Stool Examination:- Part 1 – Stool Examination and Interpretations
Stool Examination
What stool sample is needed for examination?
- The fresh stool can be examined immediately for moving organisms.
- Stool in 10% formalin can be used for Helminths and protozoa.
- A stool in formalin-ethyl acetate is used to concentrate the stool.
- The smallest amount of stool needed for the examination is 2 to 5 grams.
- For ova and parasites, there are three methods:
- Direct stool examination.
- Concentration method.
- The permanent stain of the stool.
What samples are used for various parasitic infestations?
| Sample for testing | Possible diagnosis |
|
|
|
|
|
|
|
|
|
|
|
|
What are the Precautions needed for stool examinations?
- Advise patients about the following things for at least 48 hours before the collection of the stool:
- Avoid mineral oils.
- Do not take bismuth.
- Don’t take antibiotics like tetracyclines.
- Anti-diarrheal drugs are non-absorbent.
- Avoid anti-malarial drugs.
- The patient should not have a barium swallow examination before the stool examination.
- Stop iron-containing drugs, meat, and fish 48 hours before the collection of occult blood.
- Warm stools are better for the ova and parasites.
- Don’t refrigerate the stool for ova and parasites.
- Stools for ova and parasites can be collected in formalin and polyvinyl alcohol, which are used as fixatives.
- If blood or mucus is present in the stool, it should be included because most pathogens are found in this substance.
- Examine the stool before giving antibiotics or other drugs.
- The semi-formed stool should be examined within 60 minutes of collection.
- The liquid stool should be examined within the first 30 minutes.
- The solid stool should be examined within the first hour of collection.
- Trophozoites degenerate in liquid stool rapidly, so examine the stool within 30 minutes.
- In constipated cases, use non-residual purgatives the night before collecting the stool.
What are the indications for stool examination?
- To evaluate the function and integrity of the GI tract.
- To rule out the presence of WBCs and RBCs.
- To find ova or parasites.
- To see the presence of fat for malabsorption syndrome.
- For screening for colon cancer.
- For asymptomatic ulceration of the GI tract.
- Evaluate diseases in the presence of diarrhea and constipation.
- Summary of stool studies:
- Intestinal bleeding.
- Infestation.
- Inflammatory diseases.
- Malabsorption.
- Different causes of diarrhea.
What are the stool preservatives?
- Preservatives for the wet preparation are:
- 10% formol-saline for the wet preparation. This is the best preservative as it kills bacteria and preserves protozoa and helminths.
- Sodium acetate formalin.
- Methionate iodine formalin. This is a good preservative for the field collection of the stool.
- For staining, use Polyvinyl alcohol.
- Avoid preservatives for the culture of stool.
- Usually, three parts of the preservatives and one part of the stool.
What will you look for in the Gross Stool examination?
- Color.
- Consistency.
- Quantity.
- Odor.
- Mucous.
- Helminths.
- Concretions (gallbladder stones rarely may be found).
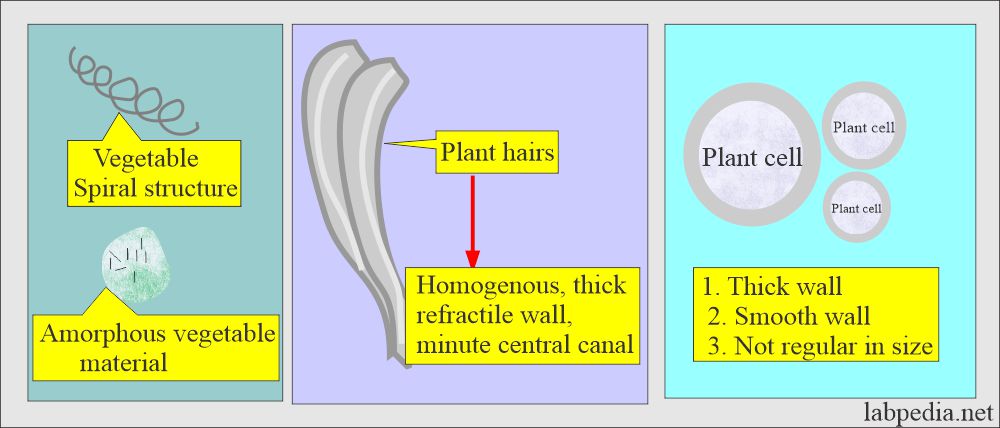
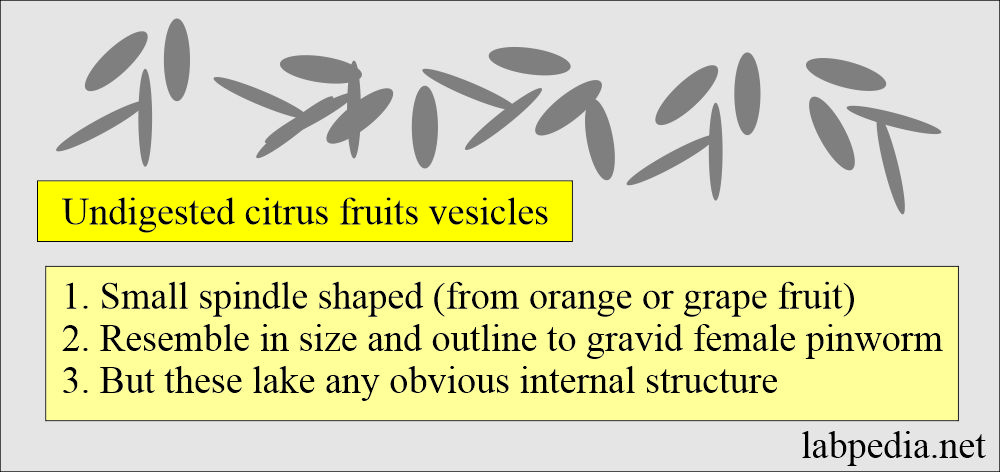
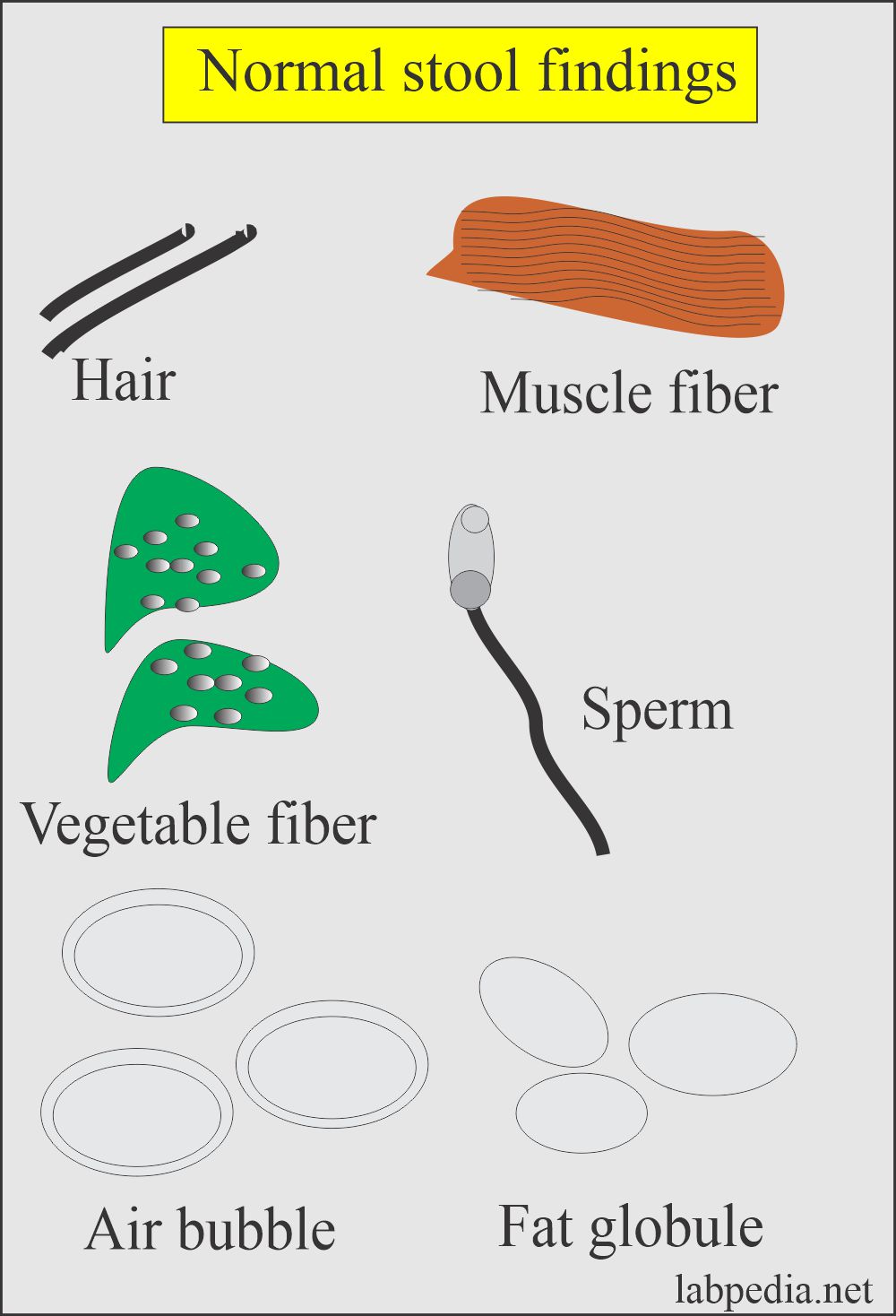
What is the appearance of Undigested food particles?
