Platelets – Part 1 – Idiopathic Thrombocytopenic Purpura (ITP)
Idiopathic Thrombocytopenic Purpura (ITP)
What sample is needed for Idiopathic thrombocytopenic Purpura (ITP) diagnosis?
- Plasma is needed.
- Plasma is separated and frozen in a plastic tube.
- Or collect the blood in acid citrate dextrose (ACD) solution.
- Apply the pressure or do a pressure dressing to stop the bleeding.
What are the precautions for Idiopathic thrombocytopenic Purpura (ITP)?
- Apply the pressure to the site of the blood sample.
- If bleeding occurs from the site, ask the patient to apply pressure.
What are the Indications for Idiopathic thrombocytopenic Purpura (ITP)?
- This test is indicated when there are low platelet counts.
- In the case of unresponsiveness to the treatment of low platelets,
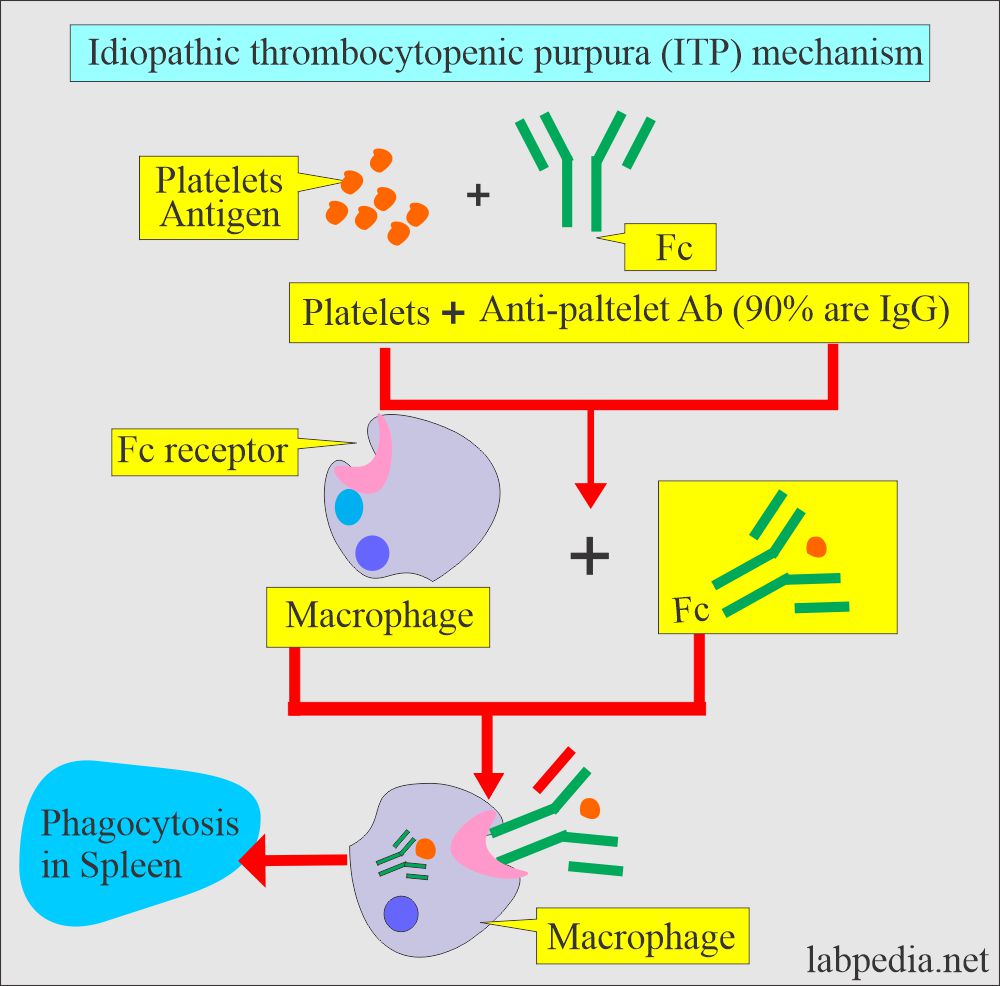
How will you discuss the Pathophysiology of Idiopathic thrombocytopenic Purpura (ITP)?
