to catecholamine.
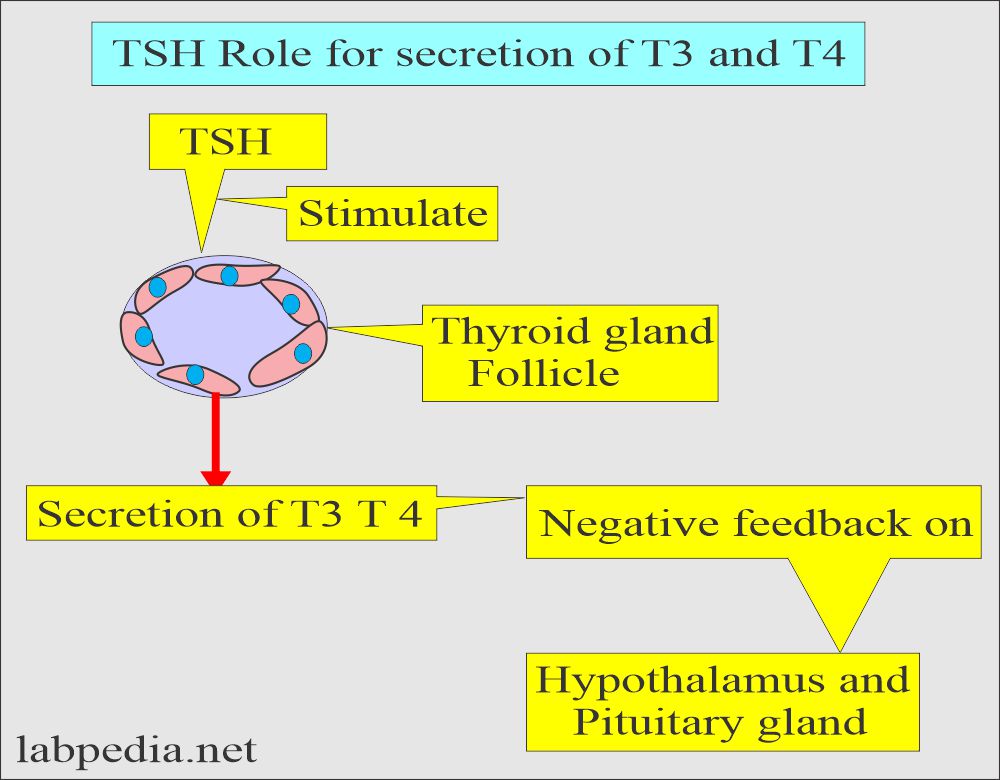
- Pituitary thyroid-stimulating hormone (TSH) regulates the synthesis of thyroid hormone.
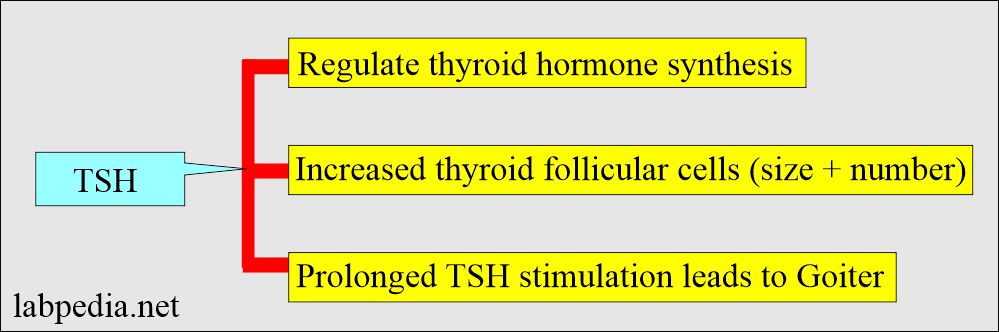
What are the functions of TSH?
- TSH Increases in the size and number of thyroid follicles.
- Prolonged TSH stimulation leads to increased vascularity and may form a goiter.
- The thyroid hormone maintains the rate at which your body uses fats and carbohydrates.
- Control your body temperature.
- Regulate the production of protein.
- The thyroid gland also produces calcitonin, a hormone that helps regulate the amount of calcium in your blood.