- Vegetable cells.
- Vegetable fibers.
- Plant hairs.
- Amorphous vegetable material.
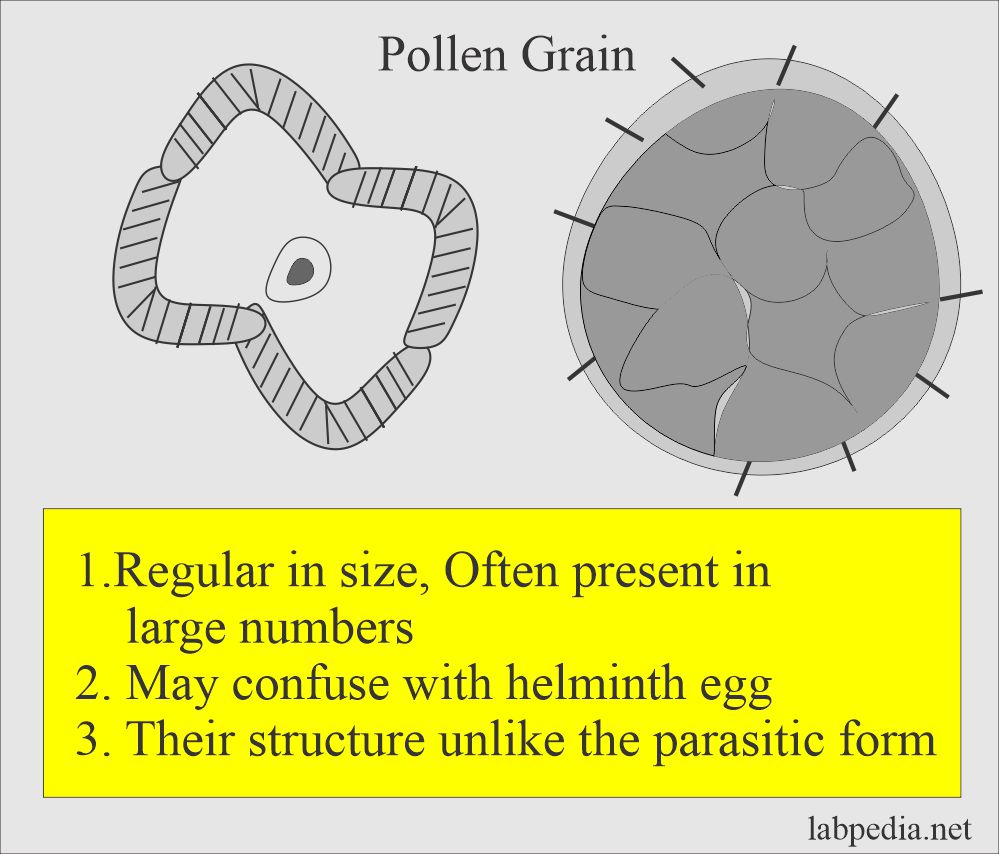
- Pollen grains are regular in size and often present in large numbers.
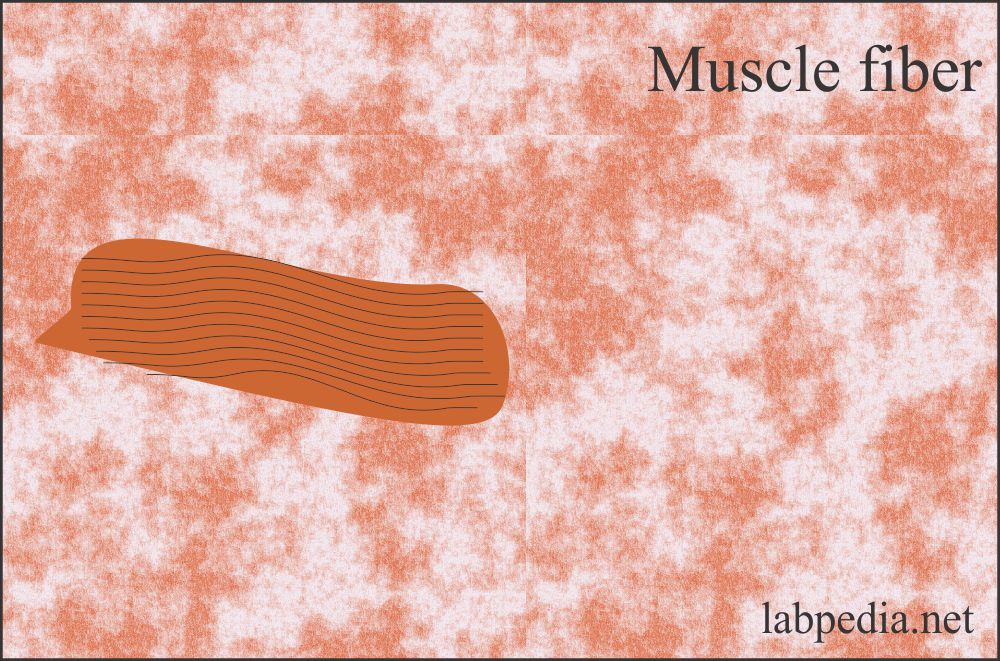
- Muscle fibers:
- These are usually light brown. Sometimes, it may show striations.
- Meat fibers and muscle fibers are seen in the stool. Their presence shows defective indigestion.
- The increased amount of meat fibers is found in:
- Malabsorption syndrome.
- A pancreatic functional defect like cystic fibrosis.
