Rubella infection (German Measles), Rubella Antibody Tests
Rubella Infection (German Measles)
What sample is needed for Rubella Antibody Tests?
- The Serum of the patient is needed.
- A random sample can be used.
- The virus can be found in the washings of the throat.
- The virus is found in the CSF, urine, amniotic fluid, and other sites in congenital infection.
What are the Indications for Rubella Antibody Tests?
- It diagnoses the rubella infection.
- It is done to find the immune status of the patient.
- It is advised in pregnant ladies.
- It may be advised in low-weight babies.
How will you describe Rubella’s history?
- Historical facts:
- Rubella virus was first isolated in 1962.
- Three live attenuated vaccine strains were developed and licensed in the USA in 1969.
- In 1964 >20,000 cases of congenital rubella syndrome and an unknown number of stillbirths occurred in the USA.
How will you define rubella infection?
- Rubella virus infection is also called German measles.
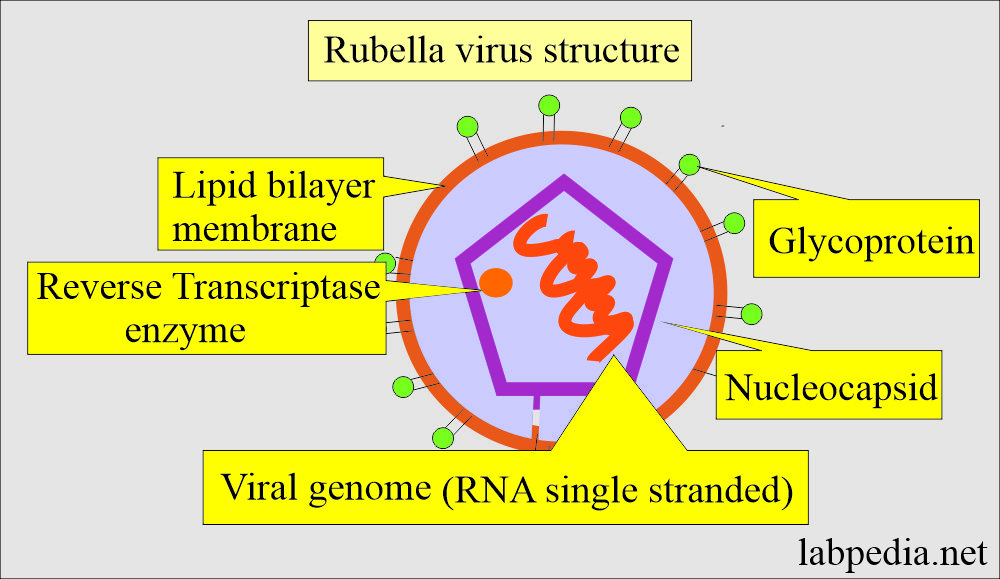
- Rubella virus is a single-stranded RNA Rubivirus.
- This is an acute episodic disease with the onset of generalized maculopapular rashes and a fever of >99 F.
- Rashes are not as prominent as in measles.
- There may be arthritis and arthralgia.
- Also, there may be lymphadenopathy and conjunctivitis.
- Lymphadenopathy mostly involves the posterior occipital area.
What is the role of Rubella infection in pregnant women?
- Infection in the first trimester is associated with congenital abnormalities, abortion, or stillbirth in 30% of the patients.
- ≤80% of patients show this association during the first month.
- 25% to 50% of the cases are subclinical.
What is the structure of the Rubella virus?
- Rubella is also called German measles or three-day measles.
- This belongs to the Togavirus group.
- This is the RNA virus and is 60 nm in diameter.
- The envelope possesses a hemagglutinin.
How does the spread of Rubella infection take place?
- This is a contagious viral infection.
- This benign disease is spread by droplet infection and enters the body through the respiratory route.
- After 3 weeks rash appears, and now the antibody can be demonstrated in the blood.
- This is best known for its distinctive red rash.
- Rubella is not the same as measles, called Rubeola, a serious disease.
- Both of these diseases have common symptoms of rashes.
- Nowadays, children are given MMR (measles, mumps, and rubella) vaccines.
- Children in the United States are given vaccination twice before they reach school age, which is highly effective in preventing rubella.
- Children are given the first MMR dose at 12 to 15 months of age and the second dose at 4 to 6 years of age.
- CDC has declared rubella eliminated in the United States.
What is the pathogenesis of Rubella virus infection?
- Viralemia occurs 5 to 7 days after exposure to the virus, and it spreads to various organs and tissues.
- In the case of pregnancy, if there is an infection, then there are chances for congenital abnormalities in the fetus.
- There are chances for abortion or stillbirth.
- 25% to 50% of the cases, the disease is subclinical.
