Polycythemia (Erythrocytosis), Polycythemia Rubra Vera, and Secondary Polycythemia
Polycythemia (Erythrocytosis)
What sample is needed to study the cause of Polycythemia?
- EDTA blood sample is required.
How will you define Polycythemia?
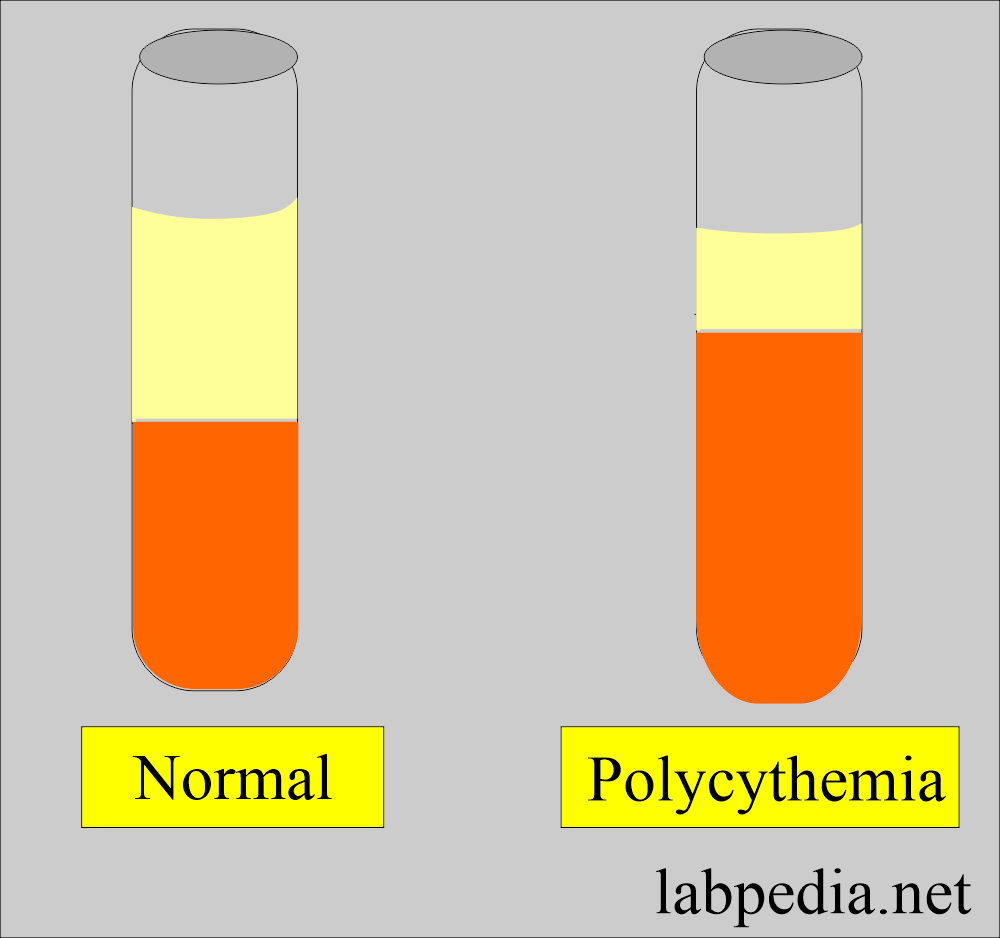
- Polycythemia is an increase in the total blood RBCs, more than the normal upper limit.
- There is increased hemoglobin and hematocrit.
- This is an uncontrolled proliferation of red blood cells.
- There is increased hemoglobin concentration above the normal upper limit.
What are the Criteria for labeling polycythemia?
- RBCs = count increased, more than the normal upper limit.
- PCV = Increased.
- Hemoglobin = Increased >18 g/dL (180 g/L).
- Male = 18 g/dL (170 g/L)
- Female = 16 g/dL (160 g/L).
- Hematocrit = Increased.
- Male = >55%
- Female = >50%
How would you classify Polycythemia?
- Types of Polycythemia. There are three types :
- Primary polycythemia (also known as polycythemia rubra vera).
- Secondary polycythemia.
- Relative polycythemia.
- There is pseudopolycythemia, where red cell volume is normal, but the plasma volume is reduced.
| Parameters | Normal value | Relative Polycythemia | Primary/secondary polycythemia |
|
|
|
|
|
|
|
|
What is the importance of Polycythemia?
- There is hyperviscosity.
- In primary polycythemia, there is an uncontrolled clonal proliferation of stem cells.
- A chromosomal abnormality of the deletion of 9p or 20q was found in the minority of the cases.
Polycythemia Rubra Vera (primary)
- Polycythemia vera is also called polycythemia rubra vera.
What are the important facts about Polycythemia vera?
- This is a bone marrow disorder where the bone marrow produces an uncontrolled RBC proliferation.
- This is basically a myeloproliferative disorder.
- This is a stem cell disorder.
- Erythrocytosis is not dependent on erythropoietin.