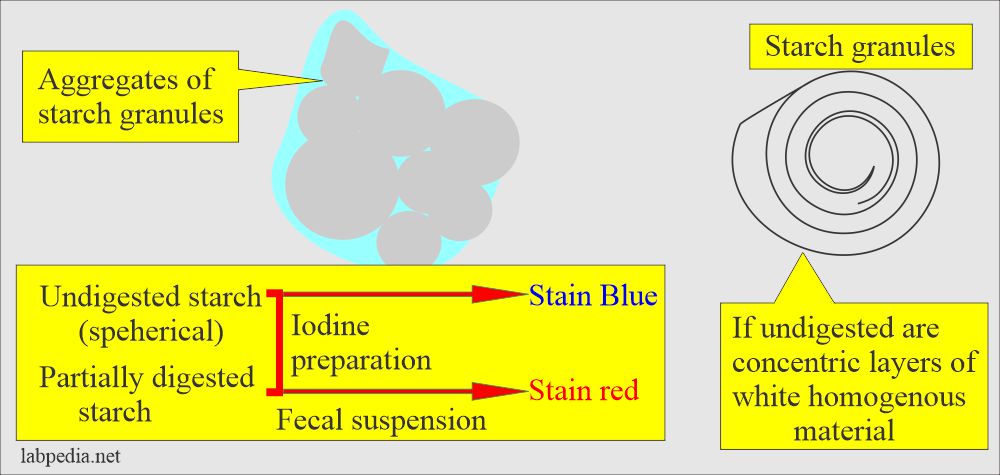
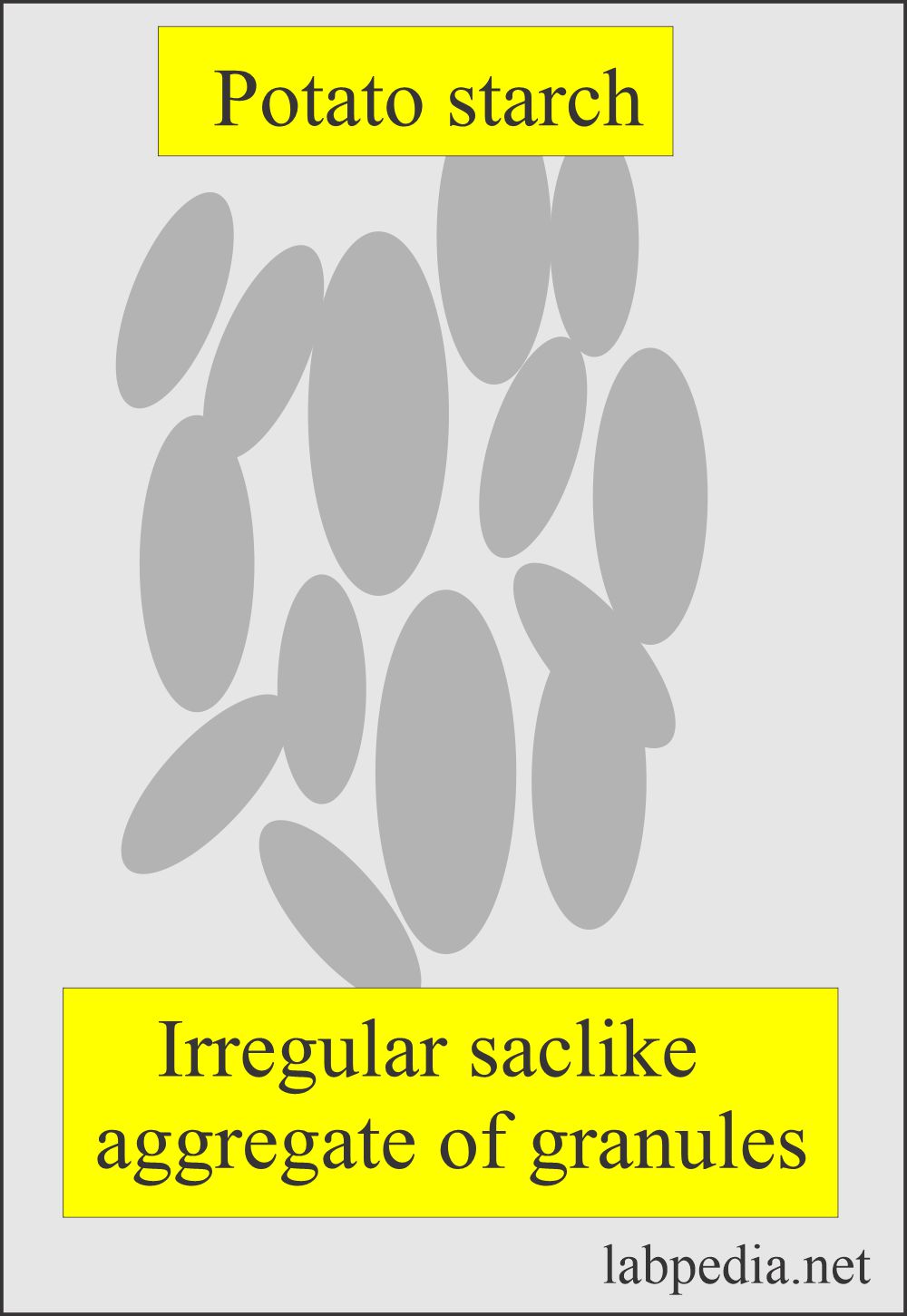
- Starch granules:
- It may be spherical if undigested; they have concentric layers of white, homogenous material.
- Fishbones.
- Water.
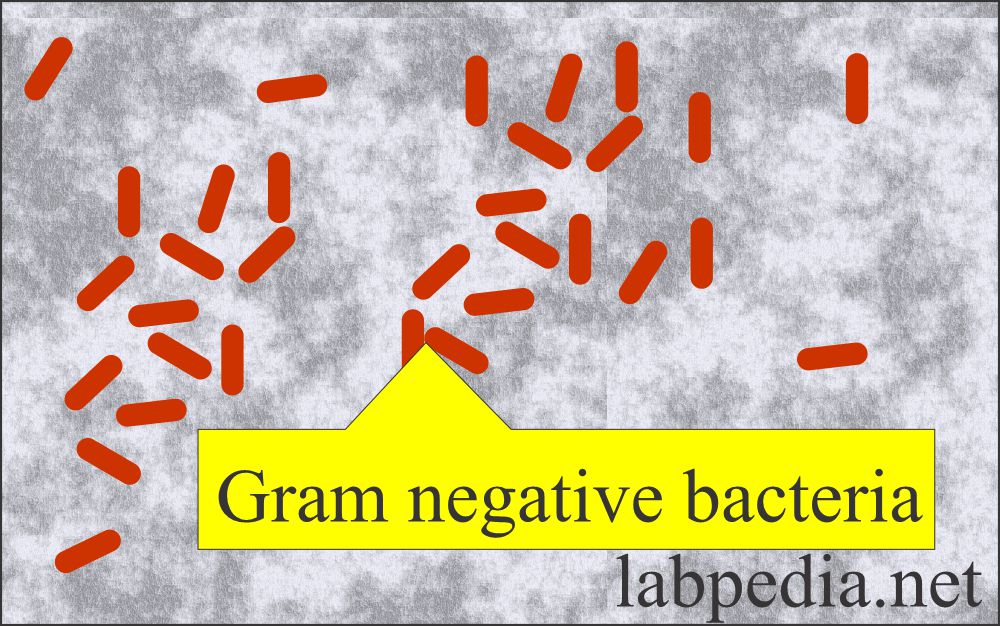
- Bacteria:
- On the stool smear, do the gram stain and see the bacteria. Normally, there are bacteria in the stool.
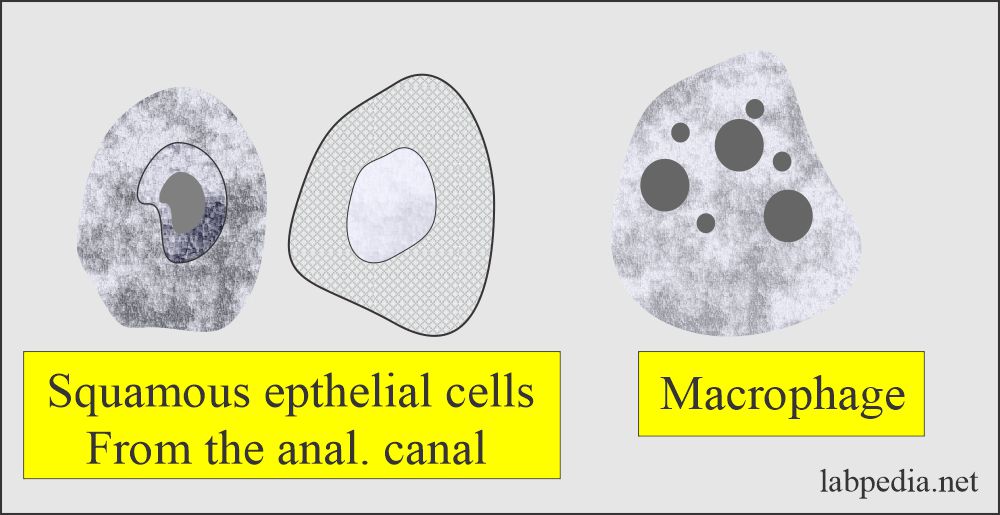
- Desquamated epithelial cells:
-
- This depends upon the size of the nuclei and the cytoplasm. These are usually from the anal canal mucosa.