- Platelets are mainly involved in the clotting mechanism.
- Antiplatelet antibodies are found in patients with idiopathic thrombocytopenic purpura (ITP), where the antigen is platelets.
- Autoimmune (idiopathic) thrombocytopenic purpura may be divided into:
- Acute.
- Chronic.
- There is the immune-mediated destruction of the platelets.
- The antibodies are usually directed against the HLA antigen on the surface of platelets, or maybe platelet-specific antigens (PLA1 and PLA2).
What is the differential diagnosis of acute and chronic ITP?
| Clinical parameter | Acute immune thrombocytopenia | Chronic Immune thrombocytopenia |
| Onset of ITP |
|
Mostly insidious |
| Age of onset |
|
|
| Complete blood picture |
|
|
| Plate count |
|
|
| Megakaryocytes | These are increased | There is an increase in the number and volume |
| Platelets-antibodies | Plate-let antibodies are found in 80% to 90% of the cases. | Plate-let antibodies are found in 80% to 90% of the cases. |
| Clinical S/S | There is purpura or other hemorrhagic manifestation | There is purpura or other hemorrhagic manifestation |
| Enlarged spleen | It is against the ITP diagnosis | It is against the ITP diagnosis |
| After splenectomy | 2/3 of the children develop normal platelet count | 85% of the adults develop normal platelet count |
What are the types of thrombocytopenia?
Immunologic thrombocytopenia:
- Immunologic thrombocytopenia may be due to the following causes:
1. Idiopathic thrombocytopenic purpura (ITP):
- This is an autoimmune phenomenon; platelets are destroyed in the spleen or reticuloendothelial system.
- Chronic idiopathic thrombocytopenia:
- This is more common in females aged 15 to 50 years.
- This is the most common cause without anemia and leucopenia.
- This is also associated with other diseases like systemic lupus erythematosus (SLE), HIV infection, chronic lymphocytic leukemia, Hodgkin’s disease, or autoimmune hemolytic anemia.
- Platelets associated with antibodies (Immunoglobulin IGg) are found in 90% of the cases.
- Platelet transfusion is indicated:
- When platelets count is <5,000/cmm, even these patients are asymptomatic.
- Bleeding after splenectomy.
- If there is severe mucosal bleeding at any platelet counts.
2. Post-transfusion purpura:
- This rare phenomenon is seen after a blood transfusion and may be seen within a few hours to a few days.
- It is usually seen around the 10th day of the transfusion.
- This will develop due to antibodies in the recipient developing against platelet antigen-1a (HPA-1a) absent from the patient’s own platelets on transfused platelets.
- Treatment is by giving intravenous immunoglobulin, plasma exchange, or corticosteroids.
3. Maternal-fetal platelet incompatibility:
- This usually occurs when the fetus has PLA1, and the mother lacks this antigen. Mothers develop antibodies that can cross the placental barrier and produce neonatal thrombocytopenia.
4. Drug-induced thrombocytopenia.
- This is due to the hypersensitivity reaction to drugs. e.g., Cimetidine, analgesics like salicylate and acetaminophen, antibiotics (cephalosporin, penicillin, sulphonamide), quinidine drugs, oral hypoglycemic agents, heavy metal ( gold, organic arsenical), diuretics (chlorothiazide), digoxin, heparin, and propylthiouracil.
What are other classifications of thrombocytopenia?
Increased platelets destruction:
- Primary immune mechanism:
- Idiopathic thrombocytopenic purpura (ITP).
- Post transfusional purpura.
- Neonatal isoimmune purpura.
- Drug-induced thrombocytopenia.
- Secondary immune mechanism:
- Lymphoproliferative disorder.
- Autoimmune disease SLE.
- Viral infections like infectious mononucleosis, HIV, and measles.
- Hemolytic uremic syndrome.
- Disseminated intravascular coagulopathy (DIC).
- Microangiopathic thrombocytopenia.