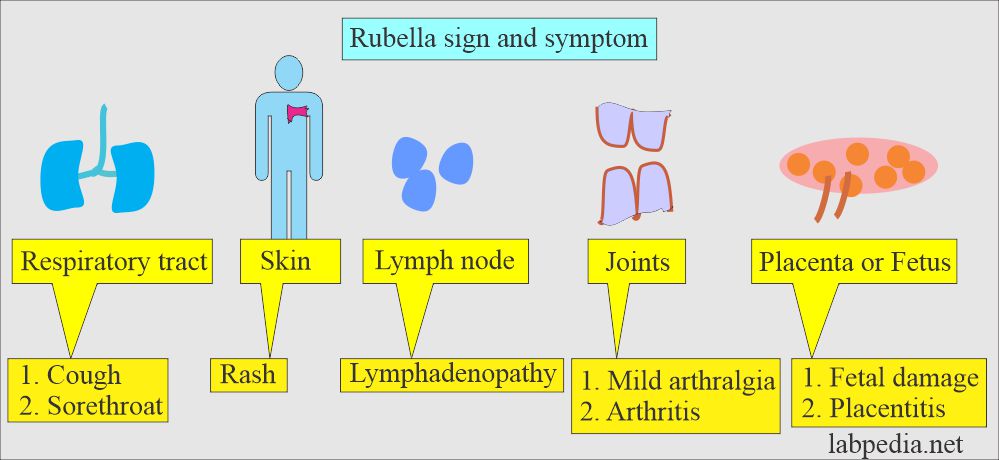
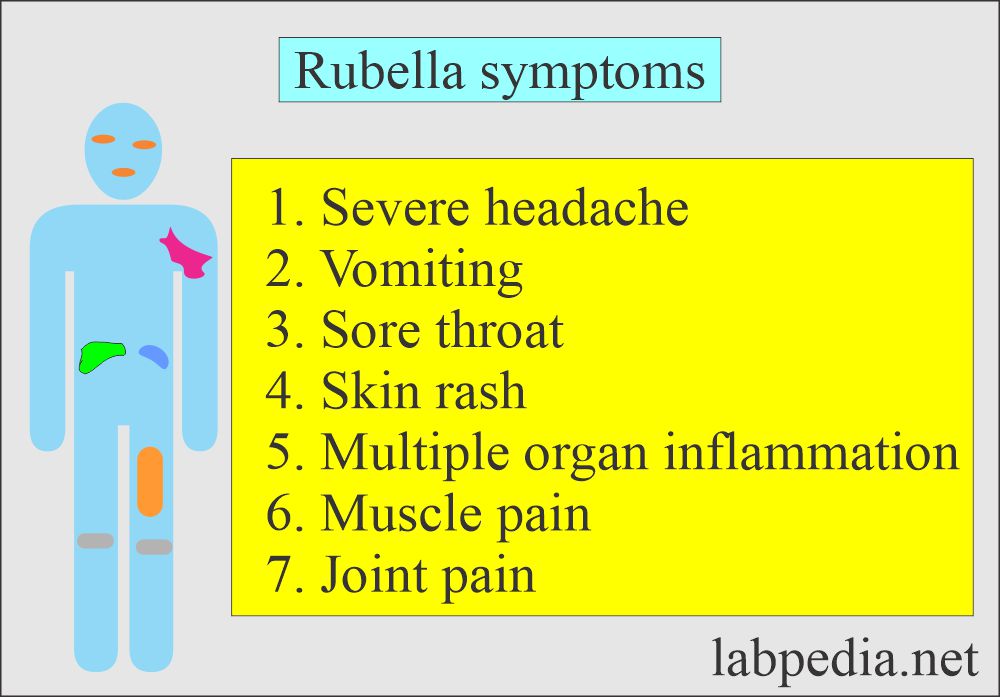
What are the signs and symptoms of Rubella infection?
- The signs and symptoms vary from person to person. A mild rash may cause the diagnosis to be missed.
- Rubella infection may resemble drug-induced rashes and infectious mononucleosis.
- The incubation period varies from 10 to 21 days, and the typical period is 12 to 14 days.
- The infectious patient is contagious for 12 to 15 days, beginning 5 to 7 days before the rash appears.
- Acute rubella infection lasts 3 to 5 days and requires little treatment.
- There is a prodromal period of catarrhal symptoms, followed by retroauricular, posterior cervical, and postoccipital lymphadenopathy.
- These patients have a fever, usually less than 101 °F, followed by a maculopapular rash for 2 to 3 days.
- The rash starts on the face and spreads to the rest of the body.
- The patient may have a sore throat, tiredness, loss of appetite, muscle and body aches, and chills.
- In older children and adults, self-limiting arthralgia and arthritis are common.
What is the mode of transmission?
- This disease is spread by contact with an infected person through coughing and sneezing.
- It spreads through respiratory secretions.
What are the normal levels of Rubella antigen/antibody?
