Porphyrias, Porphyrins, Porphobilinogen
Porphyrias
What sample is used to diagnose Porphyrias?
- Collect fresh urine.
- Random urine can be used.
- Protect the sample from light.
- Add 5 g Na2CO3.
- Store the sample at 4 to 8 °C.
What are the Indications for Porphyrias?
- This test will quantify porphyrins and porphobilinogen.
- This can be used to find various forms of porphyria.
How will you define Porphyrias?
- Acute porphyrias are inherited disorders of heme synthesis characterized by an acute attack of neurovisceral symptoms.
- It is life-threatening and diagnosed by a raised level of porphobilinogen in the urine.
- A partial deficiency of the heme biosynthesis enzymes will increase the formation and excretion of porphyrins, their precursors, or both.
- Porphyrias are a group of disorders characterized by a deficiency of or defect in the enzymes involved in porphyrin metabolism and heme synthesis.
- Porphyrias are a group of inherited metabolic diseases caused by defects in heme synthesis.
- What are the types of porphyrins?
- Uroporphyrin.
- Coproporphyrin.
- Protoporphyrin.
- Porphyrias are diagnosed by the pattern of porphyrins and their metabolites in urine, stool, plasma, and RBCs by:
- Plasma fluorescence screening.
- Measuring deficient enzyme.
- Genetic testing.
- >80% of heterozygotes are asymptomatic.
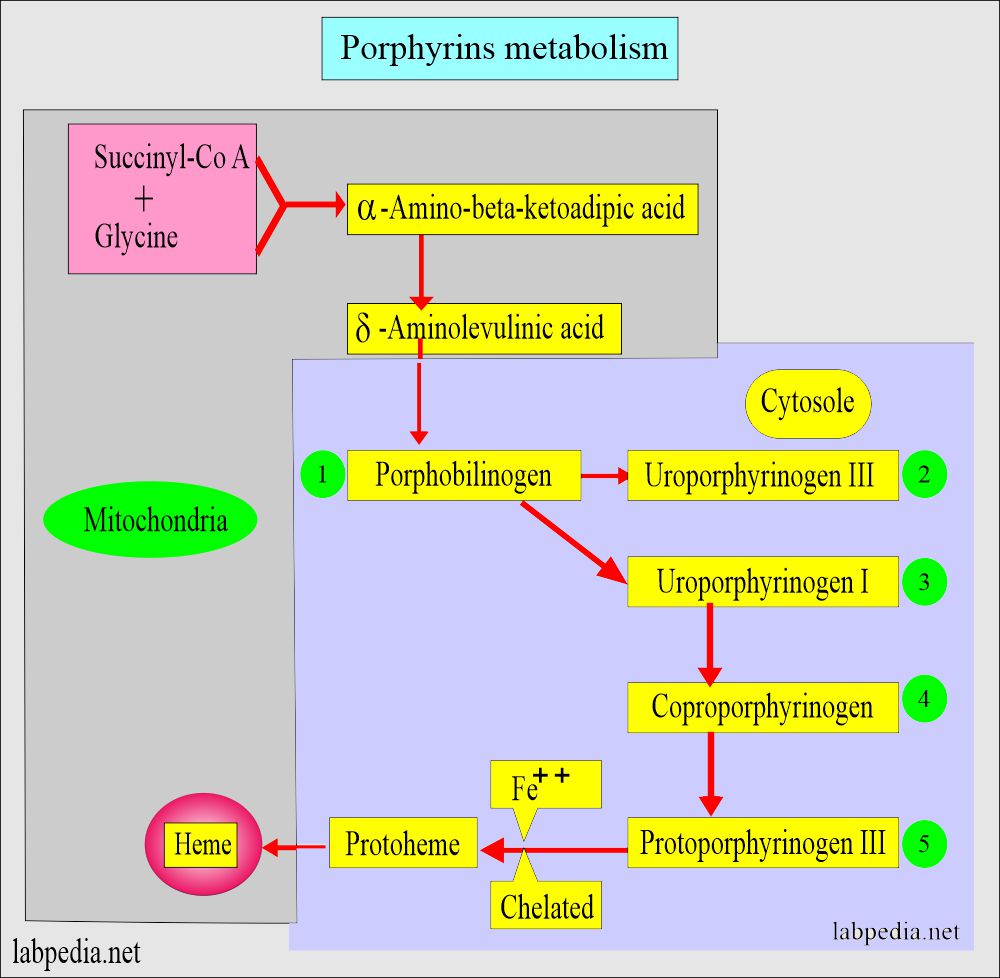
How will you discuss the Pathophysiology of Porphyrias?