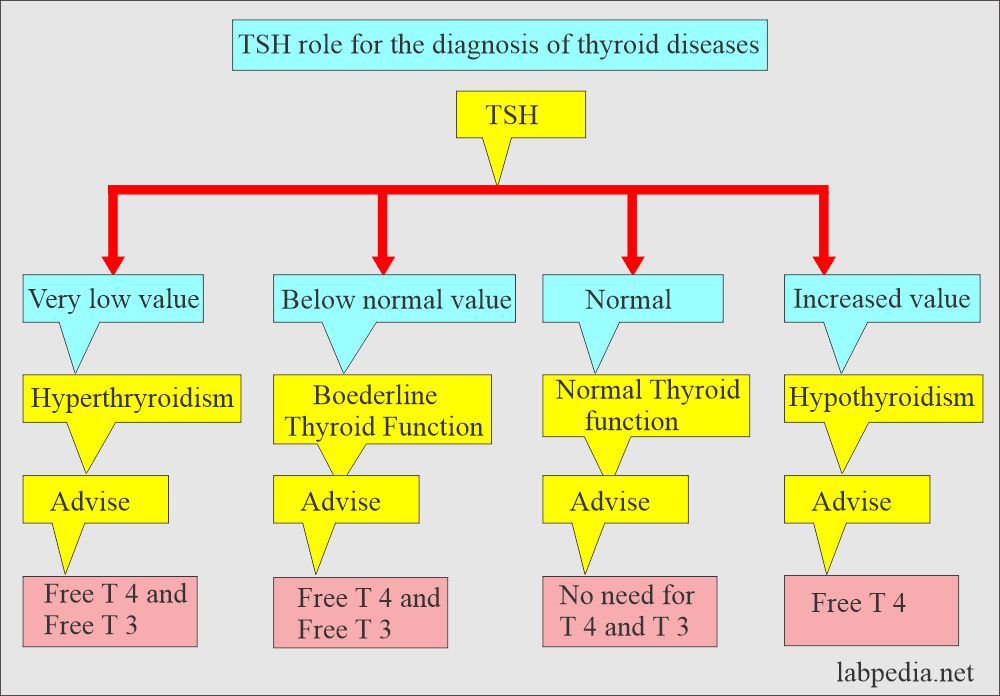
How will you discuss the cycle of thyroid hormone formation?
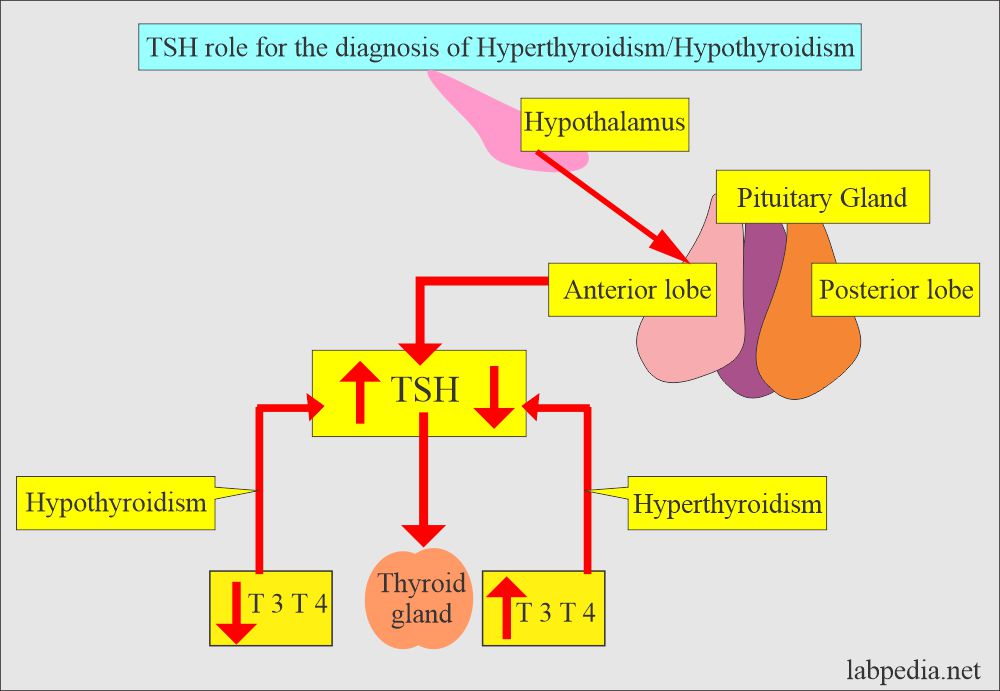
- The rate at which T3 and T4 are released is controlled by the pituitary gland and hypothalamus (which acts as a thermostat).
