Maternal Screening:- Part 1 – Maternal Triple or Quadruple screening for Genetic abnormality, Inhibin A and B
Maternal Screening
What sample is needed for Maternal Screening?
- These tests are done on the patient’s serum.
- A urine sample may also be needed.
- These tests are done during the 14th to 20th weeks of gestation.
- Supplement these tests with ultrasound.
- Ultrasound helps to establish the exact age of the fetus.
- For confirmation:
- Chorionic villus samples may be taken in early pregnancy.
- Amniocentesis may be done if needed in mid-pregnancy.
- First-trimester screening relieves a mother’s anxiety earlier than doing the test in the 2nd trimester.
What are the precautions for Maternal Screening?
- The tripple screening test should be done between 15 to 20 weeks of gestation.
- 16 to 18 weeks is a more accurate test.
- These screening tests are just warning of fetal abnormality and are not confirmatory.
What are the Indications for Maternal (prenatal) Screening?
- These tests diagnose early pregnancy abnormalities like:
- A potential birth defect like neural tube defects or abdominal wall defects.
- Chromosomal or genetic abnormalities.
- These are indicated in women over the age of 35 years.
- Abnormal maternal alpha-fetoprotein.
- Abnormal HCG level.
- Abnormal unconjugated estriol level.
- These are also indicated in women who have previous abnormal infants with birth defects.
- To diagnose trisomy 21 (Down’s syndrome).
- To diagnose trisomy 18.
- Ethenic risk factors like sickle cell anemia, Tay-Sachs disease, α, and β thalassemia.
- In the case of rubella, toxoplasmosis, or CMV infection.
- If the mother suffers from diabetes mellitus and phenylketonuria.
- If pregnant women are exposed to teratogenic material like radiation, chemotherapy, alcohol, anticonvulsants, and lithium.
- In the case of a previous pregnancy with a chromosomal abnormality.
- In the case of inherited disorders like cystic fibrosis, sex-linked recessive disorders, and metabolic disorders.
What is the significance of Prenatal screening?
- The fetus produces AFP protein.
- HCG is the hormone produced by the placenta.
- Estriol is an estrogen hormone produced by the fetus and the placenta.
- With the help of these tests, one can diagnose:
- Neural tube defects like myelomeningocele or spina bifida.
- Abdominal wall defects like omphalocele or gastroschisis.
- The incidence of fetal abnormalities is related to the age of women.
- Down’s Syndrome chances increase with increasing age are:
- At the age of 25 years = 1:1300.
- At the age of 35 years = 1: 365.
- At the age of 45 years = 1:30.
- In the USA, this screening is now offered to pregnant women in the second trimester of pregnancy.
- The screening tests are not diagnostic.
- In case of abnormality in screening tests, then confirmatory tests are advised.
What are the confirmatory tests for finding fetal abnormalities?
- Chorionic villus sampling in the first trimester.
- Amniocentesis in the mid-pregnancy.
- In the USA, most women over the age of 35 years have chorionic villus sampling or amniocentesis.
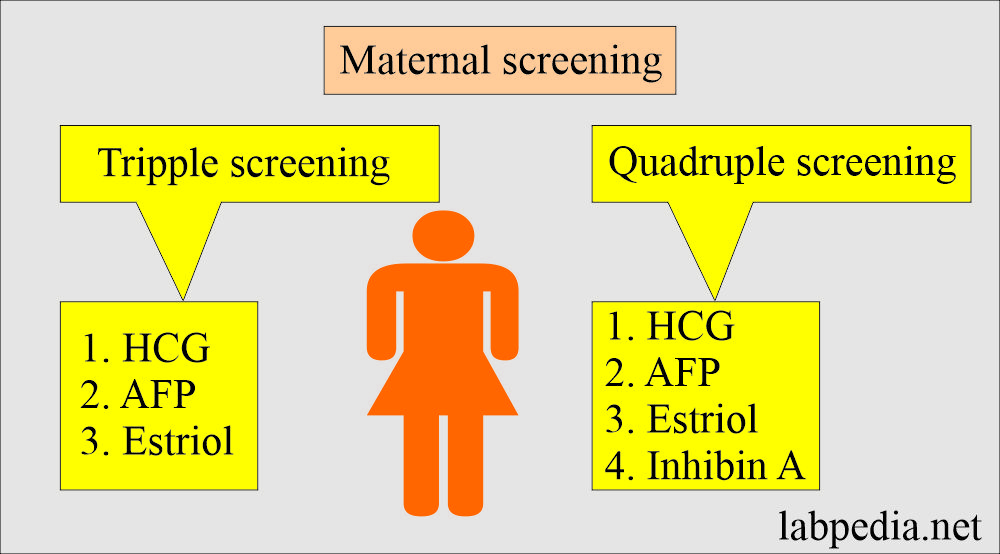
What screening tests are available to find fetal abnormalities?
- Double screening test: This consists of two markers:
- HCG.
- AFP
- Triple screening test: This consists of three markers:
- HCG (produced by the placenta).
- AFP (produced by the yolk sac and liver).
- Estriol (produced by the placenta).
- Quadruple screening test: This consists of four markers.
- HCG.
- AFP.
- Estriol.
- Inhibin A.
- Triple screening is more popular because it can diagnose trisomy 21 (Down’s syndrome) in 50% to 80% of the cases.
- If done alone, AFP will detect only 30% of the cases with trisomy 21.
- Detecting the abnormality earlier prepares the family for the coming abnormal baby, or they can decide to terminate the pregnancy.
How would you define Inhibin A and B?
Definition of Inhibin A and B:
- It is a polypeptide hormone and belongs to the transforming growth factor family.
- Inhibin is secreted by granulosa cells of the ovary and the Sertoli cells of the testes.
- It inhibits the pituitary production of FSH.
- The placenta secretes it during pregnancy.
How will you define Inhibin A?
- The corpus luteum produces inhibin A.
- This is normally secreted by the ovary granulosa cells and inhibits FSH production from the pituitary gland.
- It is a glycoprotein of placental origin in pregnancy, like HCG.
- It is important in the control of fetal growth.
- Its level is 2 times higher in trisomy 21 than in a normal pregnancy.
- Its level is lower in normal pregnancy as compared to women with spontaneous abortion.
What is the role of Inhibin A in females?
- It is undetectable before puberty.
- There is a low level in the postmenopausal period due to absent follicular secretions.
- During pregnancy, it is produced by the placenta.
- Inhibon A peaks at 8 to 10 weeks and then declines until 20 weeks. After that, it increases gradually until the term.
What do you know about Pregnancy-associated plasma protein-A (PAPP-A)?
How will you define pregnancy-associated plasma protein-A?
- PAPP-A is a zinc-binding matrix metallo-proteinase produced by syncytiotrophoblastic cells.
- This is produced by the placenta and the endometrium.
- Women with low PAPP-A at 8 to 14 weeks have the chance for:
- Intrauterine growth restriction.
- Trisomy 21.
- Premature labor.
- Pre-eclampsia.
- Stillbirth.
- In trisomy 21, the level is half of the normal level.
- A low level in the third trimester is associated with severe fetal abnormalities, fetal death, and intrauterine growth restriction.
Where would you see a positive screening test?
- Trisomy 18.
- Trisomy 21.
- Neural tube defect.
- Abdominal wall defects.
Questions and answers:
Question 1: What is the site of formation of PAPP-A?
Question 2: What is the source of inhibin A?