- The term “porphyria” is derived from the Greek word porphyria, meaning “purple pigment.”
- Porphyria is a group of disorders that result in an accumulation of chemicals called porphyrins in the body.
- This is a group of genetic abnormalities with associated enzyme deficiency involved in the porphyrin synthesis or metabolism.’
- The porphyrins are building blocks in the synthesis of heme.
- Porphyrins are a byproduct of heme synthesis.
- There is overproduction of the intermediates of the pathway.
- These intermediates are excreted in the urine, feces, or both.
- The excess of porphyrins precursors is associated with potentially fatal acute neurovisceral attacks like:
- 5-aminolevulinic acid (ALA).
- Porphobilinogen (PBG).
- Initiating the acute attack of porphyrias are the following:
- Drugs.
- Alcohol.
- Starvation.
- Hormones.
- Infections.
- Stress.
- There is a deficiency of the various enzymes in the synthesis of heme. Some of the examples are:
- 5-Aminolevulinate synthase.
- 5-Aminolevulinic acid dehydratase.
- Hydroxymethylbilane synthase.
- Uroporphyrinogen-III synthase deficiency leads to Erythropoietic porphyria.
- Uroporphyrinogen Decarboxylase deficiency leads to Porphyria cutanea tarda.
- Coproporphyrinogen Oxidase deficiency leads to Hereditary coproporphyria.
- Protoporphyrinogen dehydrogenase deficiency leads to Variegated porphyria.
- Ferrochelatase leads to Erythropoietic protoporphyria.
What is the mechanism of the toxic action of porphyrias?
- Porphyrins are the main precursors of heme, an essential constituent of hemoglobin, myoglobin, catalase, peroxidase, respiratory, and P450 liver cytochromes.
- Accumulation of porphyrins, the heme precursors, is toxic to tissue in high concentrations.
- The primary porphyrins of RBC are :
- Protoporphyrin.
- Uroporphyrin.
- Coproporphyrin.
- The primary porphyrins of RBC are :
- Then, heme combines with globin in the RBC, and hemoglobin is formed.
- Porphyrias are classified according to the location of the accumulation of porphyrins and precursors.
- In most porphyrias, there is an increased level of porphyrins and porphobilinogen in the urine.
How will you classify porphyrias?
- Symptomatically, acute porphyrias.
- Primarily present with nervous system involvement.
- Often with severe abdominal pain and vomiting.
- Neuropathy and mental disturbances.
- Cutaneous porphyrias present with :
- Skin manifestations often occur after exposure to the sun due to the accumulation of excess porphyrins near the skin’s surface.
The most common classification of porphyria:
- It is based on the accumulation of heme precursors in the liver or bone marrow and red blood cells.
- Hereditary Hepatic porphyria:
- These are subdivided into:
- A. Acute intermittent porphyria (Swedish genetic porphyria).
- B. Variegate porphyria.
- C. Hereditary porphyria.
- It has S/S of :
- All three types are inherited as autosomal dominant.
- All three may be associated with episodes of acute porphyric attacks.
- Acute neurological attacks (seizures, psychosis).
- Extreme back and abdominal pain.
- Acute polyneuropathy.
- These are subdivided into:
- Erythropoietic porphyria:
-
- It has S/S of :
- These are rare congenital disorders.
- Skin problems, usually a light-sensitive blistering rash and increased hair growth.
- There is no skin vesicle formation.
- The teeth are discolored, and they fluoresce under ultraviolet light.
- There may, in some cases, mild hemolytic anemia.
- Diagnosis: The best test is RBC porphyrin measurement.
-
- Porphyria cutanea tarda shows the following signs and symptoms :
-
- Photosensitivity of eyes and skin.
-
- Mixed porphyria.
- Acquired toxic porphyria.
How will you summarize the classification of Porphyria?
| Type of the porphyria | Onset of Porphyria | Inheritance | Psychologic/abdominal pain | Photosensitivity/skin lesion | Enzyme defect |
Hepatic
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Erythropoietic
|
|
|
|
|
|
|
|
|
|
|
|
Erythropoietic/Hepatic
|
|
|
|
|
How will you clinically classify Porphyrias?