- The hypothalamus signals the pituitary gland to make Thyroid-stimulating hormone (TSH).
- The pituitary gland is a source of TSH.
- TSH amounts depend on the amount of T3 and T4 in the blood.
- There is a feedback mechanism. If the levels of T3 and T4 are decreased, the TSH level will increase.
- If T3 and T4 increase, the TSH level will fall below normal.
- The thyroid gland regulates its production of T3 and T4 based on the amount of TSH it receives.
What is Thyroid hormone regulatory control?
- The hypothalamus produces TRH + Somatotropin, which stimulates the Pituitary gland to produce TSH.
- TSH acts on the thyroid gland to stimulate secretion of T4+ iodine trapping + new hormone synthesis + stimulate thyroid cell hypertrophy (Goiter).
- T4 + T3 = Negative feedback mechanism on pituitary gland + hypothalamus.
- Hypothyroidism occurs when the thyroid does not produce enough T3 and T4.
- Hyperthyroidism occurs when thyroid glands produce an excess of T3 and T4.
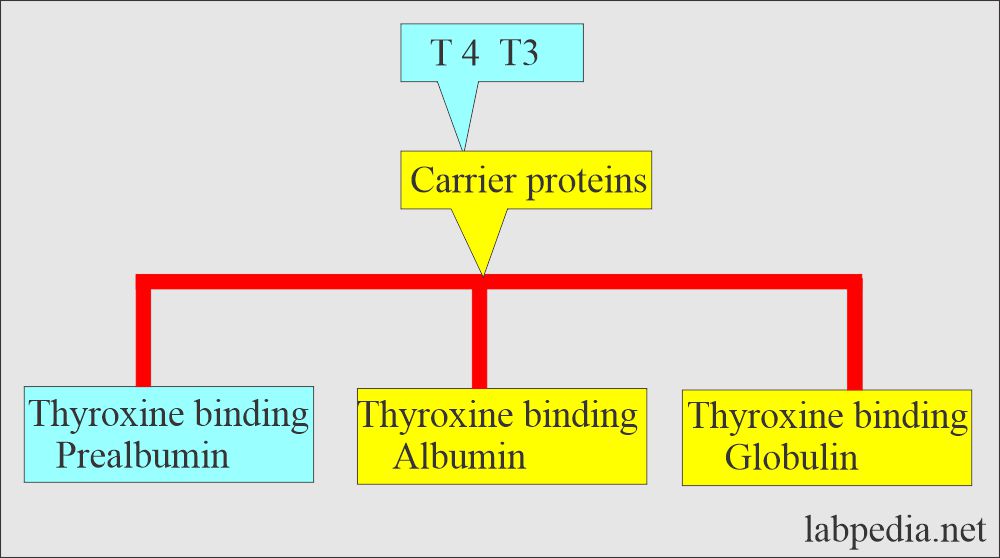
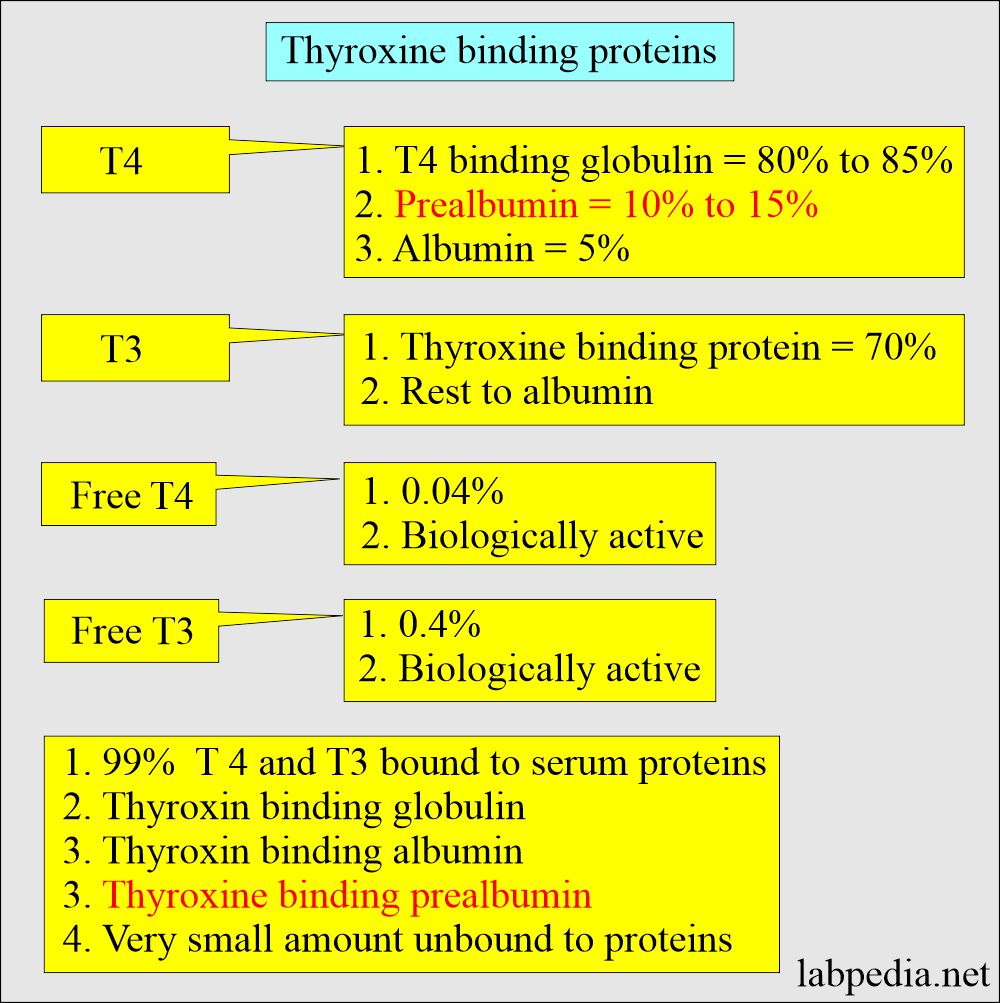
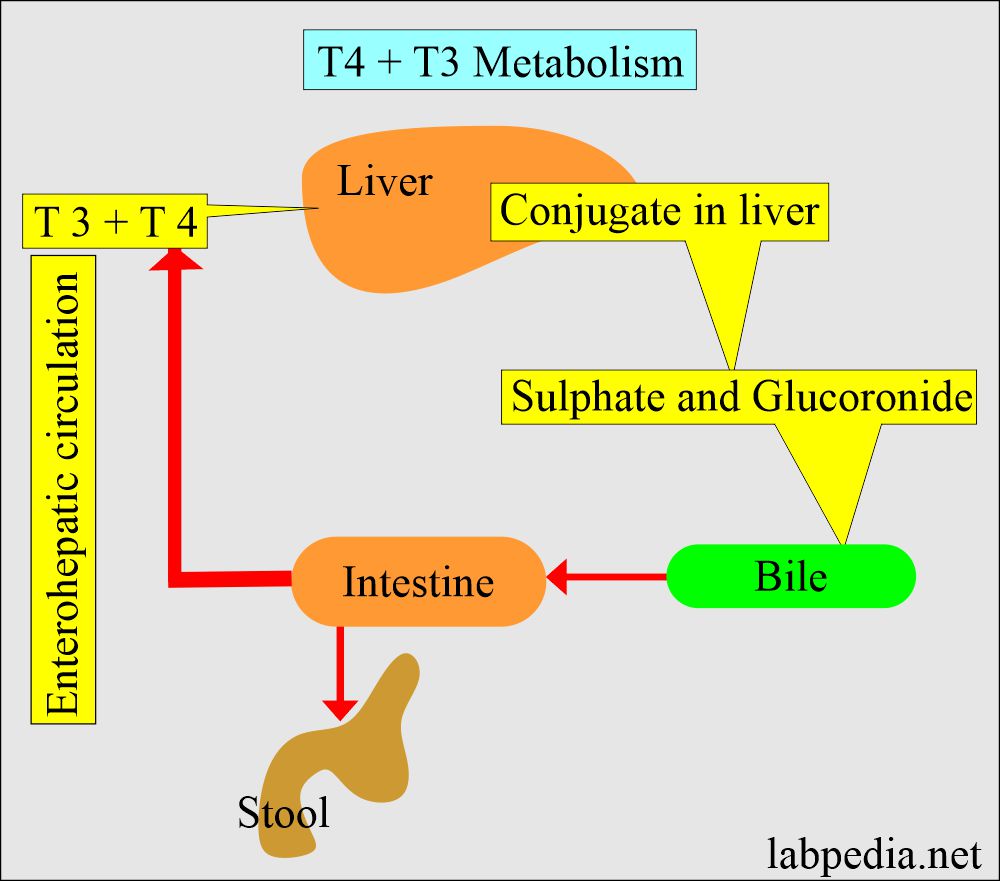
