Syphilis:- Part 1- Syphilis Presentation (Treponema Pallidum)
Syphilis (Treponema Pallidum)
What sample is needed for the diagnosis of Syphilis (Treponema Pallidum)?
- The serum of the patient is needed.
What is the indication for Syphilis (Treponema Pallidum)?
- For the diagnosis of syphilis.
How will you define syphilis (Treponema pallidum)?
- The disease syphilis was reported in the medical literature as early as 1495.
- In treating syphilis, Heavy metals, such as arsenic, were replaced by penicillin in 1940.
- Treponema pallidum is a member of the order Spirochaetales and the family Treponemataceae.
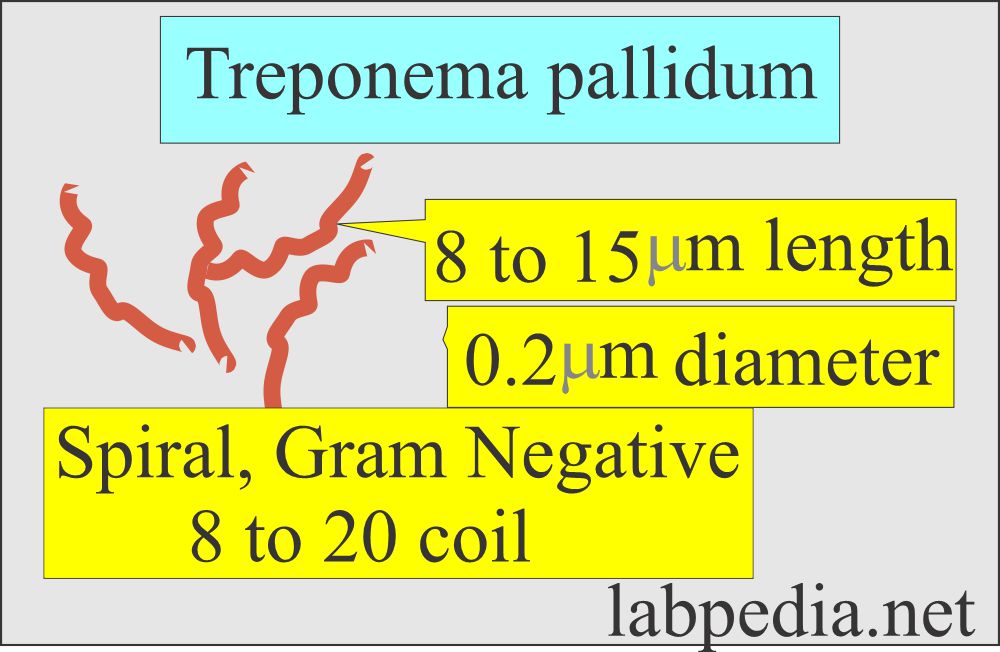
How will you describe Syphilis (Treponema pallidum) microbiology?
Spirochetes:
- It is a gram-negative organism and looks like a corkscrew.
- These are fine, spiral organisms with 8 to 24 coils. They are approximately 6 to 15 µm long and 0.2 µm in diameter.
- These bacteria can move in a spinning fashion called axial filaments.
- These bacteria replicate by transverse fission.
- This organism can not grow in ordinary media.
- These have a gram-negative cell membrane.
- These are too small to see under the light microscope.
- So, a special procedure, such as dark field, immunofluorescence, and silver stain, is used to see these organisms.
- Also, serological tests can help to diagnose syphilis.
- Syphilis is a chronic venereal disease.
- This was discovered in epidemic form in Europe in the 16th century.
- The first diagnostic blood test for syphilis was introduced by Wassermann in 1906.
- Afro-Americans are infected 30 times more than white Americans.