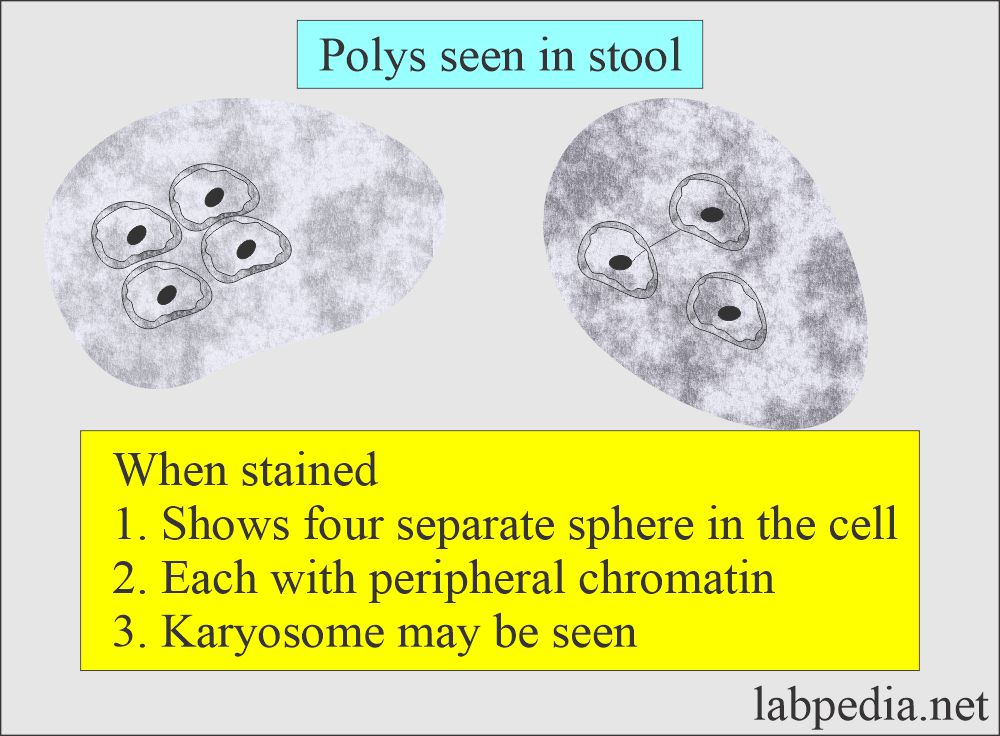
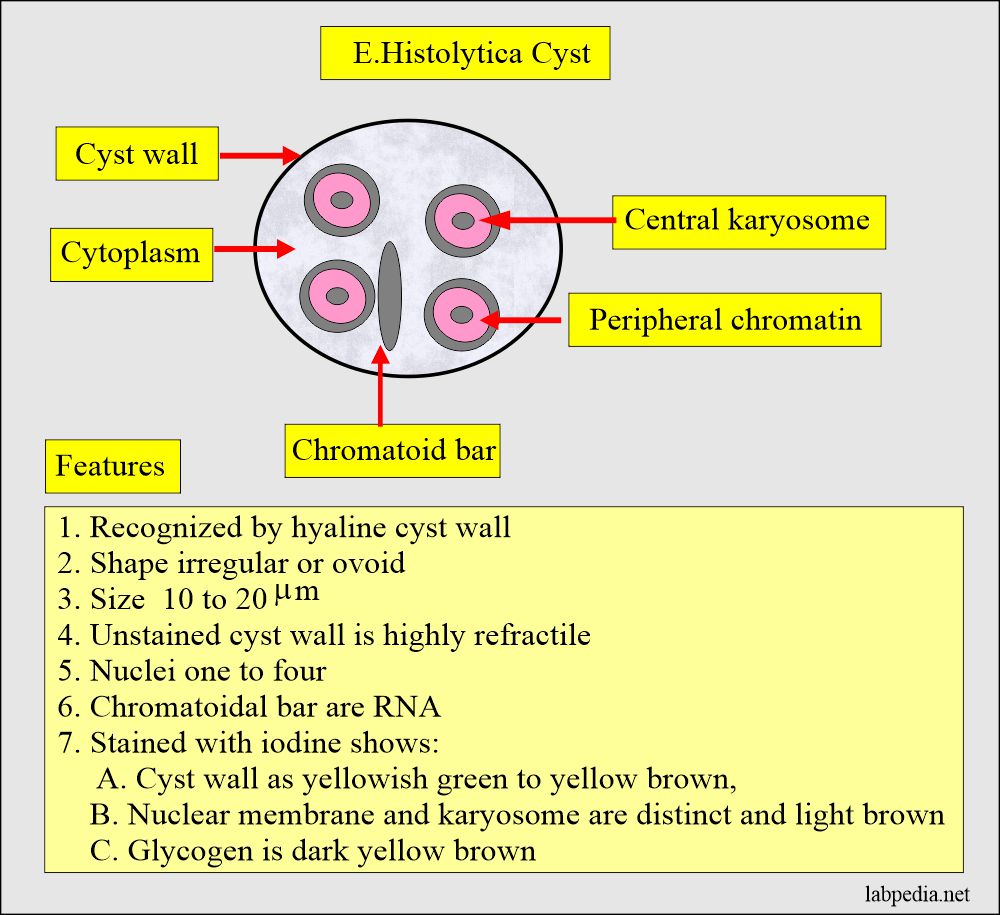
- Polymorphonuclear leucocytes:
- When stained, smears may show a nucleus divided into four separate spheres with peripheral chromatin.
- Also, shows an apparent karyosome.
- The nuclear material is larger in proportion to the amount of cytoplasm compared to the amoebic cyst.
- The shapes of the nuclei are variable.
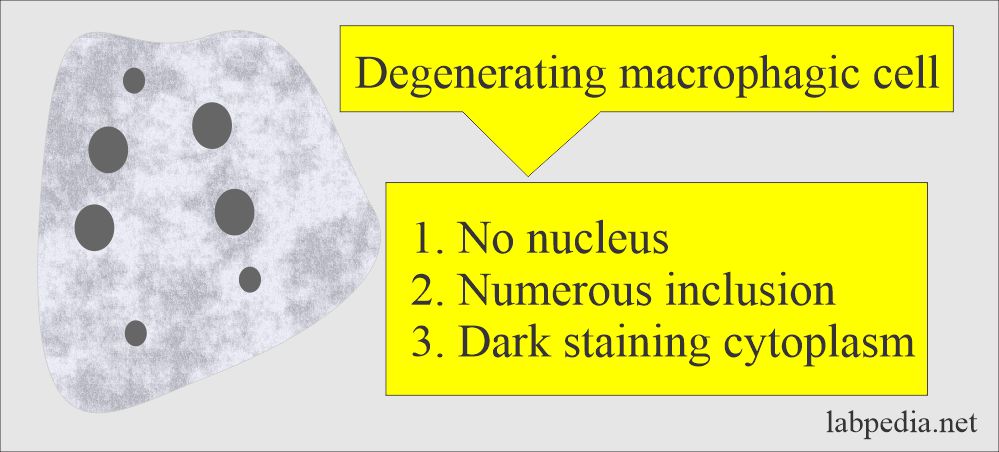
- Macrophagic cells:
- These have numerous inclusions in the dark-staining cytoplasm.
- These need to be differentiated from intestinal amoebae. There are large particles in the cytoplasm.
- The nucleus has no karyosomes.
- Degenerated macrophagic cells lose their nucleus and have few ingested materials.
- Also, the nucleus has a fine network of chromatin and large particles scattered.
What are the digestive tract products?
- Digestive tracts products are like:
- Enzymes.
- Mucus.
- Bile pigments products.
- Digested but not absorbed food.
- Products produced by the decomposition of the stool are:
- Skatole.
- Indole.
- Various gases like H2S, CO2, and nitrogen.
What is the macroscopic or gross appearance of the stool?
- The gross findings of the stool are important. Note the consistency and the color of the stool.
- Try your best to examine the stool as received in the lab. In case of delay, use the preservatives.
- Mushy or liquid stool may suggest the presence of protozoan trophozoites. The best result is obtained if the stool is examined within one-half hours.