What is the metabolism of T3 and T4?
- T3 and T4 conjugate in the liver to form Sulphate and glucuronide.
- These conjugates enter the bile and the intestine.
- Thyroid hormone conjugates are hydrolyzed and reabsorbed from the intestine (Enterohepatic circulation), and some are excreted in the stool.
- The T3 rise may be the first and only abnormality in the case of Hyperthyroidism.
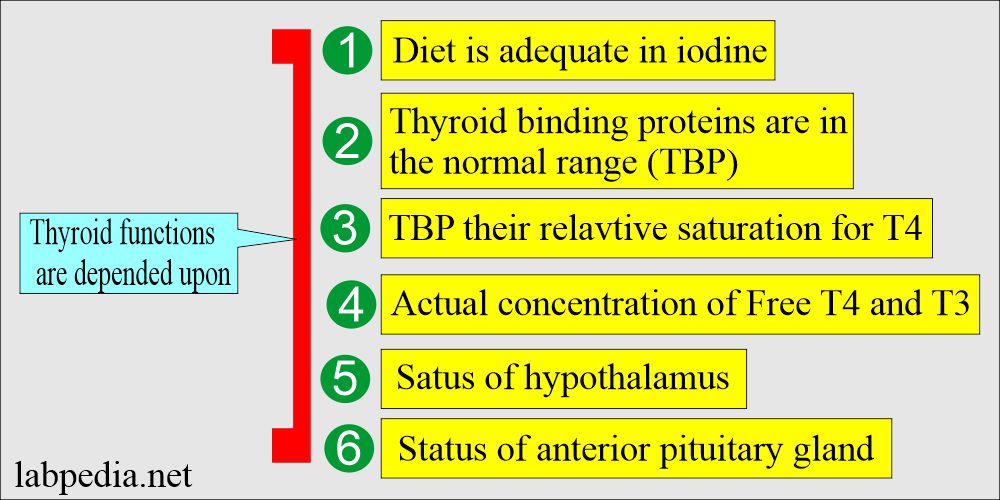
- The thyroid function tests depend upon various factors.
What are the normal Values of thyroid hormones?
