During Blood Collection, Management of Anaphylactic reaction (Type 1-Hypersensitivity)
During Blood Collection, Management of Anaphylactic reaction
When can you see a type 1 reaction?
- An anaphylactic reaction may be seen in a patient during or after taking the blood sample.
- This is a typed I Hypersensitivity reaction or Anaphylactic reaction.
- So, every technician should know how to deal with such a situation.
What are the causes of Anaphylactic reaction:?
- An anaphylactic reaction may be due to:
- Penicillin.
- Stings.
- Food like nuts, eggs, milk, and fish.
What are the signs and symptoms of Type-I hypersensitivity reaction?
- The type-1 reaction may be:
- The localized reaction is in the form of urticaria and angioedema.
- These reactions are severe but not fatal.
- Physical allergies like heat, cold, sunlight, and pressure may exist.
- The generalized reaction is also called an anaphylactic reaction.
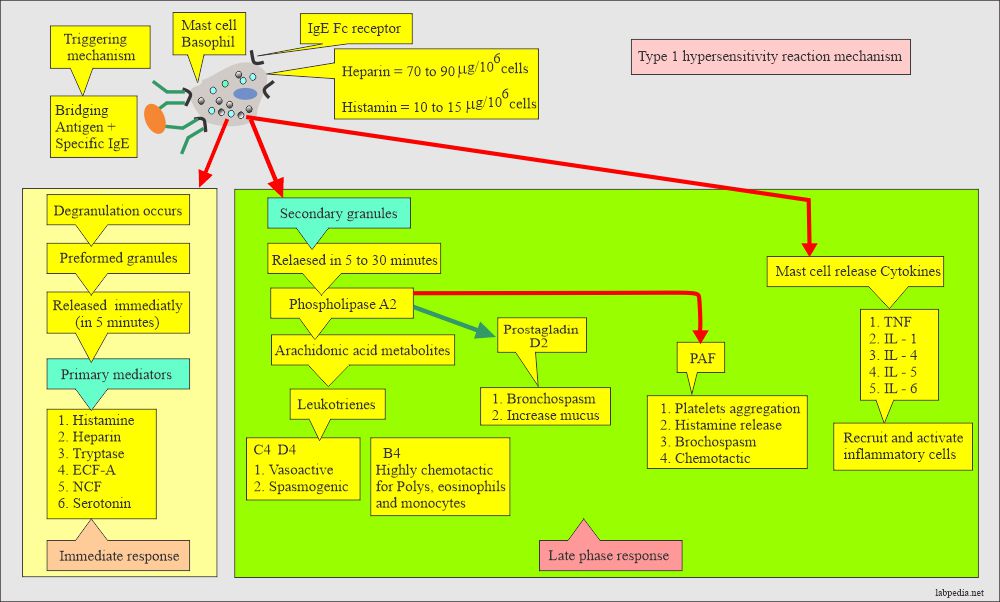
- These are due to the release of primary and secondary mediators.
- The affected organs are the cardiovascular system, respiratory, and gastrointestinal systems.
- There may be involvement of the skin.
How will you describe the pathophysiology of an anaphylactic reaction?
- The antigen may be:
- Atopic allergies.
- Drugs like penicillin.
- Insect Stings.