- Porphyria that produces skin manifestation without the presence of neurological symptoms are:
- Porphyria cutanea tarda.
- Congenital erythropoietic porphyria.
- Erythropoietic porphyria.
- Porphyria that is manifested by neurological symptoms (cutaneous symptoms are absent) are:
- Acute intermittent porphyria.
- Porphyria that has both cutaneous and neurological manifestations are:
- Hereditary coproporphyria.
- Variegate porphyria.
How will you classify Porphyrias according to symptoms?
- Neurologic only.
- Cutaneous only.
- Both neurologic and cutaneous types.
How is the excretion of Porphyrins?
- Aminolevulinic acid and porphobilinogens are excreted in the urine.
- Uroporphyrins are also excreted in the urine; a minimal amount is in the feces.
- Most coproporphyrins are eliminated in the feces, and a small amount is in the urine.
- Protoporphyrins are eliminated through bile; the average fecal content is 1 mg/day.
- Coproporphyrins’ urinary excretion increases in obstructive jaundice, liver diseases, lead poisoning, and hemolytic anemias.
| Disease | Substrate | Enzyme deficiency |
| Acute Intermittent Porphyria | Porphobilinogen | Hydroxymethylbilane synthase |
| Porphyria Cutanea Tarda | Uroporphyrinogen III | Uroporphyrinogen decarboxylase |
| Hereditary coproporphyria | Coproporphyrinogen III | Coproporphyrinogen Oxidase |
| Erythropoietic Protoporphyria | protoporphyrin | Ferrochelatase |
What are the signs and symptoms of Porphyrins?
- The following factors may initiate an acute attack:
- Some of the drugs.
- Smoking may initiate the attack.
- Use of alcohol.
- By some surgical procedures.
- Emotional upset.
- In females by the menstrual cycle.
- In females during pregnancy.
- Sometimes, an infection may give rise to an attack.
- The acute attack may start with anxiety, restlessness, and difficulty sleeping.
- The patient may develop a painful abdomen, and this may be very severe.
- There may be nausea and vomiting.
- The patient may develop constipation.
- There may be tachycardia and hypertension.
- Urine is dark or reddish.
- Rarely, there may be sudden death, which may be due to cardiac arrhythmias.
What are the normal values of Porphyria?
Source 1
Porphobilinogen
- Fresh urine or 24 hours sample = Negative
- Spectrophotometric method (24 hours of urine)
- <2.0 mg/L
- <3.4 mg/day
- ≤2.0 mg/day
- To convert into SI unit x 4.42 = µmol/L
Porphyrins
- Urine fresh random = Negative
- Total porphyrin (whole blood) = <60 µg/dL
Total porphyrins
- 20 to 320 nmol/L (urine)
Uroporphyrin fraction = <33 µg/24 hours urine
= 17 to 52 µg/24 hours urine
Coproporphyrins fraction = <183 µg/24 hours urine
= <294 µg/24 hours urine
= 52 to 163 µg/24 hours urine
Source 2
Urine 24 hours or fresh:
- Negative or trace.
- Total porphyrin:
- Male = 8 to 149 mcg/24 hours of the urine
- Female = 3 to 78 mcg/24 hours of the urine
- Uroporphyrin:
- Male = 4 to 46 mcg/24 hours of urine
- Female = 3 to 22 mcg/24 hours of the urine
- Coproporphyrin:
- Male = <96 mcg/24 hours of the urine
- Female = <60 mcg/24 hours of the urine
- Porphobilinogen = 0 to 2 mg /24 hours of the urine
- another source <1 mg/24 hours of the urine
- δ-Aminolevulinic acid = 1.5 to 7.5 mg/day of the urine
Source 4
- Porphobilinogen
- Random specimen = 0 to 2.0 mg/L
- 24-hour sample = 0 to 1.5 mg/24 hours
- Δ-aminolevulinic acid
- Random specimen = 0. to 4.5 mg/L
- 24-hour specimen = 1.5 to 7.5 mg/24 hours
| Test | µg/24 hours Urine | |
| Male | Female | |
| Random sample | Negative | Negative |
| Uroporphyrin | 8 to 44 | 4 to 22 |
| Coproporphyrin | 10 to 109 | 3 to 56 |
| Heptacarboxyporphyrin | 0 to 12 | 0 to 9 |
| Pentacarboxy porphyrin | 0 to 4 | o to 3 |
| Hexacarboxyporphyrin | 0 to 5 | 0 to 5 |
Diagnosis of Porphyrins:
- A urine sample is not as accurate as the plasma concentration.