Source 1
T3 Total
- Cord blood (>37 weeks) = 5 to 141 ng/dL
- 1 to 3 days = 100 to 740 ng/dL
- 1 to 11 months = 105 to 245
- Children
- 1 -5 years = 105 to 269 ng/dL
- 6 to 10 years = 94 to 241 ng/dL
- 16 to 20 years = 80 to 210 ng/dL
- Adult
- 20 to 50 years = 70 to 204 ng/dL
- 50 to 90 years = 40 to 181 ng/dL
- Pregnancy
- Last 5 months = 116 to 247 ng/dL
- To convert into SI unit x 0.0154 = nmol/L
- Last 5 months = 116 to 247 ng/dL
Source 1
Free T3
- Cord blood (>37 weeks ) = 15 to 391 pg/dL
- Child and adult = 260 to 480 pg/dL (4.0 to 7.4 pmol/L)
- Pregnancy
- First trimester = 211 to 383 pg/dL
- Second and third trimesters = 196 to 338 pg/dL
Another source 2
T3 total
- 1 to 3 days = 100 to 740 ng/dL
- 1 to 11 months = 105 to 245 ng/dL
- 1 to 5 years = 105 to 270 ng/dL
- 6 to 10 years = 95 to 240 ng/dL
- 11 to 15 years = 80 to 215 ng/dL
- 16 to 20 years = 80 to 210 ng/dL
- 20 to 50 years = 75 to 220 ng/dL
- >50 years = 40 to 180 ng/dL
Another source 1
T4 Total (T4)
| Age | µg/dL |
| Cord blood | 7.4 to 13.0 |
| 1 to 3 days | 11.8 to 22.6 |
| 1 to 2 weeks | 9.8 to 16.6 |
| 1 to 4 month | 7.2 to 14.4 |
| 4 to 12 month | 7.8 to 16.5 |
| 1 to 5 year | 7.3 to 15.0 |
| 5 to 10 year | 6.4 to 13.3 |
| 10 to 15 year | 5.6 to 11.7 |
| Adult | Male = 4.6 to 10.5 Female = 5.5 to 11.0 |
| >60 year | 5.0 to 10.7 |
| Maternal serum 15 to 40 weeks | 9.1 to 14.0 |
Another source 1
T4 Free (FT4)
| Age | ng/dL |
|
|
|
|
|
|
|
|
|
|
|
|
- To converts SI unit x 12.9 = nmol/L
Source 2
T4 Total (T4)
| Age | µg/dL |
| 1 to 3 days | 11.22 |
| 1 to 2 weeks | 10 to 16 |
| 1 o 12 months | 8 to 16 |
| 1 to 5 years | 7 to 15 |
| 5to 10 years | 6 to 13 |
| 10 to 15 years | 5 to 12 |
| Adult | Male 4 to 12 Female 5 to 12 |
| >60 years | 5 to 11 |
Another source 2
T4 Free
- Newborn (0 to 4 days) = 2 to 6 ng/dL (26 to 77 pmol/L)
- Child 2 weeks to 20 years = 0.8 to 2.0 ng//dL
- Adult = 0.8 to 2.8 ng/dL (10 to 36 pmol/L)
TSH
Source 1
| Age | µU/mL |
|
Premature infants 28 to 36 weeks gestation |
0.7 to 27 |
| 1 to 4 days | 1.0 to 39 |
| 2 to 20 weeks | 1.7 to 9.1 |
| 5 months to 20 years | 0.7 to 6.4 |
| Adults | |
| 21 to 54 years | 0.4 to 4.2 |
| 55 to 87 years | 0.5 to 8.9 |
| Pregnancy | |
| First trimester | 0.3 to 4.5 |
| Second trimester | 0.5 to 4.6 |
| Third trimester | 0.8 to 5.2 |
- To converts into SI unit x 1.0 = mU/L
Source 2
- Adult = 0.4 to 5.6 mIU/L
- Newborn = 3 to 20 mIU/L
- Cord blood = 3 to 12 µU/mL
- Values vary between laboratories.
Another source
- Adult
- 21 to 54 years = 0.4 to 4.2 mU/L
- 55 to 87 years = 0.5 to 8.9 mU/L
- Newborn = 1.7 to 9.1 mU/L
- 0.3 to 3.04 mIU/L (another reference)
- Pregnancy
- First trimester = 0.3 to 4.5 mU/L
- Second trimester = 0.5 to 4.6 mU/L
- Third trimester = 0.8 to 5.2 mU/L
(Normal values vary from lab to lab and different methodologies)
| Thyroid disease | T4 total | T4 free | T3 total | T3 free | TSH |
| Normal | N | N | N | N | N |
| Hypothyroidism | Low | Low | Low low | Low | High |
| Hyperthyroidism | High | High | High | High | low or absent |
How will you discuss Hypothyroidism?
