August 7, 2024
Neonatal Jaundice
What sample is needed for Neonatal Jaundice?
- Can get blood from the finger or heel prick.
- If possible, take venous blood.
How will you classify Neonatal jaundice?
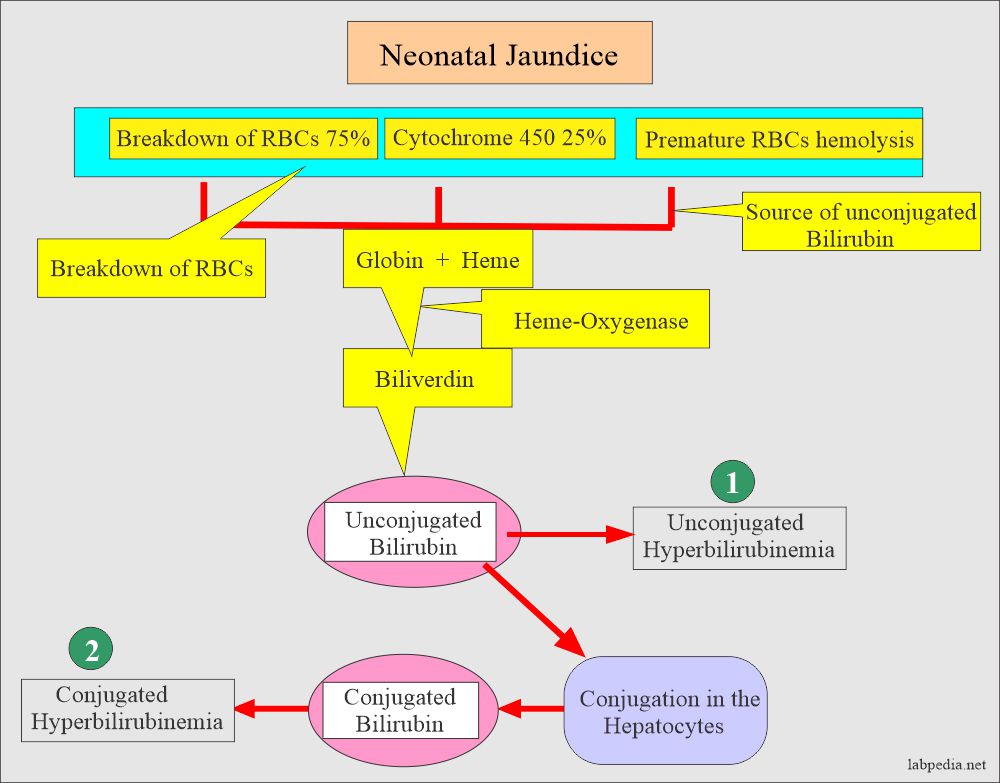
Neonatal jaundice can be classified as:
- Unconjugated hyperbilirubinemia.
- There is a risk of the development of kernicterus.
- Conjugated hyperbilirubinemia.
- This type of jaundice is characterized by an increased conjugated bilirubin >1.5 mg/dL (24 µmol/L).
- The most important cause is idiopathic neonatal hepatitis and biliary atresia.
- This type may be seen in newborns as a complication of parenteral nutrition.
- Neonatal jaundice can also be classified as:
- Physiologic jaundice.
- Pathological jaundice.
How will you discuss the Physiologic jaundice of the newborn?
- Benign Physiologic jaundice of the newborn appears in the first 2 to 3 days (first few days of birth).
- Rarely does bilirubin rise to 5 mg/dL/day.
- The peak reaches a peak level within the first 4 to 5 days.
- Bilirubin level remains elevated for <2 weeks.
- Rarely it exceeds >20 mg/dL.
- Factors contributing to physiologic jaundice are:
- The bilirubin level increased because of the short life of RBCs.
- There is a decreased level of glucuronyltransferase enzyme in the first few days of birth.
- There is the exposure of breastfeeding infants to inhibitors of bilirubin conjugation present in breast milk.
- Differentiation from pathologic jaundice?
- Hemolytic disease leading to jaundice:
- Rh-incompatibility occurs when the fetus is Rh-positive.
- Infants become jaundiced with unconjugated bilirubin in the first or second days of life.
- These babies may develop kernicterus.
- Breast milk hyperbilirubinemia:
- It is seen in 30% of breastfed newborns.
- The exact cause is unknown.
- This condition lasts for a few weeks.
- It can be treated by discontinuing breastfeeding.
How will you discuss the Pathological neonatal jaundice?
- This jaundice in newborns may appear in the first 24 hours.
- It keeps on rising in the first week of age.
- It may persist for more than 10 days.
- Total bilirubin may be >12 mg/dL.
- The rise is quick, with a single-day increase of >5 mg/dL/day.
- Conjugated (direct bilirubin) will be >2 mg/dL.
- Conjugated bilirubin levels up to 2 mg/dL are found in infants by one month, and this will remain through adulthood.
- This is seen in newborns whose livers are immature and lack sufficient conjugating enzymes. This leads to an increased amount of unconjugated bilirubin.
- This unconjugated bilirubin can cross the blood-brain barrier and give rise to encephalopathy (Kernicterus).
- Bilirubin above 15 mg /dl in the newborn needs immediate treatment.
- This is treated by exchange of blood transfusion or light phototherapy.
What is the Differential diagnosis of neonatal jaundice?
| Clinical conditions | Conjugated bilirubinemia | Unconjugated bilirubinemia |
|
|
|
|
|
|
|
Metabolic disorders:
|
Hemolytic diseases of the newborn:
|
|
|
Increased enterohepatic circulation:
|
|
Hereditary causes:
|
Hereditary causes:
|
|
|
|
How will you treat neonatal jaundice?
- Newborn babies are exposed to phototherapy.
- The baby is exposed to 450 nm, changing bilirubin into water-soluble and excreted into the bile.
- An exchange blood transfusion is needed when the bilirubin level rises above 15 mg/dL.
What will the Bilirubin levels be that may require treatment in a full-term, healthy baby?
| Age of the infants | Bilirubin level | Treatment |
| 24 hours or younger infants | >10 mg/dL (>170 mmol/L) | Needed |
| 25 to 48 hours of infants | >15 mg/dL (>255 mmol/L) | Needed |
| 49 to 72 hours of infants | >18 mg/dL (>305 mmol/L) | Needed |
| Older than 72 hours of infants | >20 mg/dL (>340 mmol/L) | Needed |
What will the panic value of bilirubin be in neonates?
- >15 mg/dL (>250 µmol/L). It may damage the brain and leads to mental retardation in infants.
Questions and answers:
Q 1: What is the bilirubin level for blood exchange in the newborn?
Q 2: How to treat physiologic jaundice.

thanks for the important information
Thanks.