- Helminth eggs and larvae are found in liquid or stool. Proglottids or adult tapeworms may be seen grossly.
How will you describe the physical character and appearance of the stool?
| Physical characters | Macroscopic (Gross) appearance |
|
|
|
|
|
|
How will you describe the consistency of the Stool?
- The stool consistency may be:
- Normal is soft and formed.
- Loosely formed stools.
- Watery stools.
- Thin stools.
- Pellet-like stools.
- Dry or hard stools are found in constipated patients.
- Puttylike stools.
- The small, round, hard stool is due to chronic constipation.
- Pasty stools are due to high-fat contents and are seen in:
- Common bile duct obstruction.
- In Celiac disease, the stool looks like aluminum paint.
- Cystic fibrosis is due to pancreatic involvement and is greasy.
- Diarrheal stools are watery.
- Steatorrhea stool is:
- Large in amount.
- Frothy.
- Foul-smelling.
- Constipated stools are firm and may see spherical masses.
- Ribbon-like stool suggests the spastic bowel, rectal narrowing, stricture, or partial obstruction.
- The hard stool is due to excessive water absorption and prolonged contact with the colonic mucosa.
What are the possibilities for stool color?
- The normal color is due to the presence of stercobilinogen and is brown.
- Yellow or yellow-green color is seen in diarrhea.
- Black and tarry (related to consistency) stools are due to bleeding of the upper GI tract from tumors.
- The maroon or pink color is from the lower GI tract due to tumors, hemorrhoids, fissures, or inflammatory processes.
- Clay-colored stools are due to biliary tract obstruction.
- Mucous in the stool indicates constipation, colitis, or malignancy.
- The pale color and greasy appearance are due to pancreatic deficiency, which leads to malabsorption.
What are the causes of the stool’s different colors?
| The color of the stool | Causes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the variables of the quantity of the stool?
- Normally, there is 100 to 200 G/day.
- With a vegetable diet, maybe 250 g/day.
- Many disorders cause large, bulky stools, even in people who don’t eat much.
- Like malabsorption syndrome and carbohydrate indigestion.
- Your stool size has more to do with how well you digest your foods than what you eat.
- Some foods produce larger stools because they don’t break down completely.
- Some gastrointestinal disorders also cause poor food breakdown and absorption, which leads to large, bulky stools.
What are the causes of stool odor?
- The foul odor is caused by undigested protein and by excessive intake of carbohydrates.
- Stool odor is caused by indole and skatole, which are formed by bacterial fermentation and putrefaction.
- A foul odor is sickly produced by undigested lactose and fatty acids.
- The odor is increased due to excess intake of proteins.
- The putrid odor is due to severe diarrhea of malignancy or gangrenous dysentery.
What are the causes of mucus in the stool?
- The mucosa of the colon produces mucus in response to parasympathetic stimulation.
- Pure mucous is translucent, gelatinous material clinging to the stool’s surface. This may be seen in the following conditions:
- Severe constipation.
- Mucous colitis.
- Excessive straining of the stool.
- Emotionally unstable patient.
- Mucus in diarrhea with microscopically present RBCs and WBCs are seen in:
- Bacillary dysentery.
- Ulcerative colitis.
- Intestinal tuberculosis.
- Amoebiasis.
- Enteritis.
- Acute diverticulitis.
- Ulcerating malignancy of the colon.
- Mucus with blood that is clinging to stool is seen in:
- Malignancies of the colon.
- Inflammatory lesion of the rectal canal.
- Excessive mucus was seen in:
- Villous adenoma of the colon.
- This depends upon the dietary intake.
What are the causes of Stool’s physical character?
| Stool findings (Physical features) | Possible Causes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What does the chemical examination of stool include?
- Stool pH.
- Reducing substances.
- For occult blood.
- Presence of fat, carbohydrate, and proteins.
What is an interpretation of the stool pH?
- Normally, stool is slightly acidic, alkaline, or neutral.
- pH is 7.0 to 7.5, depending on the diet.
- Newborn pH = 5.0 to 7.5.
- The pH of the stool depends upon the diet and bacterial fermentation in the small intestine.
- Carbohydrate changes the pH to acidic, while protein breaks down to alkaline.
- The breastfed infant’s pH has a slightly acidic stool.
- Bottle-fed infants have a slightly alkaline stool.
- The pH stool test helps to evaluate carbohydrate and fat malabsorption.
- pH stool also helps to know disaccharidase deficiency.
- What are the causes of Alkaline (Increased pH) stool?
- Colitis.
- Villous adenoma.
- Diarrhea.
- Antibiotic therapy.
- Excess intake of proteins.
- What are the causes of Acidic (Decreased pH) stool?
- Fat malabsorption.
- Disaccharidase deficiency.
- Carbohydrate malabsorption.
- Excess intake of carbohydrates.
- What are the precautions for pH estimation?
- Barium intake and laxatives change the pH.
- If the specimen is contaminated with urine, we must discard the sample.
What are the causes of Fats in the stool?
- The fat in the stool shows the possibility of:
- Malabsorption.
- Deficiency of pancreatic digestive enzyme.
- Deficiency of Bile.
What is the normal amount of Urobilinogen in the stool?
- This is normally found in 40 to 280 mg/24 hours (100 to 400 Ehrlich units/100 gm).
What is the normal amount of Coproporphyrin in the stool?
- 400 to 1000 mg/24 hours.
What is the normal value of Fat in the stool?
- Normally, absent. It is less than 7 grams /24 hours during three days.
- This is less than 30% of dry weight (On a diet of 50 grams of fat per day).
- Normal
- 2 to 6 grams/24 hours (7 to 21 mmol/day).
What is the normal value of Calcium in the stool?
- This is about 0.6 grams / per 24 hours.
What is the normal value of the Stercobilinogen in the stool?
- It is normally 40 to 280 mg/day, averaging 150 mg/day.
What is the normal value of Nitrogen in the stool?
- It depends upon the nature of the diet.
- The normal amount is 1 to 1.5 g/day (<2.5 grams/day).
What will you see in the microscopic examination of the stool?
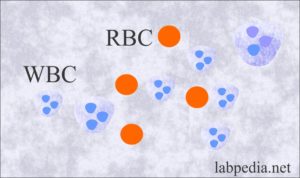
- Presence of leukocytes (pus cells).
- Presence of Red Blood Cells.
- Ova and parasites.
- Presence of meat fibers and muscle fibers.
- Presence of fat.
- Yeast and molds.
- Bacteria.
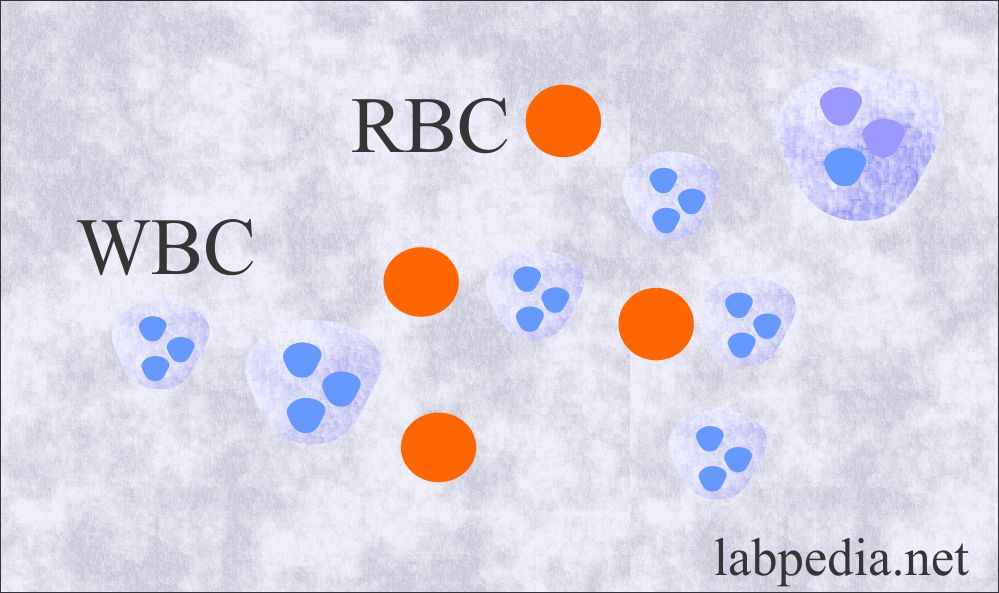
What are the causes of WBCs in the stool?