- There is inadequate production of thyroid hormones:
- It is characterized by decreased T4.
- Ther is an increased level of TSH.
- Signs and Symptoms of Hypothyroidism:
- The signs and symptoms of hypothyroidism vary widely, depending on the severity of the hormone deficiency.
- At first, you may barely notice symptoms such as fatigue and sluggishness.
- Increased sensitivity to cold
- Constipation.
- Skin is pale and dry skin.
- There is puffiness of the face due to edema.
- The patient develops Hoarseness of voice.
- There is an increased level of cholesterol.
- The patient also gains weight.
- There are Muscle aches, tenderness, and stiffness.
- There is Muscle weakness
- There may be pain, stiffness, or swelling of joints.
- Female patients develop heavier menstrual periods.
- The patient may develop signs of Depression.
- Usually, these patients become obese.
- There may be joint pain.
- This patient may suffer from infertility.
- These patients may develop heart problems.
- In untreated cases, signs and symptoms become worse.
- Constant stimulation of the thyroid gives rise to enlargement of the gland, which is called Goiter.
- Advanced hypothyroidism is known as Myxedema.
How will you discuss Myxedema?
- It includes more signs and symptoms like :
- Low blood pressure.
- Decreased breathing.
- Decreased body temperature.
- Unresponsiveness can even cause the patient to go into a coma.
- Myxedema may be fatal in some patients.
What are the Causes of hypothyroidism?
- Autoimmune thyroid disease.
- Iodine deficiency.
- Iodine-induced.
- Goitrogen exposure.
- A defect in hormone synthesis.
- Thyroid ablation by surgery or radiation.
- Thyroid agenesis or dysgenesis.
- Hypothalamic-pituitary disease.
How will you diagnose Hypothyroidism?
| Clinical condition | TSH | Total thyroxine | Free T4 | T3 | Thyroglobulin |
| Primary hypothyroidism | Increased | Decreased | Decreased | Decreased | Normal/Increased |
| Secondary hypothyroidism | Normal/decreased | Decreased | Decreased | Decreased | |
| Tertiary hypothyroidism | Normal/decreased | Decreased | Decreased | Decreased |
How will you diagnose Hashimoto’s disease?
| Causes | TSH | T3 | T4 |
| Pituitary abnormality | High | Low | Low |
| Hashimoto’s disease in an early stage | High | Low | Low |
| Hashimoto’s disease in late-stage | High | Low or normal | Low or normal |
Hyperthyroidism (Thyrotoxicosis)
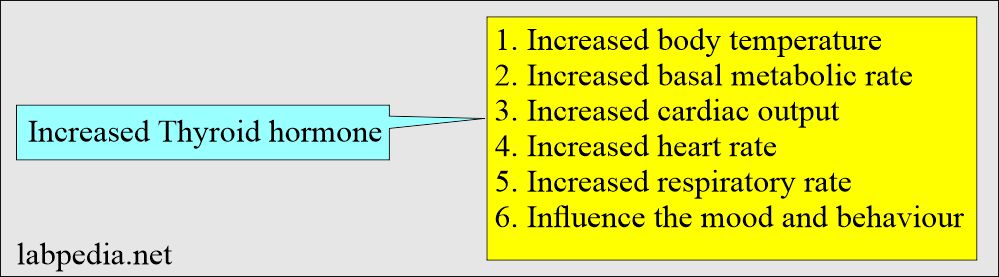
There is excessive production of thyroid hormones:
- It is characterized by elevated T4.
- There is a decreased or even absent level of TSH.
What are the Signs and Symptoms of Hyperthyroidism?
- Hyperthyroidism can significantly accelerate your body’s metabolism, causing :
- Sudden weight loss, even appetite, and food intake remain normal or increase.
- Rapid or irregular heartbeat ( Tachycardia, Palpitation may be more than 100 beats/minutes.).
- The patient may even develop Arrhythmias.
- The patient develops sweating.
- Nervousness or irritability.
How will you discuss Graves disease?
