Malarial parasite:- Part 3 – Plasmodium vivax, Benign Tertian Malaria
Plasmodium vivax
What sample is needed for Plasmodium vivax?
- Malarial parasites (MP) may be diagnosed during a fever from a patient’s blood smear.
- The best time to make a smear is during shivering.
- As soon as possible after taking the blood sample, make thick and thin blood smears. If you delay, the parasite may change its morphology.
- A serum is needed for serological methods and PCR.
How will you define Plasmodium vivax?
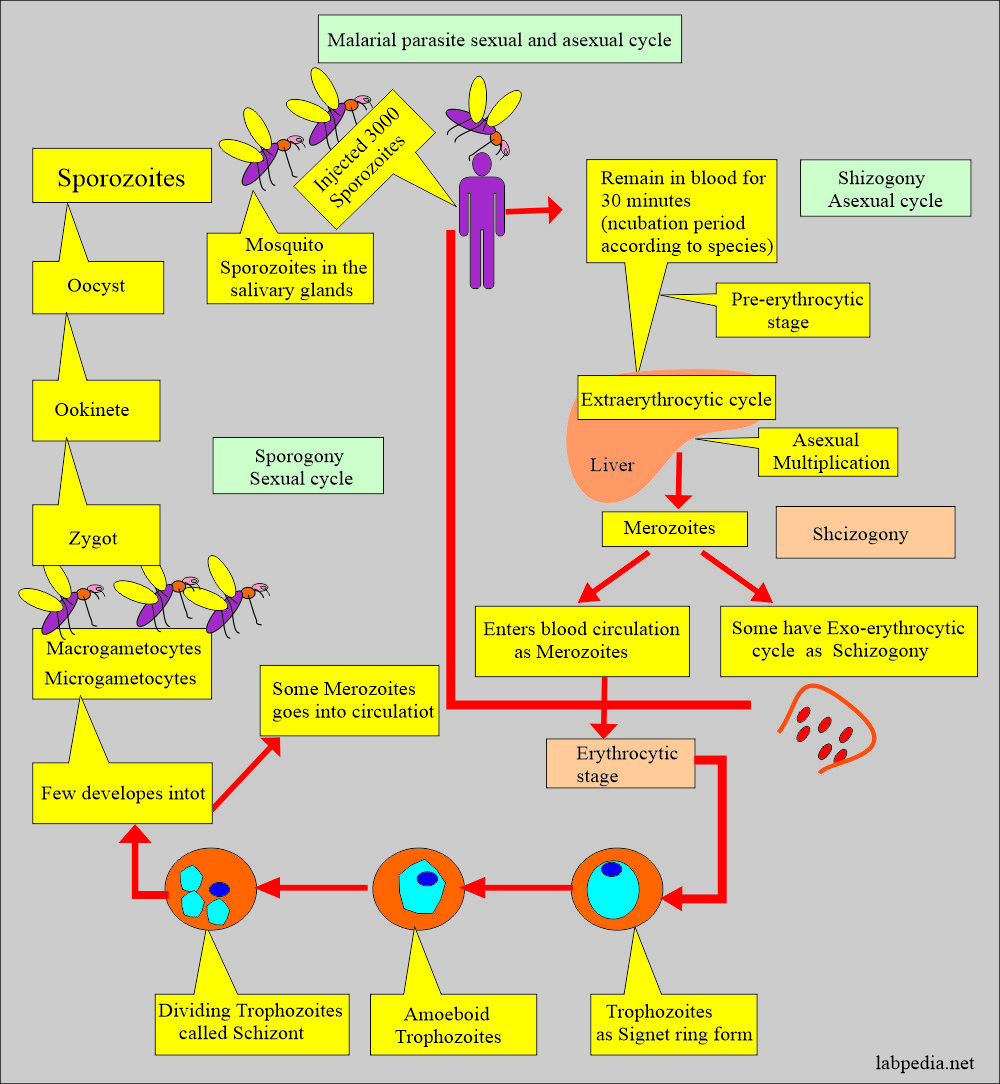
- There is a fever every 48 hours, and it infects young RBCs.
- There may be a relapse for five years.
Why is it called Benign tertiary malaria due to Plasmodium vivax?
- Plasmodium vivax usually causes an acute self-limiting febrile illness, and there is a spike in the fever every third day.
- In this case, there is no complication of death, so-called benign tertiary malaria.
What are the facts about Plasmodium vivax?
- This is the most predominant parasite in most areas of the world.