- Normally, there are no WBCs.
- WBCs only appear in infection or inflammation.
- Their presence is important in case of diarrhea or dysentery.
- >3 WBCs /high fields are seen in ulcerative colitis and bacterial infection.
- Greater numbers of WBCs indicate invasive pathogens.
- Viruses and parasites don’t cause the presence of WBCs in the stool.
- What causes the increased number of WBCs seen in the stool?
- Bacillary dysentery.
- Chronic ulcerative colitis.
- Shigellosis.
- Salmonella infection.
- Yersinia infection.
- Invasive E.coli diarrhea.
- Fistula of anus or rectum.
- Localized abscess.
- Few WBCs are seen in amoebiasis.
- Also, WBCs are seen in typhoid.
What are the conditions where WBCs are absent?
- Cholera.
- Viral diarrhea.
- Drug-induced diarrhea.
- Amoebic colitis.
- Non-invasive E.coli diarrhea.
- Parasitic infestation.
- Toxigenic bacterial infection.
What are the causes of Red Blood Cells in the stool?
- Normally, RBCs are absent.
- Epithelial cells are present, and these are increased with GI tract irritation.
- Few WBCs are seen, which may be increased due to GI tract inflammation.
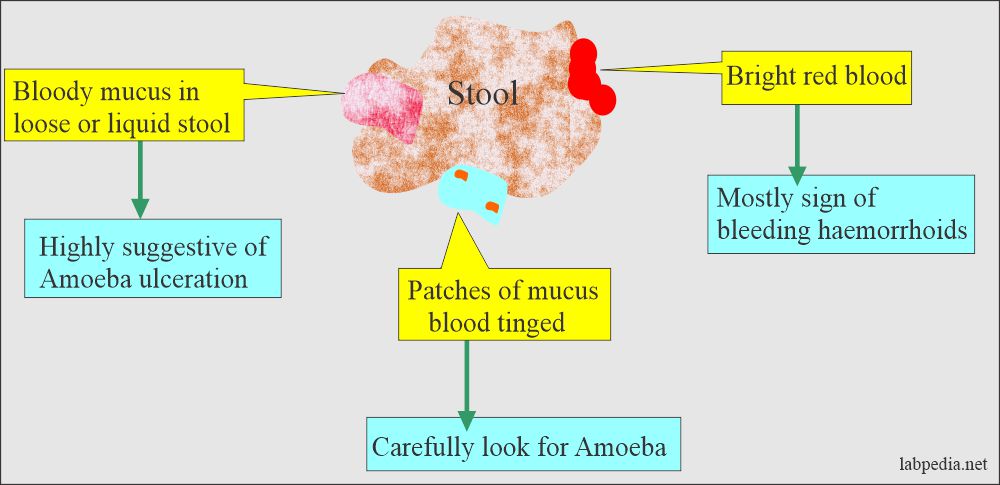
- What is the appearance of blood in the stool?
- Bright red from the bleeding in the lower GI tract.
- Maroon in color.
- Black and tarry from bleeding from the upper GI tract.
- Occult blood (not visible to the naked eye).
- What are the causes of blood in stool?
- Hemorrhoids.
- Cancer.
- Dysentery.
- Make a smear from the mucus or blood-colored area from the watery or semiformed stool.
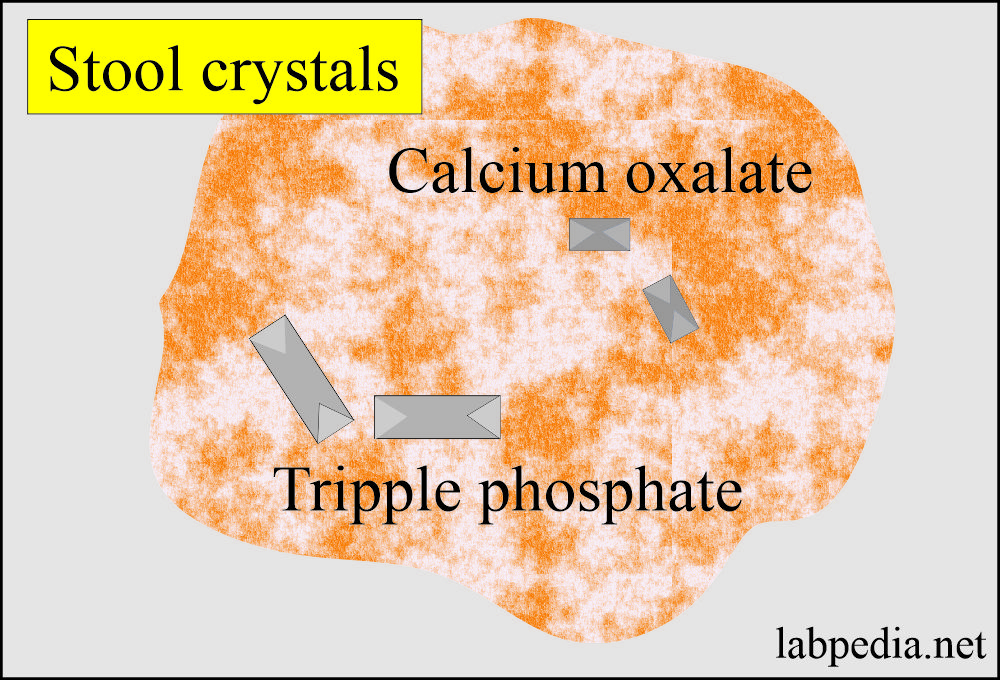
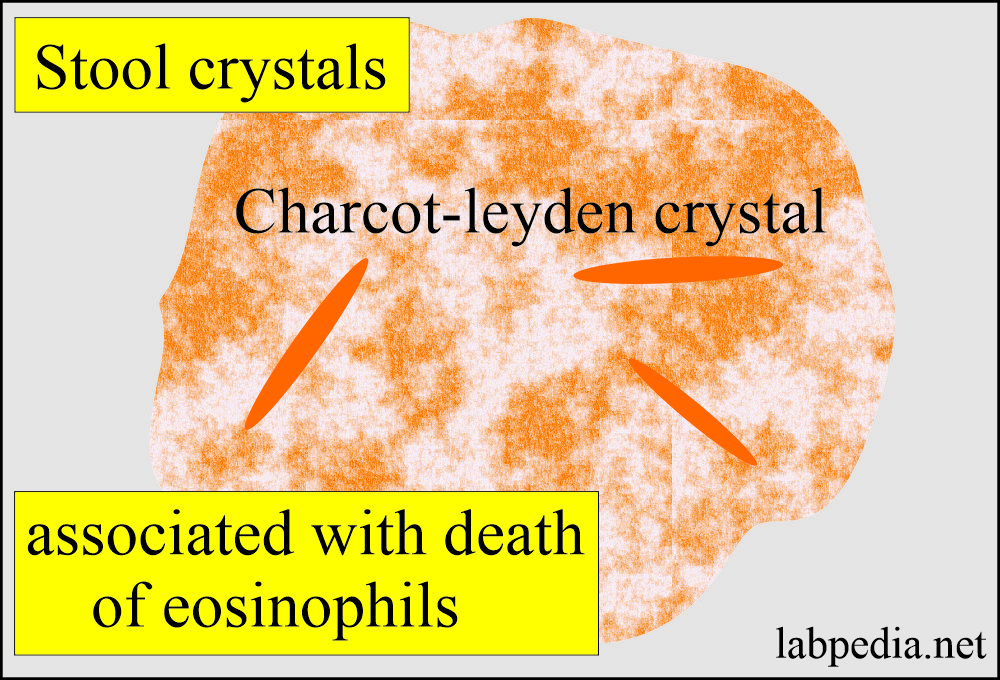
What causes the Presence of crystals and other substances in the stool?
- Crystals of calcium oxalate, fatty acids, and triple phosphate are commonly present.