Source 1
- The serologic tests are used to determine the following:
- The immune status of the individual.
- Diagnose postnatal rubella.
- Occasionally to support the diagnosis of rubella.
- IgM antibody disappears within 4 to 5 weeks.
- IgG antibody remains for life.
- For Diagnosis, EIA is the preferred method, while others are acceptable.
Source 2
Latex agglutination method
- This is rapid and convenient.
- Normal = Negative for IgG and IgM antibodies.
- IgG positive indicates previous exposure or current immunization.
- IgM positive indicates current or recent infection.
HAI (Hemagglutination inhibition method)
- <1:8 = No immunity to infection.
- >1:20 = Immunity to rubella infection.
- The disadvantage is that it detects both IgM and IgG.
ELIZA
- IgM = >1.1 IU/mL = indicates active infection.
- IgG = <7 IU/mL = Indicates No immunity to rubella.
- IgG = >10 IU/mL = indicates immunity to rubella.
Semiquantitative immunoassay method
-
- This is an indirect enzyme-labeled immunoabsorbent assay using microwells of a solid phase.
How is the Rubella disease spread?
- The reservoir is human.
- The mode of transmission is through:
- Person-to-person contact.
- It spreads through respiratory tract secretions.
- If there is direct contact with the lesion.
What are the types of Rubella infection?
Acquired infection:
- The incubation period of acquired rubella infection varies from 10 to 21 days, typically 12 to 14 days.
- The infected person is contagious for 12 to 15 days, beginning 5 to 7 days before the appearance of a rash (if present).
- Acute rubella infection lasts 3 to 5 days and generally requires little treatment.
- Permanent effects are extremely rare in acquired infections.
- The clinical presentation of acquired rubella is usually mild.
Congenital infection:
- Rubella virus is teratogenic if the mother is infected during the first trimester.
- During Viremia, viruses cross the placenta to cause disease in the fetus.
- This is usually a mild infection, a self-limiting disease with only rare complications in children and adults.
- Pregnant women infected in the first trimester of women can have a devastating effect on the fetus.
- In utero, a fetus may have death or rubella syndrome.
- The congenital abnormalities are the following:
- The cardiovascular system shows patent ductus arteriosus.
- Eyes show cataracts and glaucoma.
- The central nervous system shows mental retardation and deafness.
What are the groups requiring the immune status?
- Preschool and school-aged children.
- All females at or just before the childbearing age.
- All women are to be married.
- In the case of a married woman, if she is not vaccinated, then she should be vaccinated and avoid becoming pregnant for at least three months because there is a remote possibility that the fetus may be infected.
- Pregnant women are not positive for rubella immunity. To avoid any infection in fetuses, advise the IgM antibody test. If she is not vaccinated then try to avoid exposure to rubella infection.
- Healthcare workers should be vaccinated to prevent the spread of infection to pregnant women.
What are the complications of Rubella infection?
- If the pregnant woman develops rubella infection in the first trimester, complications are devastating for the fetus.
- Complications of birth defects in a pregnant woman:
- Deafness.
- Cataracts.
- Heart defects.
- Mental retardation.
- Liver and spleen damage.
- Rubella syndrome when the following complications are seen:
- Encephalitis.
- Microcephaly.
- Hepatomegaly.
- Splenomegaly
- Bone defects.
- Mental retardation.
- Cataract.
- Thrombocytopenic purpura.
- Cardiovascular defects.
- Stillbirth.
- At least a 20% chance of damage to the fetus if a woman is infected early in pregnancy.
- Increased chances of spontaneous abortion and stillbirth.
What is the outcome of Rubella infection?
- Utero-infection can result in the death of the fetus.
- First trimester chances of anomalies = around 25%
- Second trimester = <1%
- First month = 50% ±
- Second month = 25% ±
- Third month = 10% ±
- Infected infants shed viruses for up to one year.
What is the immunology (serology) of Rubella infection?