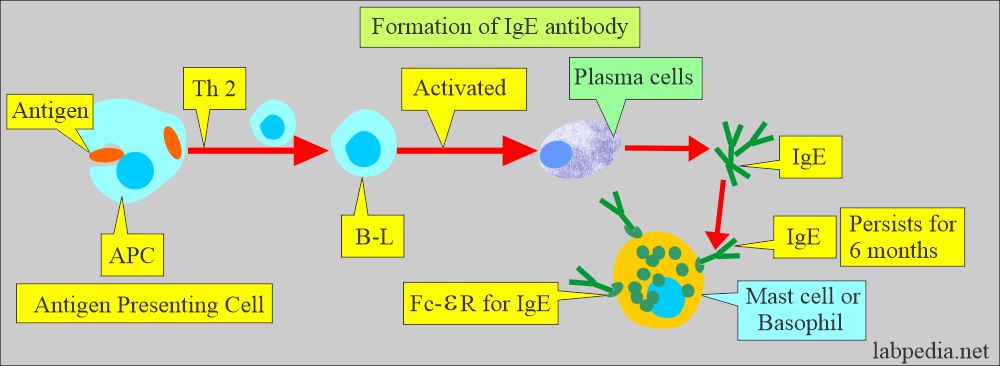
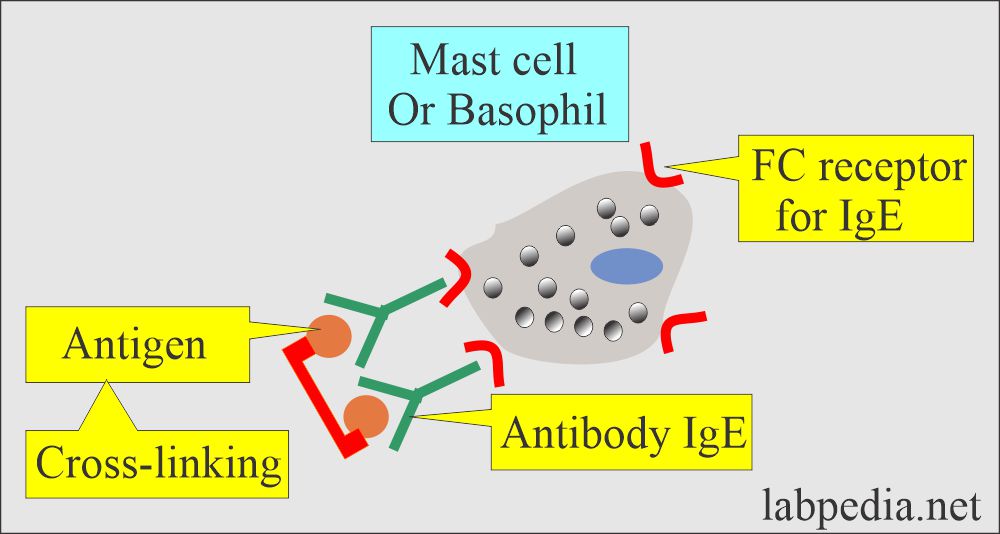
- The antibody is mainly IgE.
- Rarely is this reaction seen by IgG.