- Urine is suitable as a screening test for porphyria.
Treatment of Porphyrins:
- Treat to relieve the symptoms.
- Drug-like heme arginate is given to stop the process.
Questions and answers:
Question 1: What is the mechanism of toxic injury in porphyrias?
Question 2: How you will diagnose porphyrias?

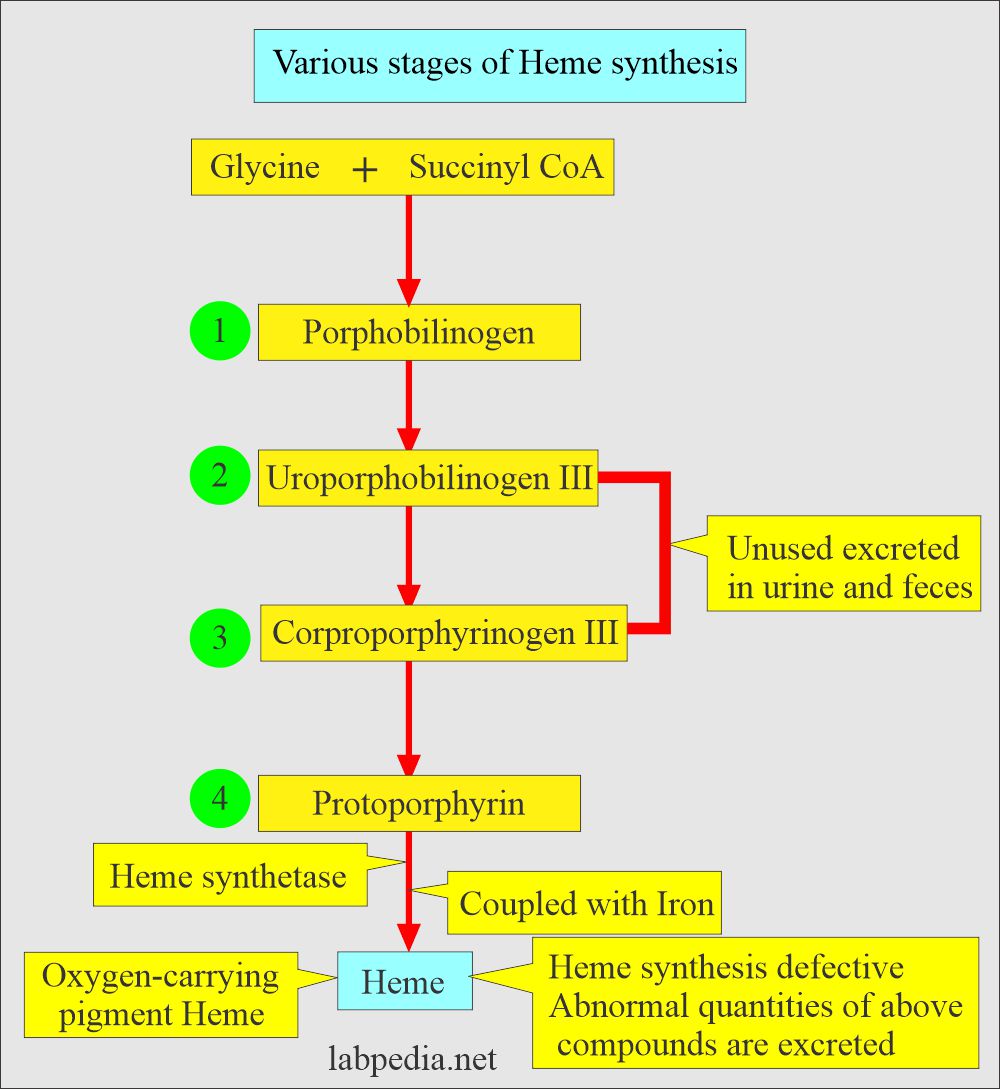
Conversion of protoporphyrinogen lll to protoheme occurs in the mitochondria according to Tietz