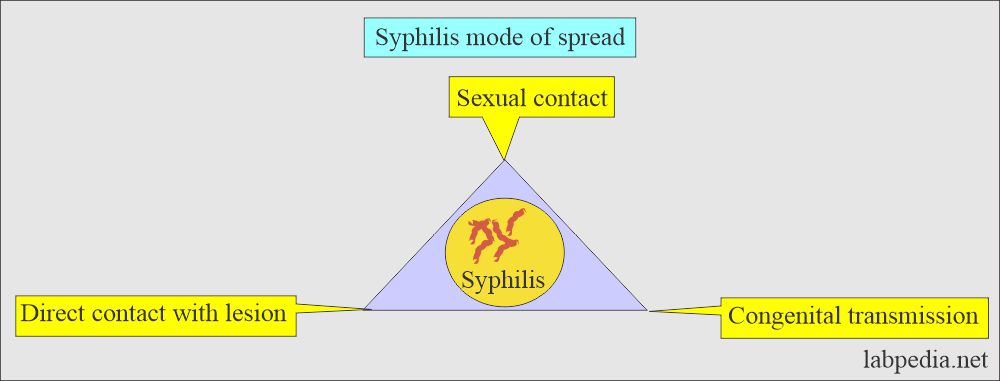
What is the mode of spread of syphilis (Treponema pallidum)?
- Spirochaete Treponema Pallidum causes syphilis, and its natural host is humans.
- The most common source of infection is a cutaneous or mucosal lesion in the primary or secondary stage of the disease.
- During sexual acts, the organism enters the body through minute abrasion of the skin or mucous membranes.
- Once it enters the body, the spirochetes are immediately disseminated.
- In congenital syphilis, it spreads across the placenta to the fetus.
- The incubation period is 2 to 4 weeks.
- Syphilis can spread through:
- sexual contact
- Congenital
- Direct contact with the lesion.
What are the Treponema-associated diseases in humans?