- Pregnancy-associated thrombocytopenia.
Abnormal platelet destruction:
- Splenomegaly leads to hypersplenism.
- Hemangiomas.
Decreased production of the platelets:
- Lymphomas.
- Leukemias.
- Metastatic carcinoma infiltration of the bone marrow.
- Myelofibrosis.
- Aplastic anemia.
- Pernicious anemia.
- Folic acid deficiency.
What are the symptoms of low platelets (Thrombocytopenia)?
- If there is a bruise or bleeding, it will take longer to stop.
- Skin bruises easily.
- In the female, there is heavy bleeding.
- There are frequent nosebleeds.
What are the signs and symptoms of Idiopathic thrombocytopenic purpura (ITP)?
- In the beginning, there are nonspecific symptoms.
- It may develop ITP within 1 to 3 weeks of the viral infection in young children.
- The onset of symptoms is usually abrupt and usually counts as <20,000 /cmm.
- The disease is usually self-limiting, and spontaneous remission with or without therapy occurs in most cases.
- In adults, this is seen between the ages of 20 to 50 years and is more common in females.
- There is no recent history of infection or drug therapy.
- Typically platelets <30,000/cmm, the patient may have a bleeding tendency.
- Typically, patients will have mucosal bleeding.
- The primary hemostatic defect is menorrhagia, epistaxis, bruises, or petechiae.
What are the signs and symptoms of Thrombotic thrombocytopenic purpura (TTP)?
- This rare and often fatal syndrome is associated with low platelet count (thrombocytopenia).
- Then, patients develop weakness, malaise, fatigue, and fever.
- The patient may develop abdominal pain.
- The patient may have abdominal pain, pancreatitis, and gastrointestinal bleeding.
- These patients may have neurologic and renal dysfunction.
- There may be a mild headache; in some cases, patients may develop coma and seizures.
- S/S severity is variable.
- Fever is usually <38 °C.
- The patient may develop proteinuria or hematuria, and these signs are mild (Hemolytic uremic syndrome).
What are the possible Complications of Idiopathic thrombocytopenic Purpura (ITP)?
- There is the possibility of bleeding.
- There may be a bruise formation.
- There is the possibility of infection.
- Some patients may feel dizziness.
The normal level of platelets
Platelets
| cmm | x109 / L (SI unit) | |
| Adult | 15,000 to 400,000 | 150 to 400 |
| Premature infants | 100,000 to 300,000 | 100 to 300 |
| Newborn | 150,000 to 300,000 | 150 to 300 |
| Infants | 200,000 to 475,000 | 200 to 475 |
| Children | 150,000 to 400,000 | 150 to 400 |
- Platelet antibody = Negative
What are the causes of Increased levels of Antibodies?
- Immunologic thrombocytopenic purpura( ITP)
- Neonatal thrombocytopenia.
- Posttransfusion purpura.
- Drug-induced thrombocytopenia.
- Systemic lupus erythematosus.
How will you treat Idiopathic thrombocytopenic Purpura (ITP)?
- The count above 50,000/cmm does not require treatment.
- Steroids (corticosteroids) are given in high doses.
- 80% of the patients respond and go into remission.
- Prednisolone 1 mg/kg/day is the initial dose in the adult.
- The dose is gradually reduced to lower doses after 10 to 14 days.
- Splenectomy is the second choice.
- This is advised in patients with a count <30,000/cmm after the steroids for three months.
- Or in patients on high doses of steroids to maintain a count above 30,000/cmm.
- Immunoglobulins are given intravenously in high doses, and there is a rapid increase in the platelet count.
- 400 mg/kg/day for 5 days or 1 gram/kg/day for 2 days.
- Immunosuppressant drugs like vincristine, cyclophosphamide, azathioprine, or cyclosporin alone or in combination.
- Platelets transfusion.
- Stem cell transplantation can be tried.
- 80% of the patients respond and go into remission.
Critical value = <50,000/cmm or >one million /cmm.
Questions and answers:
Question 1: At what level of platelets bleeding may occur?
Question 2: What is the complication of low platelets in young females?