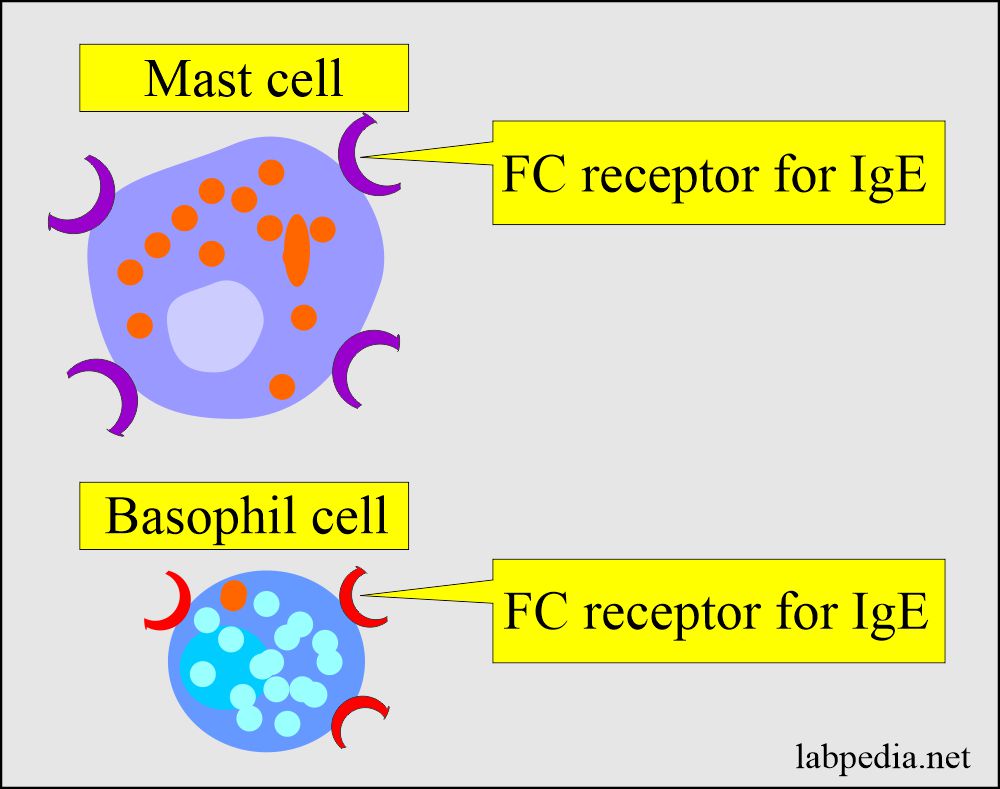
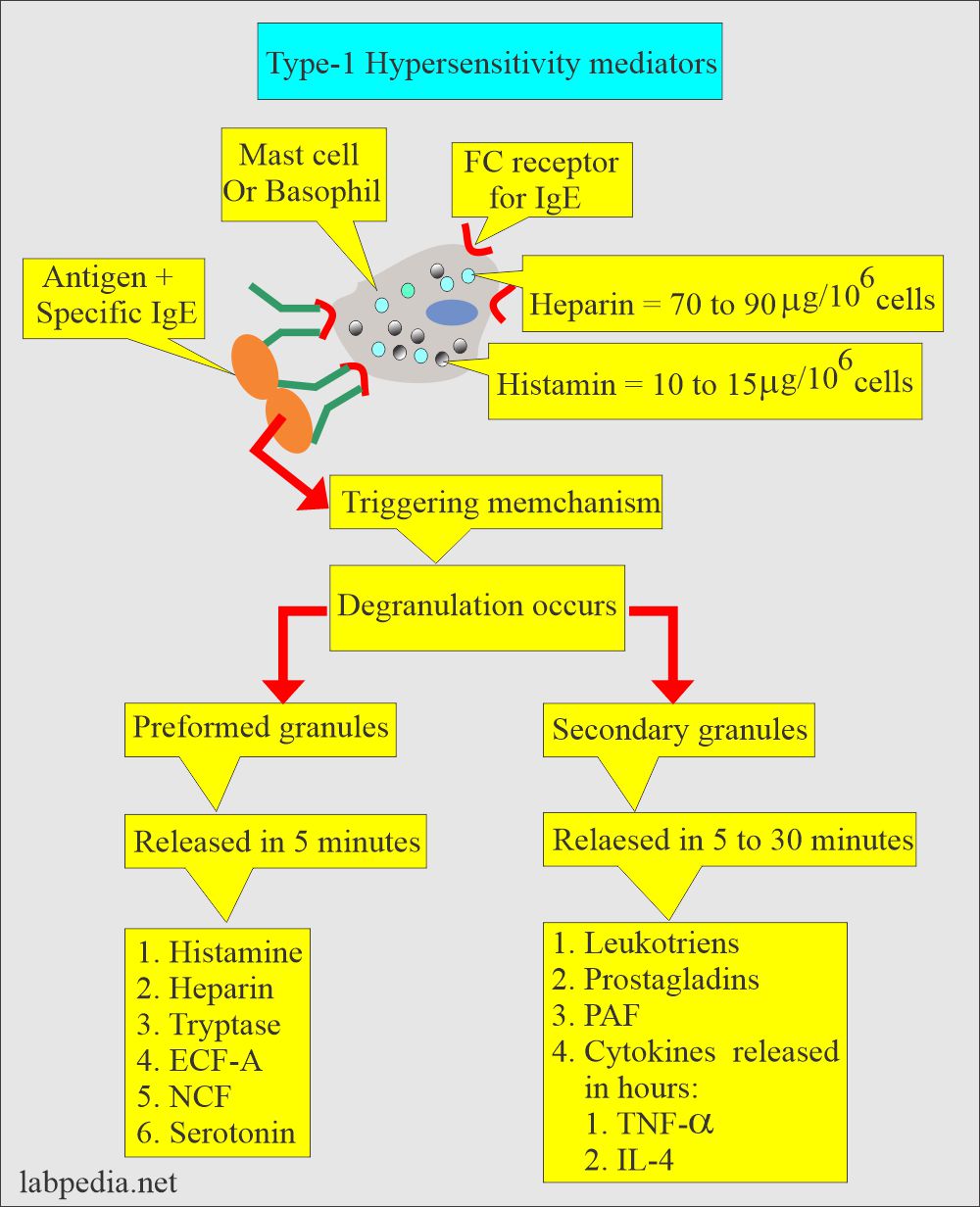
- The immune cells are mast cells and basophils.