What is the onset of polycythemia Rubra Vera?
- The median age at diagnosis is 60 years. It occurs between 40 to 70m years of age.
- This is more common in men than in women.
What is the presentation of polycythemia rubra vera?
- This is a chronic disease; many patients die from thrombosis or cardiac arrest.
- Polycythemia vera may also produce too many other types of blood cells, such as white blood cells and platelets.
- Polycythemia vera is also called primary polycythemia.
- It is rare and usually develops slowly.
- Polycythemia vera is often found during a blood test for some other reason.
- These patients who survive long may develop myelofibrosis or myeloid leukemia.
What are the lab findings of Polycythemia Rubra Vera?
- Laboratory findings are:
- Increased RBC count, Hb, and Hct.
- Normal MCV and MCH.
- Increased WBCs and platelets.
- Bone marrow shows panhyperplasia.
What are the causes of polycythemia (Rubra) vera?
- Unknown.
- Bone marrow abnormality
- 95 % of the cases have a genetic abnormality.
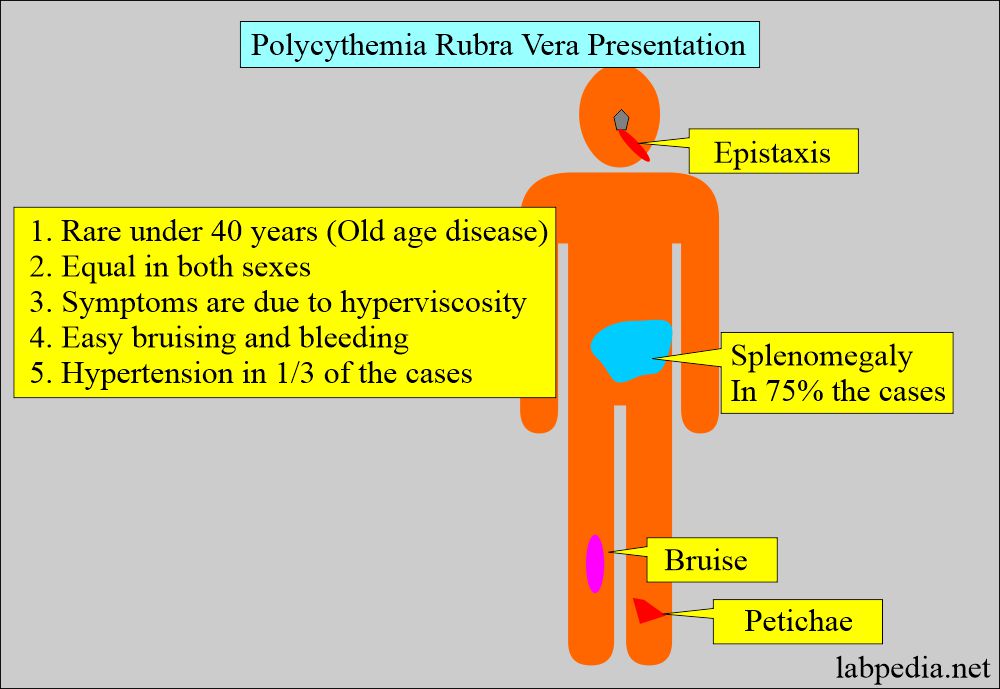
What are the signs and Symptoms of Polycythemia (Rubra) vera?
- This is often found incidentally when raised hemoglobin and RBC counts are found.
- This is the disease of old age with equal sex distribution.
- Rarely seen under the age of 40 years
- The symptoms are due to the following:
- Hyperviscosity.
- Hypervolemia.
- Hypermetabolism.
- There is a history of epistaxis and bleeding from the GI tract.
- There is easy bruising and bleeding.
- The patient may have neurologic symptoms like vertigo, tinnitus, headache, and eye problems, particularly after a hot bath, and may become a severe problem.
- Hypertension is seen in 1/3 of the patients.
- There may be generalized pruritus.
- The spleen may be palpable in 75% of the cases (60% to 90%). It is more common in patients with leucocytosis.
- Hepatomegaly is less common but seen in 40% to 50% of the cases.
- Gout may be seen due to a raised level of uric acid.
- Peptic ulceration is seen in 5% to 10% of the patients.
- In these patients, there is a tendency to develop peptic ulcer and gout.
- There is a tendency to develop venous thrombosis.
How will you diagnose Polycythemia (Rubra) Vera?
- Hemoglobin is raised.
- Hct may be >60%.
- Normal MCV and MCH.
- Total red cell mass:
- Male >35 mL/Kg
- Female = >32 ml/Kg.
- Arterial oxygenation is >92%.
- There is an increased number of WBCs and platelets. You may see a shift to the left.
- A raised platelet count is seen in half of the patients.
- Increased leucocytosis is seen in more than half of the patients, and even may see increased basophils.
- Increased neutrophil alkaline phosphatase score (NAP).
- Bone marrow is hypercellular with prominent megakaryocytes.