- This is an autoimmune disorder.
- Grave’s Disease is due to Hyperthyroidism.
- Symptoms of hyperthyroidism:
- Tremors are usually fine, trembling with hands and fingers.
- Patients have increased sensitivity to heat.
- Changes in bowel patterns, especially more frequent bowel movements.
- An enlarged thyroid gland (goiter).
- The patient will have Fatigue and muscle weakness.
- The patient will have sleep difficulty.
- Beta-blockers can mask many of the symptoms of hyperthyroidism.
What are the Causes of hyperthyroidism?
- Multinodular goiter.
- Single toxic goiter.
- Subacute thyroiditis.
- Autoimmune thyroid disease.
- Pituitary adenoma (thyrotropin-producing tumor).
- Gestational trophoblastic tumor.
- Postpartum Thyroid disease.
- Hyperemesis gravidarum.
- Exogenous thyroid hormones.
- Metastatic thyroid cancer.
- Iodine-induced.
What are the findings in Hyperthyroidism:?
| Causes | TSH | T3 | T4 |
| Grave’s Disease | Low | Raised | Raised |
| Thyroiditis with hyperthyroidism | Low | Raised | Raised |
| Thyroid nodule (hot or toxic ) | Low | Raised | Raised |
What are the lab tests in various thyroid diseases?
| Disease | TSH | T4 |
|---|---|---|
| Multinodular goiter | low | high |
| Single toxic nodule | low | normal or high |
| Subacute thyroiditis | low | high |
| Autoimmune thyroid disease | low | high |
| TRH pituitary adenoma | normal or high | high |
| Gestational neoplasm | low | high |
| Postpartum hyperthyroidism | low | high |
| Hyperemesis gravidarum | low or normal | high |
| Metastatic thyroid cancer | low | high |
| Iodine-induced | variable | high |
| Exogenous thyroxine | low | high |
How will you discuss Goiter?
- Definition: This is an enlarged thyroid gland because of any cause.
- Causes are :
- Inflammatory.
- A function that may be normally increased or decreased.
- Neoplastic.
- Most goiters have normal function, with 90% of the multinodular goiters being colloid goiters.
What is Euthyroid Sick syndrome?
- This is also known as low T3 syndrome.
- There is biochemical hypothyroidism as T4 is shifted away to form T3.
- Total T4 and TSH usually remain within normal limits.
How will you summarize Thyroid function tests?
| Disease | T3 | T4 (total) | T4 free | TSH | Cholesterol |
| Hypothyroidism | decreased | decreased | low | increased | increased |
| Hyperthyroidism | increased | increased | increased | decreased or absent | decreased |
| Excess Thyroid-binding globulin (TBG) | increased | increased | Normal | decreased | |
| Decreased thyroglobulin (TBG) | Low | Low | Normal |
How will you differentiate different thyroid diseases?
| Clinical disease | Free T4 | Total T4 | T3 | TSH | Thyroglobulin |
| Hyperthyroidism primary clinical | Increased | Increased | Increased | Decreased | Normal |
| Hyperthyroidism subclinical | Normal | Normal | Normal | Decreased | Normal |
| Hypothyroidism primary clinical | Decreased | Decreased | Decreased | Increased | Normal/Increased |
| Hypothyroidism primary subclinical | Normal | Normal | Normal | Increased | Normal |
| Hypothyroidism Secondary | Decreased | Decreased | Decreased | Normal/Decreased | |
| T3 thyrotoxicosis | Normal | Normal | Increased | Decreased | Normal |
| TSH-secreting tumors | Increased | Increased | Increased | Increased | Normal |
| Pregnancy with hyperthyroidism | Increased | Increased | Increased | Normal | Increased |
| Pregnancy with hypothyroidism | Decreased | Increased | Increased | Increased | Increased |
| Goiter | Normal | Normal | Normal | Normal | Normal |
| Thyroid carcinoma | Normal | Normal | Normal | Normal | Increased |
| Hashimoto’s thyroiditis | Variable | Variable | Variable | Variable | |
| Nephrosis | Decreased | Decreased | Normal | Decreased |
- Please see more details in T3 and T4.