- T. Pallidum = Syphilis
- T. pallidum variant = Bejel
- T. carateum = Pinta
- T. pertenue = Yaws
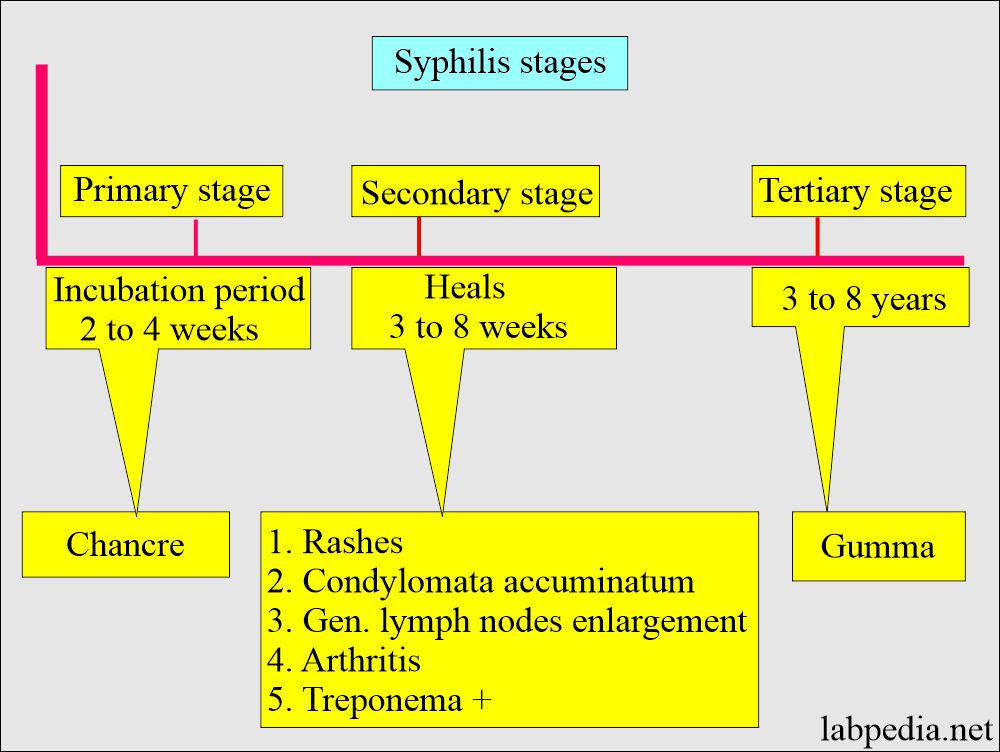
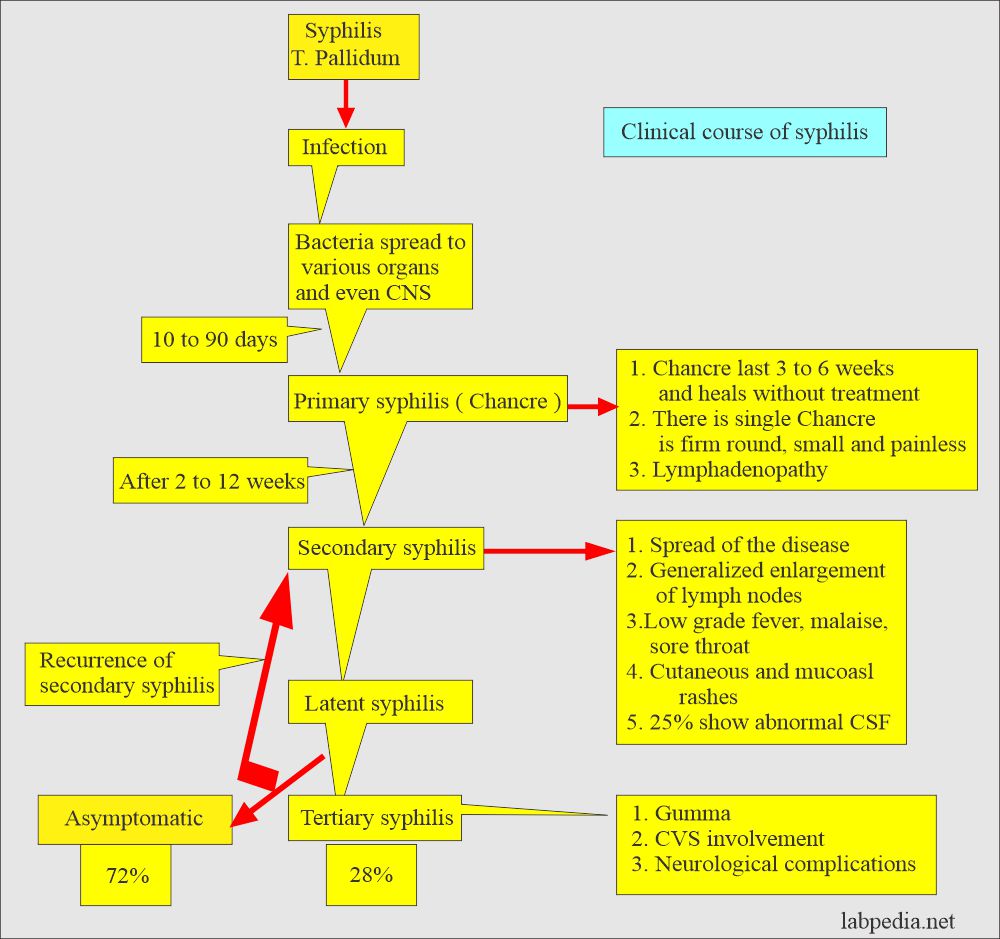
What are the clinical stages of Syphilis (Treponema pallidum)?
- Clinically, syphilis is divided into four stages:
- Primary stage.
- Secondary stage.
- Latent stage.
- Tertiary or late stage.
- What is the incubation period?
- This is 2 to 4 weeks (3 to 6 weeks average), and the range may be 1.5 to 13 weeks.
- . The primary stage starts after this incubation period.
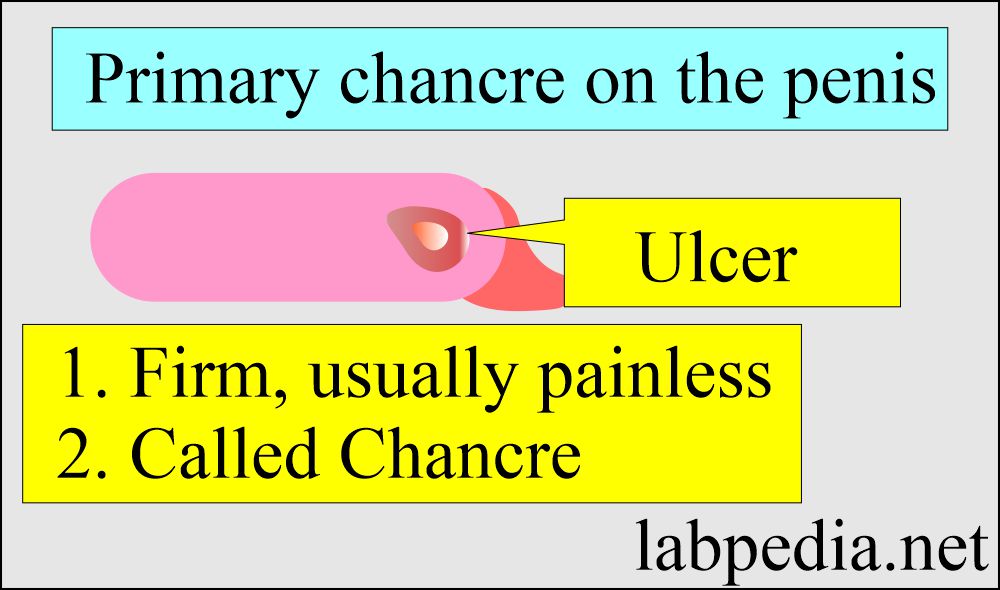
The primary stage:
- This is characterized by the appearance of a chancre at the primary site of inoculation.