- The serum erythropoietin level is usually low.
- Blood viscosity is increased.
- Serum LDH level is normal,
- Serum uric acid is increased in up to 40% of the cases due to the turnover of RBCs.
- There is splenomegaly.
- The JAK2 mutation is seen in granulocytes in almost 100% of the cases.
- There is increased serum vitamin B12 and B12-binding capacity.
- Typical parameters for the diagnosis are:
- Increased RBC mass (Increased RBC and hematocrit).
- Leucocytosis and Thrombocytosis.
- Splenomegaly.
How will you treat polycythemia Rubra Ver?
- Venesection to keep hematocrit low.
- Cytotoxic myelosuppression by chemotherapy. Phosphorus-32 therapy is used in older patients.
- Interferon (α-interferon) suppresses the bone marrow.
- Aspirin prevents thrombotic complications.
What will the prognosis be for polycythemia Rubra Vera?
- Mostly, the prognosis is good, and the median survival is 10 to 16 years.
- The major complications are thrombosis and hemorrhage.
- It may progress to myelofibrosis with myeloid metaplasia in about 20% to 25%.
- 5% to 6% of the cases end up in acute leukemia.
Secondary polycythemia
- Secondary polycythemia is true polycythemia caused by either natural or artificial increases in erythropoietin production, leading to increased RBC production.
- RBCs count maybe 6 to 8 million (occasionally 9 million cmm).
- Secondary polycythemia resolves when the underlying cause is treated.
What are the causes of Causes of secondary polycythemia?
- Or physiological polycythemia may be caused by:
- High Altitude (altitude sickness).
- Hypoxic disease.e.g., cyanotic heart and hypoxic lung disease (COPD). And chronic obstructive sleep apnea.
- Smoker’s polycythemia is due to the formation of the carboxyhemoglobin.
- Idiopathic or Iatrogenic can be induced directly by phlebotomy, which can concentrate the erythrocytes.
- Genetic abnormalities in hemoglobin oxygen release.
- Renal diseases like cystic disease and hydronephrosis.
- Less common causes are:
- Renal-cell carcinoma (1% to 5%).
- Liver tumors (Hepatoma = 3% to 12%).
- Pheochromocytoma.
- Adrenal adenoma with Cushing’s syndrome.
- Anabolic steroids use (athletes abuse steroids).
- Testosterone replacement for hypogonadism.
- People who take erythropoietin may develop secondary polycythemia.
How will you diagnose Secondary polycythemia?
- Increased RBC count.
- Increased hemoglobin.
- Increased hematocrit.
- Normal MCV and MCH.
- White cells and platelets are normal.
Relative polycythemia (Pseudopolycythemia)
How will you define Relative polycythemia?
- A total normal RBC mass falsely appears to have increased due to a decrease in the plasma volume.
- Dehydration is the most common cause.
What are the causes of Relative Polycythemia?
- It is caused by:
- Stress,
- Smoking.
- Dehydration in case of water deprivation and vomiting.
- Plasma loss in burn and enteropathy.
What are the characteristics of Relative Polycythemia?
- This is characterized by the following:
- Raised hemoglobin.
- Normal TLC.
- Normal platelets.
- Normal red cell mass.
- Decreased plasma volume.
What are the laboratory findings of Relative Polycythemia?
- Laboratory findings are:
- Increased RBC count, Hb, Hct,
- Normal WBCs and platelets.
- Relative polycythemia is seen in decreased plasma volume and may be seen in dehydration or hemoconcentration.
How will you treat the Polycythemia?
- The treatment of the choice is phlebotomy.
- Donate one point of blood until the Hct is <45%.
- The patient should be given a low-iron diet.
- Chemotherapy like myelosuppressive drugs may be given.
How will you summarize various Polycythemias?
| Clinical and laboratory findings | Relative polycythemia | Secondary polycythemia | Primary polycythemia Rubra |
| 1. Red cell mass | DEcreased/Normal | increased | Increased |
| 2. Erythropoietin | Normal | Increased (rarely normal) | Decreased (rarely normal) |
| 3. White blood cells(shift to left) | Normal | Normal | Increased in 80% of the cases |
| 4. Platelets count | Normal | Normal | Increased by 50% of the cases |
| 5. Nucleated RBCs | Absent | Absent | Usually present |
| 6. Bone marrow | Normal | increased erythropoiesis |
|
| 7. Leucocyte alkaline phosphatase score | Normal | Normal | Increased in 70% of the cases |
| 8. Serum vitamin B12 | Normal | Normal | Increased in 75% of the cases |
| 9. Splenomegaly | Absent | Absent | Present in 75% of the cases |
| 10. Hepatomegaly | Absent | Absent | Present in 35% of the cases |
| 11. Heart or lung disease | Absent | Present | Absent |
| 12. Cyanosis | May be present | Present | Absent |
questions and answers:
Question 1: Is there any association of heart/lung disease with polycythemia vera?
Question 2: Do you see cyanosis in polycythemia vera?