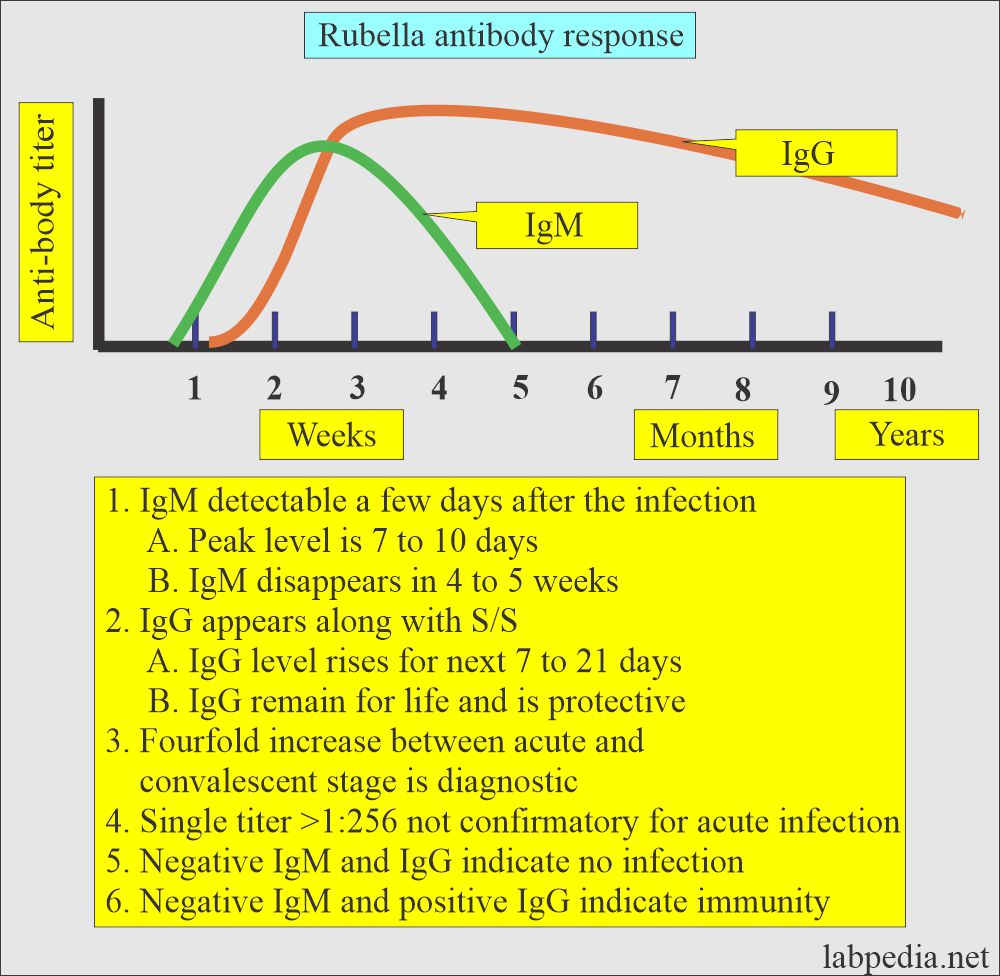
- The formation of antibodies IgM and IgG against rubella is also observed.
- If IgG and IgM are negative, the patients never suffered from rubella infection and have not been vaccinated.
IgM appears in a few days to weeks after the onset of the rubella rash (11 to 25 days). It may persist for ≤1 year.
- IgM disappears in about 6 weeks.
- For active disease, advise IgM.
- To identify congenital infection, advise IgM.
- IgM is necessary to label acute infection.
- IgM can not cross the placental barrier. Therefore, the presence of IgM in the neonatal period is diagnostic of congenital rubella syndrome.
- IgM will be positive for at least 6 months in the newborn to confirm the rubella infection.
- IgM is the best test for congenital or recent infection during the first 6 months of life.
- IgM was detected 15 to 25 days after the vaccination in ≤80% of the cases.
IgG persists at a low level and is detectable for years.
- For immune status, advise IgG.
- IgG titer of 1:8 or more indicates past infection and future protection from the rubella infection.
- Titers of 1:8, 1:16, 1:64, and 1:512 or greater are found in acute and past infections.
- IgM should be advised to use the same serum sample to confirm acute infection.
- IgG can cross the placental barrier and enter into fetal circulation.
- IgG appears after 15 to 25 days of the infection and >25 to 50 days after the vaccination.
- Less than 1/3 of the cases show no IgG after ten years of the infection.
- The absence of IgG-antibody excludes congenital infection.
Acquired infection:
- In the case of primary rubella infection, the presence of IgM and IgG antibodies is associated with the appearance of clinical signs and symptoms.
- IgM is detectable a few days after the onset of S/S and reaches a peak level at 7 to 10 days.
- These antibodies persist but decrease in concentration over the next 4 to 5 weeks until these antibodies are not detectable.
- IgG remains present and protective indefinitely.
Congenital infection:
- IgG can cross the placental barrier, so it cannot distinguish between fetal and maternal IgG antibodies in neonatal blood.
- IgM testing is not valuable as it can not cross the placental barrier.
How would you diagnose Rubella infection?
- Latex agglutination.
- Hemagglutination inhibition (HAI).
- Passive hemagglutination (PHA).
- Enzyme Immunoassay for IgM.
- Enzyme immunoassay for IgG.
- Radioimmunoassay (RIA).
- Fluorescent immunoassay (FIA).
What is the Prevention of the Rubella infection?
- Vaccination is needed.
- A vaccine, as a live virus, is part of MMR.
Questions and answers:
Question 1: What is the importance of IgG in Rubella infection?
Question 2: What is the mode of spread of Rubella infection?