- These cells have receptors for the Fc portion of IgE.
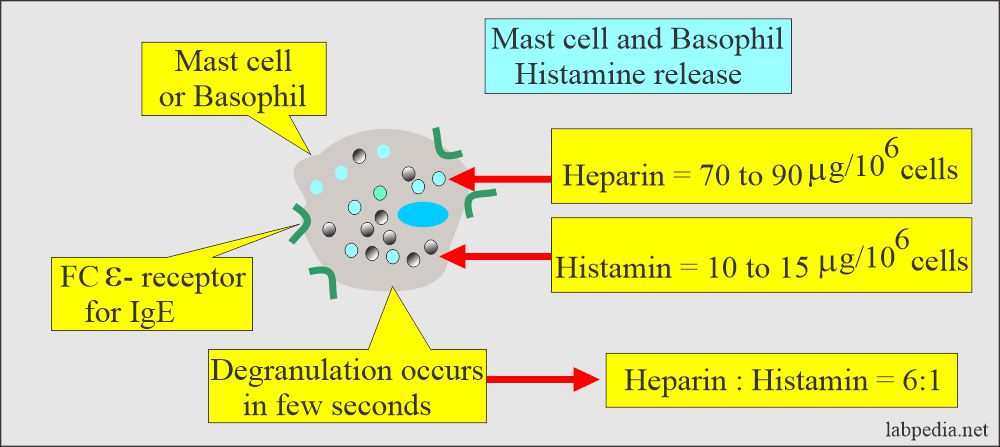
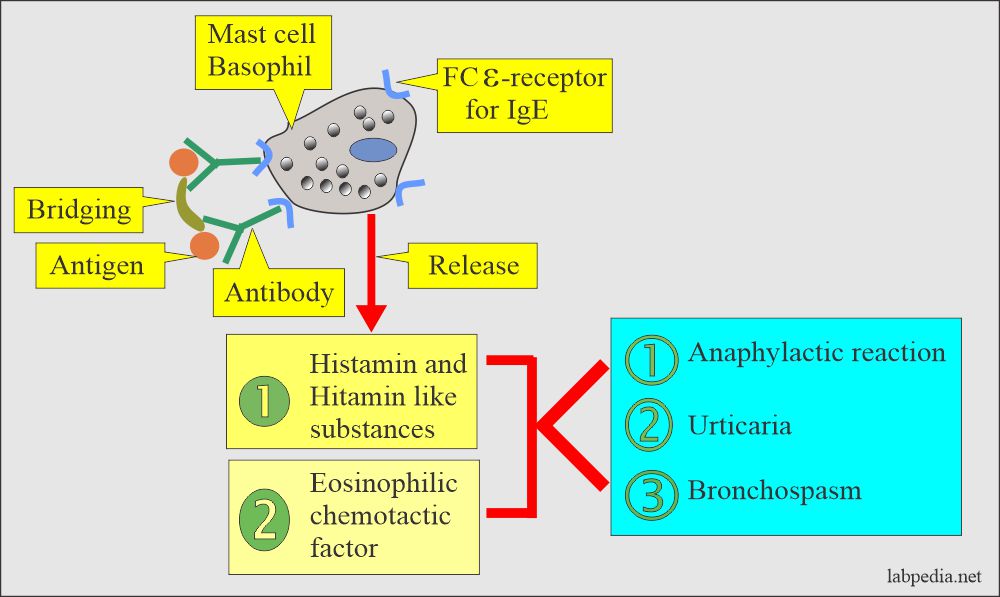
- This is basically a histamine-like reaction or histamine poisoning.