- In the male, the lesion is at the penis, and in the female are multiple lesions on the vagina or the cervix.
- It has a firm and usually painless ulcer called Chancre.
- These ulcers are shallow and are at the site of infection.
- Enlarged lymph nodes may be seen and are painless.
- This heals spontaneously in 3 to 8 weeks. This stage lasts 4 to 6 weeks (2 to 8 weeks).
- The lesion is positive for the spirochetes.
- Serological tests for syphilis are often negative in the early phase of the disease, so advise darkfield microscopy or a direct fluorescent antibody test.
- In the primary stage, Chancre usually heels, followed by the secondary stage.
The secondary stage:
- 25% of untreated cases from the primary chancre go into the secondary stage.
- The secondary stage lasts for about 4 to 12 weeks.
- The Patient may develop this stage after roughly 2 months of the chancre (or 6 to 8 weeks).
- The infection becomes generalized 6 to 8 weeks later; this is the bacteremia stage.
- This is characterized by the appearance of systemic lesions.
- Mucous membrane lesions may be seen in the oral cavity (in 60% of the cases).
- There are widespread rashes of the skin.
- These rashes (about 80%) are small, red, flat lesions distributed over the body.
- These rashes typically involve palms and soles.
- Cutaneous surfaces, warts-like lesions called Condylomata, are seen. They are usually seen in moist and warm sites like the perianal area, vulva, and scrotum.
- Any organ, including CNS, eyes, kidneys, and bones, may be involved.
- This is a highly infectious stage and contains many organisms (treponemes).
- Generalized lymphadenopathy is seen in 50% (75%) of cases.
- Asymptomatic involvement of the central nervous system is seen in roughly 30% of the cases.
- Other rare complications are arthritis, hepatitis, glomerulonephritis, periostitis, and sometimes iridocyclitis and chorioretinitis.
- These mucocutaneous lesions are highly infectious.
- During the last part of the secondary stage, visible lesions disappear, and the patient enters the latent stage.
Latent syphilis:
- The latent stage may last about 3 to 5 years.
- The disease has been dormant for many years. The symptoms of the second stage have resolved.
- But serological tests are positive.
- 25% or more will have a relapse and develop an infectious lesion of the skin, like secondary syphilis.
- After 4 years, there are generally no more relapses, and this disease may be noninfectious except for pregnant mothers.
- This ultimately develops into cardiovascular or neurosyphilis.
- Roughly 1/3 of cases progress into the tertiary stage.
Late syphilis:
- This occurs after 10 to 20 years of the primary lesion.
- There are two main types:
- Cardiovascular involvement in the form of aortitis and aneurysm.
- Neurosyphilis may be:
- General paralysis with dementia, tremors, and spastic paralysis.
- Tabes dorsalis with ataxic gate, trophic changes in joints in the form of Charcot’s joints.
- There may be optic atrophy.
- Meningovascular syphilis causes a headache, cranial nerve palsies, and Argyll- Robertson pupil (pupillary loss of reaction to light).
Tertiary stage:
- This stage appears 3 to 10 years after the primary lesion (another source says it takes 6 to 40 years to develop the tertiary stage).
- This is also called late syphilis and is a noninfectious stage.
- This is characterized by granulomatous skin lesions called gummas, which may occur on a mucous membrane, subcutaneous tissue, bone, and viscera.