- Charcot-Leyden crystals are seen in parasitic infestation, especially in amoebiasis.
- Undigested vegetable fibers and meat fibers are seen sometimes.
- Neutral fat globules stained with Sudan may be seen normally at 0 to 2+.
- Hematoidin crystals are sometimes seen after GI tract hemorrhage.
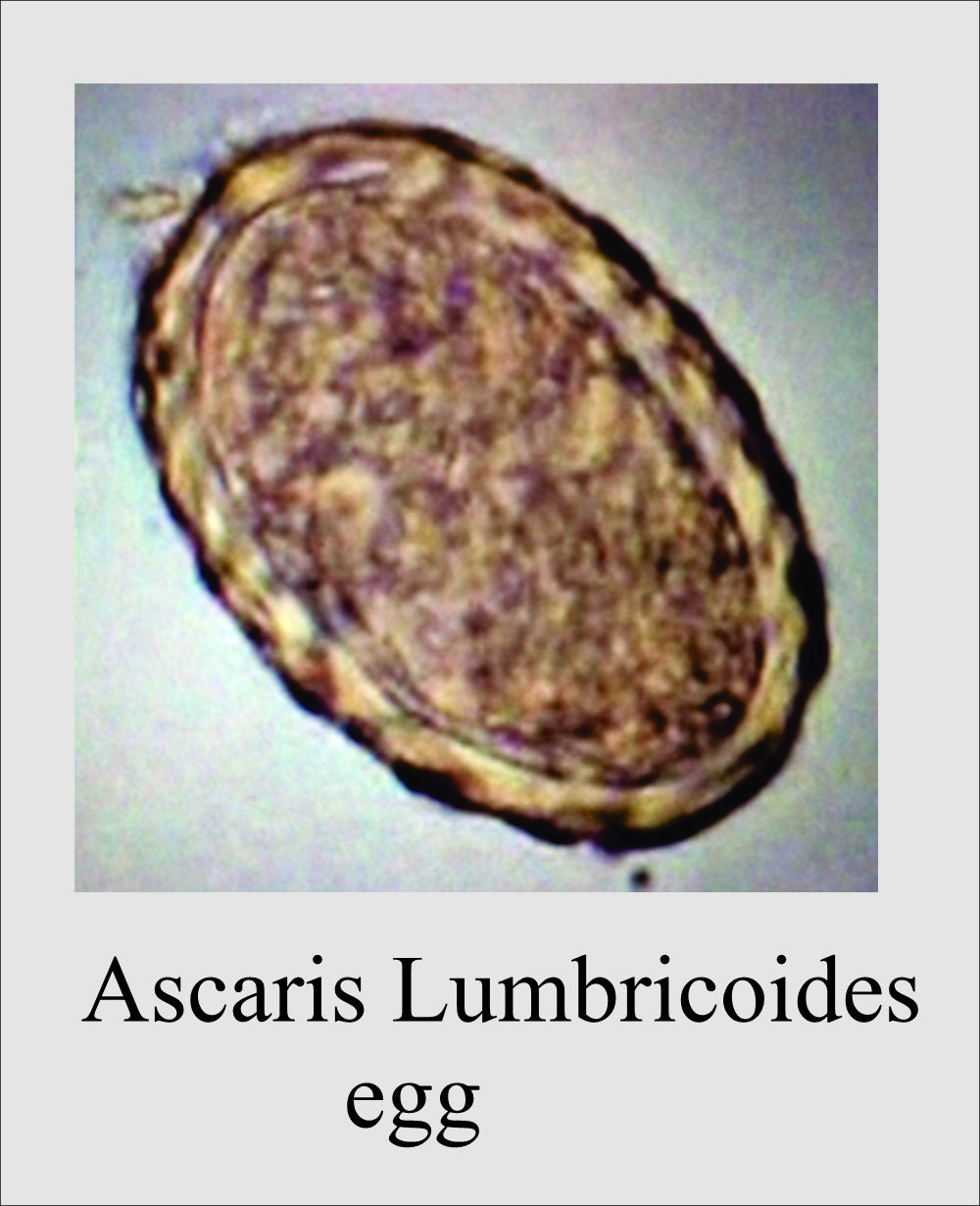
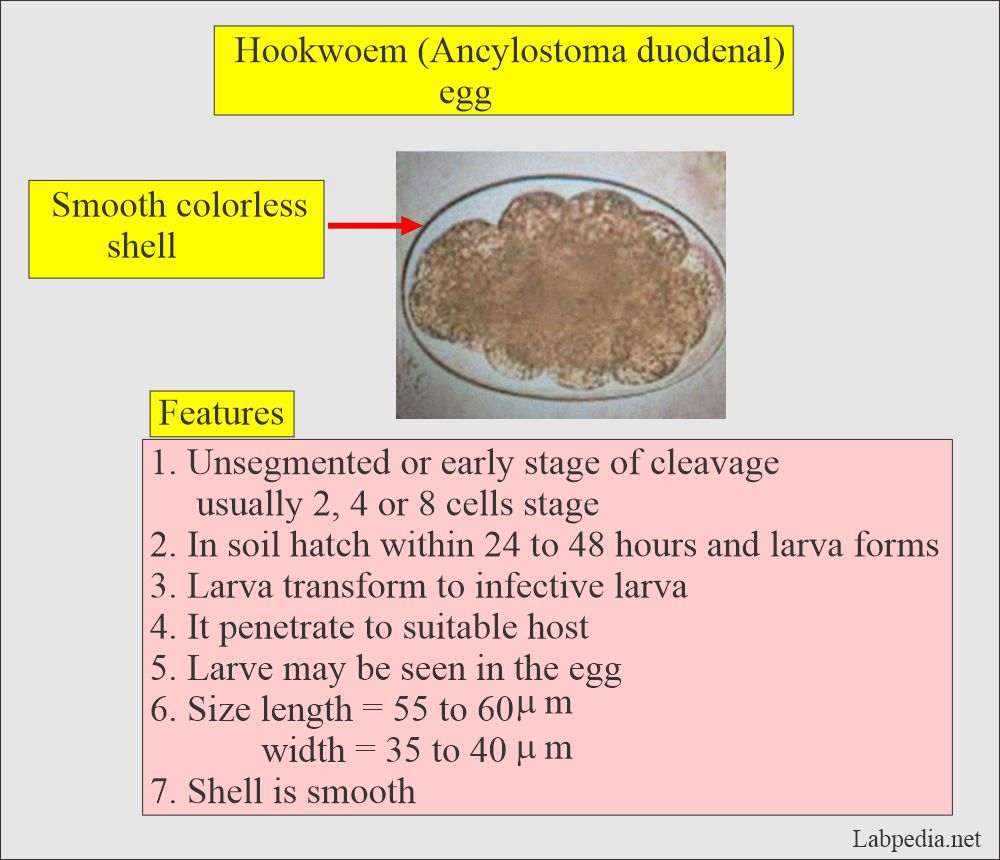
What Ova and parasites are seen in the stool?
- Normally, there are no parasites or eggs in the stool sample.
- Multiple stool samples are needed to rule out the parasitic infestation for at least three consecutive days.
- An abnormal result means parasites or eggs are present in the stool.
- Such infections include:
- Roundworms: Ascaris lumbricoides.
- Hookworms: Necator americanus.
- Pinworms: Enterobius vermicularis.
- Whipworm: Trichuris trichiura.
- Tapeworms: Diphyllobothrium latum, Taenia saginata, and Taenia solium.
- Protozoa: Entamoeba histolytica (an amoeba) and Giardia lamblia (a flagellate)
- Strongyloidiasis.
Summarize the normal stool examination?
| Physical character | Normal values |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Biochemical features | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
20 to 950 units/g |
|
|
|
|
| Microscopic findings | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How would you summarize a normal stool?
- Quantity
- The bulk of the stool is 100 to 200 grams.
- It may be up to 250 grams on a vegetable diet.
- Amount of water
- Normally, up to 75 % of the stool water is present.
- It is interesting that our body also has roughly 75% of water.
- Gross appearance
- Normal is soft and formed.
- Scanty mucous was seen.
- Abundant mucous was seen.
- Mucous with blood seen.
- Grossly fibrous.