- The main signs and symptoms are due to the pharmacological reaction of histamine or histamine-like substances.
- The following diagram gives a summary of the Type 1 hypersensitivity reaction.
What are the stages of the Type 1 reaction hypersensitivity reaction?
Stage 1:
- The offending antigen attaches to IgE.
Stage 2:
- Activated mast cells and basophils release mediators.
Stage 3:
- Mediators released leads to:
- Vascular changes.
- Activation of platelets.
- Activation of eosinophils.
- Activation of Neutrophils.
- Activation of the coagulation system.
- Plasma histamine levels peak more quickly than tryptase at ∼1o minutes after the onset of an anaphylactic reaction.
- Its level returns to normal within an hour.
- Urine histamine may be elevated for 24 hours.
What are the chemical mediators of type 1 hypersensitivity?
- Histamine increases the vascular permeability and contraction of the smooth muscles.
- Leukotrienes cause the contraction of the lung smooth muscle (bronchospasm).
- Serotonin causes contraction of the smooth muscles.
- PAF (Platelets activating factor) leads to the release of histamine and serotonin from the platelets.
- ECF-A (Eosinophil chemotactic factor) attracts the eosinophils at the antigen and antibody reaction site.
- ECF-A gives rise to the release of secondary mediators.
- Prostaglandins also affect the smooth muscles and vascular permeability.
How will you describe the clinical presentation of a type-1 hypersensitivity reaction?
- Nervousness.
- Itching and urticaria of the skin.
- The feeling of confusion.
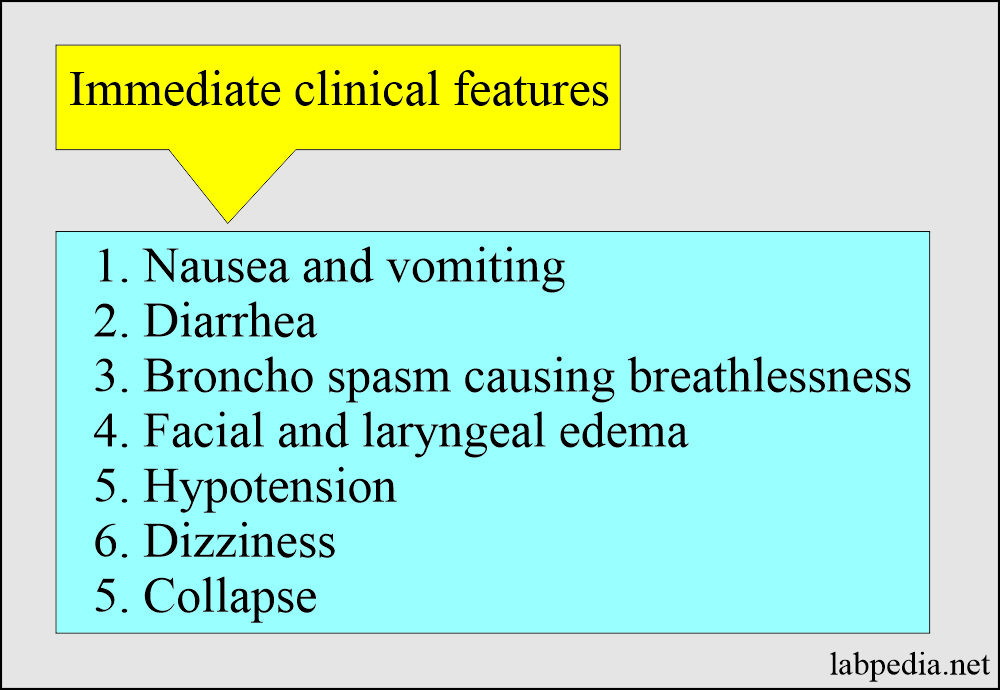
- Nausea, vomiting, and diarrhea.