- 25% of the patients may develop neurologic, ocular, and cardiovascular diseases.
Late or quaternary stage:
- 10 to 20 years after primary syphilis, there are two main clinical sequences:
- Neurosyphilis may present as follows:
- General paralysis of insane with dementia, tremor, and spastic paralysis.
- Tabes dorsalis with characteristic features of ataxic gait, atrophic changes in joints, Charcot’s joints, and there may be optic atrophy.
- Meningovascular syphilis with a headache, cranial nerve palsies, and papillary loss of reaction to light (Argyll-Robertson pupil).
What is the presentation of syphilis (Treponema pallidum)?
- Gumma formation:
- In about 15% of untreated cases, the gummatous lesion appears after 3 to 10 years of the primary lesion.
- These are granulomatous lesions.
- These are noninfectious lesions mainly found in the skin and the bone.
- Cardiovascular involvement:
- These are seen after at least 10 years of the primary infection in 10% of the untreated cases.
- An aneurysm exists in the aorta (ascending part) or aortic arch.
- Neurosyphilis:
- This disease is seen in roughly 8% of untreated cases.
- Neurosyphilis presentation is as follows:
- Asymptomatic patients when patients look normal. But the CSF is serologically positive.
- Subacute meningitis is when the patient has a fever, stiff neck, and headache.
- CSF examination shows:
- Increased proteins.
- Low glucose level.
- Increased number of lymphocytes.
- Positive tests for syphilis.
- Meningovascular syphilis is when the brain’s blood vessels and meninges are damaged.
- There are cerebrovascular occlusion and infarction of the tissue in the brain, meninges, and spinal cord.
- Tabes dorsalis affects the spinal cord.
- In this case, the posterior column and dorsal roots are involved.
| Clinical stage | Clinical presentation |
|
|
|
1. Skin involvement with the presence of rashes 2. Involvement of CNS, bones, eyes, kidneys, arthritis 3. Condylomata latum |
|
|
|
1. Neurosyphilis 2. Involvement of the cardiovascular system 3. Gumma of the skin and bone |
How will you discuss Congenital syphilis?
- Bacteria can enter fetal circulation at any time from the placenta during pregnancy, crossing the placental barrier.
- The chances are higher when the mother is in the primary or secondary stage to infect the fetus.
- Without treatment, roughly 40% of the fetus will die in-utero around the 4th month of the pregnancy.
- The manifestations of congenital syphilis are:
- Stillbirth.
- Infantile syphilis.
- Hepatosplenomegaly and bone abnormalities.
- There are pancreatic fibrosis and pneumonitis.
- The lungs may be firm and pale.
- Tissues are positive for the spirochetes.
- Congenital syphilis was clinically seen as:
- Latent infection when there are no symptoms, but infants are serologically positive.
- The early stage appears after the end of the second year.
- Most infants are healthy at birth, and symptoms appear in the first few weeks.
- There are generalized skin rashes and nasal deformities. Hepatitis, meningitis, anemia, and bone lesions.
- Late syphilis manifestations appear in the first few weeks of life.
- They may not be able to thrive.
- There is bone sclerosis.
- Joint effusion and arthritis.
- Interstitial keratitis.
- Juvenile general paralysis of the insane and tabes.
- Deafness.
- Notching of the incisor teeth.
How will you diagnose syphilis (Treponema pallidum)?
- Specific tests for syphilis are:
- Treponema pallidum immobilization test (TPI).
- Fluorescent treponemal antibody absorption test (FTA-ABS).
- The micro-hemagglutination assay for treponema pallidum (MHA-TP).
- Reiter protein complement fixation test (RPCF).
- Reiter protein is produced by the non-pathogenic treponema called the Reiter strain.
- Darkfield examination.
- This is a direct examination of Treponema pallidum from the syphilitic lesion.
- Immunological tests.
- Cardiolipin test. This is the first serologic test. This was dependent upon the complement activation.
- Cardiolipin is from the beef heart and is a phospholipid.
- VDRL (Venereal disease research laboratory test) is based on cardiolipin.
- CSF (cerebrospinal fluid) examination.
Questions and answers:
Question 1: What are the chances of getting an infection of the fetus?
Question 2: What are the complications of the tertiary stage of syphilis?