- Homogenous appearance.
- Color
- The normal color is yellowish-brown due to the presence of bilirubin and bile.
- In infants, the color is green, and the stool is loose or pasty.
- Various colors depending on diet.
- Clay color stool is seen in biliary obstruction.
- Tarry stool is seen if more than 100 ml of blood comes from the upper GI tract.
- The red color is due to blood in the large intestine, undigested beets, or tomatoes.
- The black stool is seen due to blood, iron, or bismuth medication.
- Consistency may be:
- Soft.
- Formed.
- Semiformed.
- Hard.
- Loose.
- Diarrheal.
- Watery like a fluid.
- pH
- This is from 7.0 to 7.5.
- This may be acidic with high lactose intake.
What does the routine stool examination consist of?
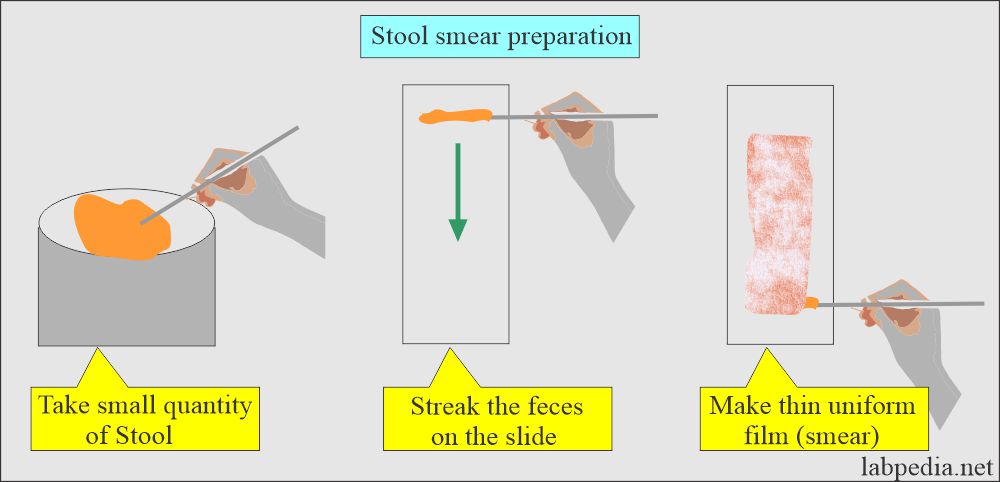
- Direct wet film.
- Saline: You can make a smear with normal saline.
- Check the clarity of the saline solution microscopically.
- Iodine preparation is used to identify cysts in the stool.
- Keep the iodine solution in dark brown bottles with tight caps.
- Methanol is used to fix the slide.
- Concentration method.
- Permanently stained slide.
- The stained slide can be preserved using the DPX, permount, or Hystomount.
- Place a drop of the above preservatives over the stained slide and leave it to dry.
- After drying, remove the excess of the mount.
- These smears can be kept for several years.
-
The following drawing shows how to make a thin smear for a permanent stain.
What are some examples of parasites?
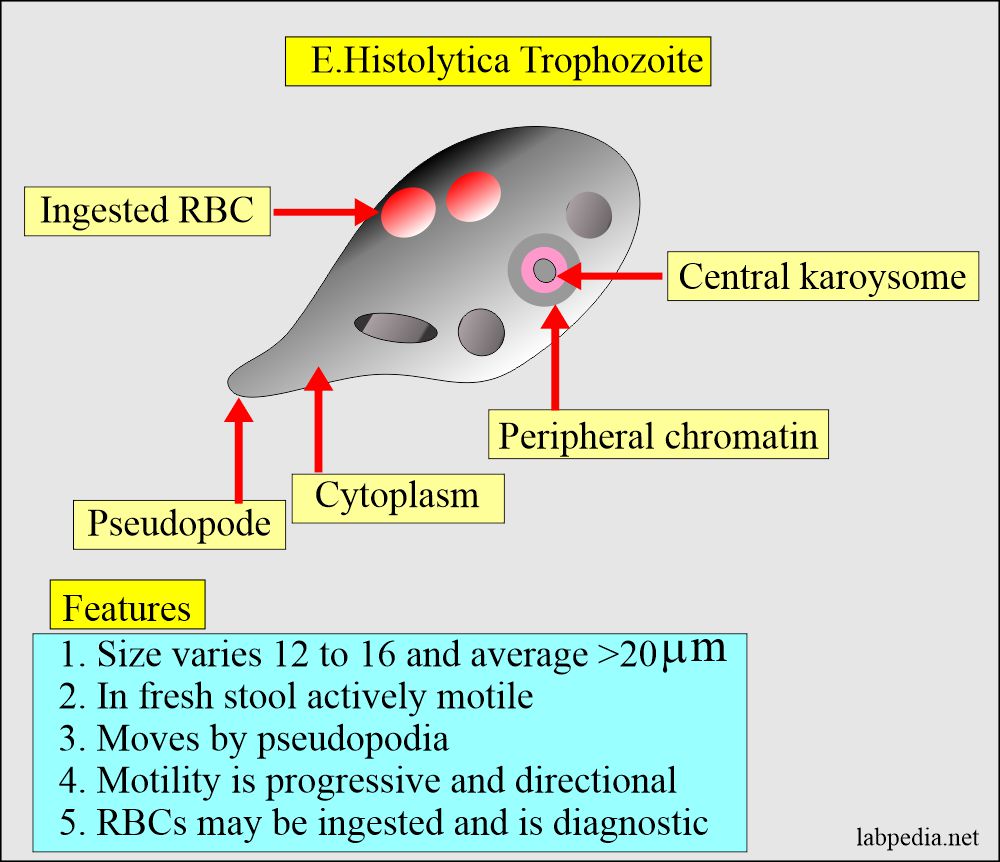
Stool examination: Stool E. Histolytica trophozoite
What are the Important facts about the stool examination?
- The intestinal protozoan is usually found in soft and liquid stools.
- Cysts are rarely found in liquid stool.
- Cysts are found in the formed stool.
- Helminth eggs are found in liquid or formed stool.
- Liquid stools are diluted, so difficult to find these parasites.
- Examined the surface of the unpreserved stool for macroscopic parasites.
- Pinworms are seen at the surface, and tapeworms are in the stool’s interior.
- The freshly passed stool is essential for the detection of amoebae or flagellate.
- Should examine all liquid or soft stools within 30 minutes of the collection.
- Formed stool immediate examination is not critical; it can wait 3 to 4 hours.
Questions and answers:
Question 1: What is the normal pH of the stool.
Question 2: What is the effect of the high fiber diet.
Question 3: How much fats goes in the stool.
Question 4: Which crystal is seen in parasitic infestation in the stool.
- Note: Stool study is continued.



While doing the microscopic examination of stool specimen, you have noticed that there are many epithelial cells and few calcium crystals found per field. What action you will do?
Maxamud
Medical laboratory
Please let me know what you want about the topic you mentioned.
Is sperm normal in stool?
Not at all. Sperms are abnormal in the stool.
Hi Dr. Riaz!
Fecalysis of a 4 year old/female
Color: Brown
Consistency: Soft
Red blood cells: 0-1/HPF
Pus cells: 0-1/HPF
Bacteria: Few
Yeast cells: None
Parasite: No ova or parasite seen
Others: None
Thank you!
This stool examination looks normal.
I have a stool sample here, and I can’t tell if these are fat globules or eggs of some kind? Also I have a picture I think of intestinal worm but I’m not sure. Thank you for looking.
https://adobe.ly/3Z4P86Y
I have seen all your photos; I think these are foo/vegetable/fat globules particles. I do not think that any of these are parasites.
Thank you!
RiazCancel
Assalam o alaikum…. I have done few times my stool dr I just found many times just undigested food or vegetable cells before that I hear from my teacher unfertilized ova of ascaris lumbricoids but I was not satisfied and I done many times research and I found my answer it’s was just a veg cells I found and I did D/R civil hospital govt than I just read remarks undigested food so what is the solution for that Im weak not I had lost my weight in few years and not growing.
Please check your Fasting blood glucose and HbA1c.
undigested food veg cells
Good
Good Procedures of stool examination
Thanks.