- Abdominal or back pain.
- There will be flushing, pallor, or cyanosis.
- Urticaria.
- Laryngeal edema leads to stridor (laryngospasm).
- Tachycardia.
- There is low blood pressure.
- Convulsions.
- Respiratory depression.
- Bronchospasm (wheezing) leads to an asthmatic attack.
- Respiratory distress is due to edema.
- Respiratory obstruction is the leading cause of death.
How will you treat an anaphylactic reaction?
- Immediately perform the following measures.
- Stop taking the blood sample or blood donation.
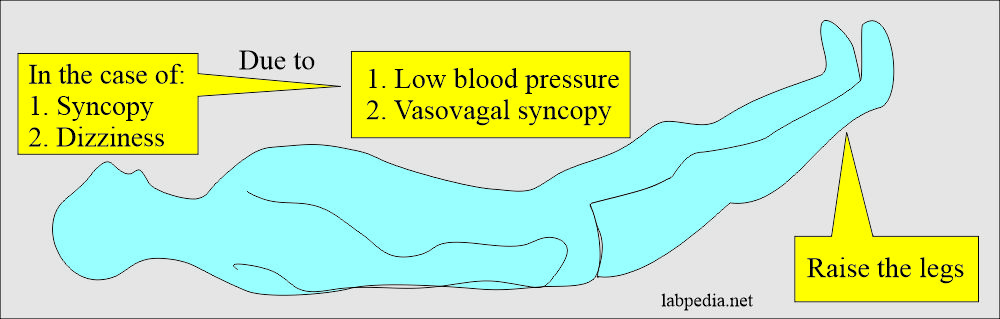
- Lie the patient flat and raise the legs.
- Establish an I/V line.
- Give normal saline infusion for the hypotension.
- Maintain the airway.
- Call the doctor for help.
- Give an injection of antihistamine or decadron (hydrocortisone).
- Give oxygen if needed.
- Monitor blood pressure.
- Give cardiopulmonary resuscitation if needed.
- If the patient does not improve, then transfer the patient to the hospital.
What would you do in a mild reaction?
- Only antihistamines are enough.
What would you do with a severe reaction?
- First, epinephrine (1:1000, 0.3 to 0.5 ml subcutaneous) should be given, followed by corticosteroids (Hydrocortisone 100 mg I/V).
- Another reference: Give I/M 0.5 ml of 1:1000 epinephrine (Adrenaline).
- Repeat after 5 minutes if the shock persists.
- Can repeat epinephrine after 20 minutes.
- If the airway is completely obstructed and has low blood pressure, repeat epinephrine 1:10,000, 3 to 5 ml I/V at one ml/minute.
- Consider dopamine if the blood pressure does not improve.
- H1 and H2 receptor blockers are also effective in hypotension.
- Corticosteroids help to treat the late-phase reaction.
What would you do in a Late-phase reaction?
- It can occur 4 to 6 hours after the first reaction and can be as severe or worse than the initial reaction.
- Late phase reaction can occur up to 72 hours, so the patient’s observation is critical.
Questions and answers?
Question 1: What is the role of Leukotrienes?
Question 2: In case of a reaction during blood collection, what will you do?

Patient suffering generalized type-1 hypersensitivity reaction may present with iching urticaria erythema difficulty in breathing hypotension and tachycardia. If we treat patient with epinephrine this may cause precipited cardaic arrhythmias?
You may be right if having practical experience. I am quoting few references.
For severe allergic reactions which lead to hypotension, epinephrine helps to increase blood flow through veins by constricting blood vessels. By binding to receptors on smooth muscles of the lungs, epinephrine helps to relax the muscles blocking the airways and allows breathing to return to normal.
https://www.aentassociates.com/why-epinephrine-stops-allergic-reactions/#:~:text=For%20severe%20allergic%20reactions%20which,breathing%20to%20return%20to%20normal.