- 70% to 90% of cases in most of Asia and S. America.
- In SE Asia and the western Pacific, 50% to 60% of cases are seen.
- 1% to 10% of the cases are seen in Africa.
- Plasmodium vivax is the second most significant species and is prevalent in Southeast Asia and Latin America.
- Plasmodium vivax has the complication of a dormant stage in the liver.
- Plasmodium vivax can become active in the liver without mosquito biting, which can lead to clinical symptoms.
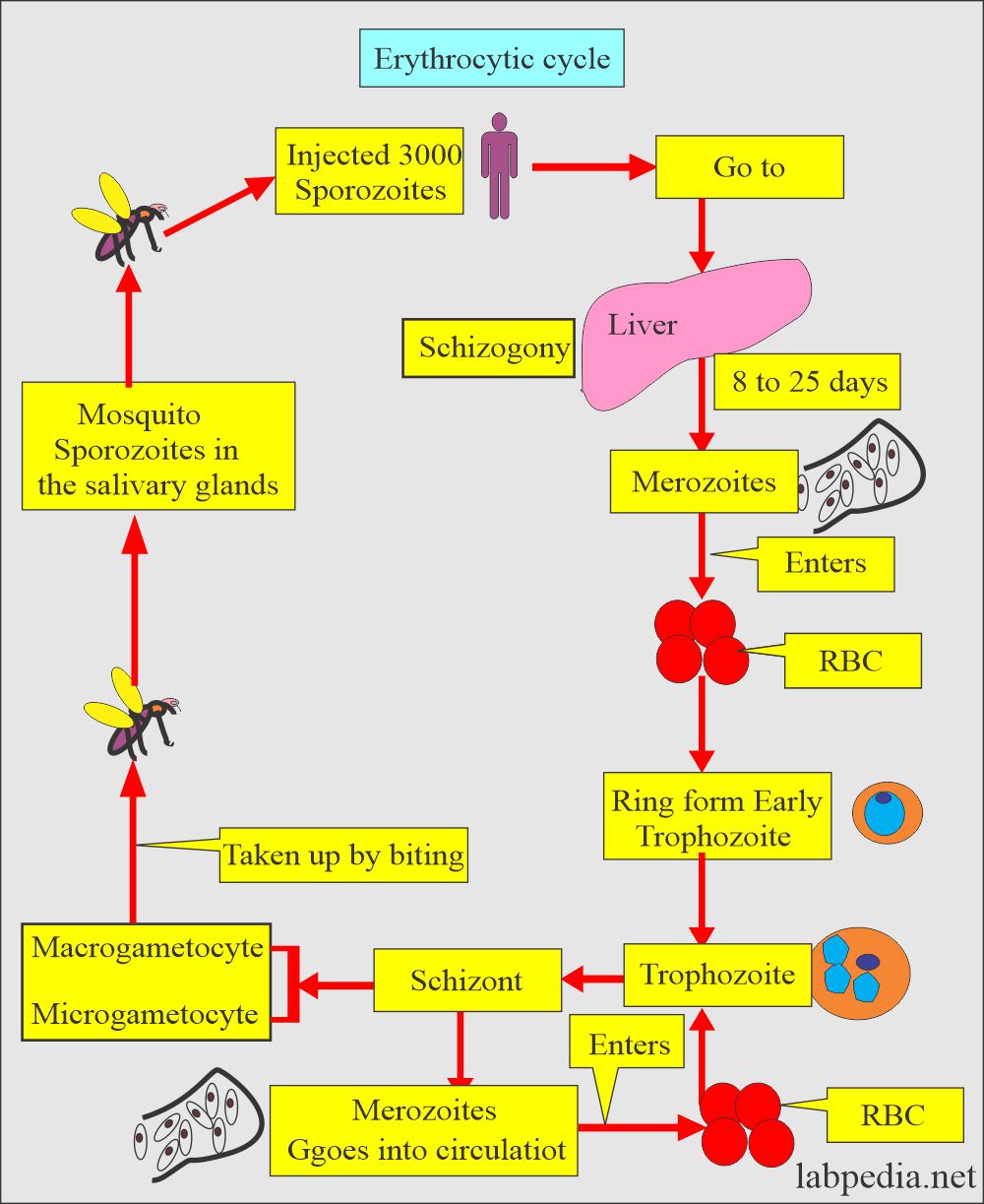
How will you discuss the erythrocytic cycle of Plasmodium vivax?
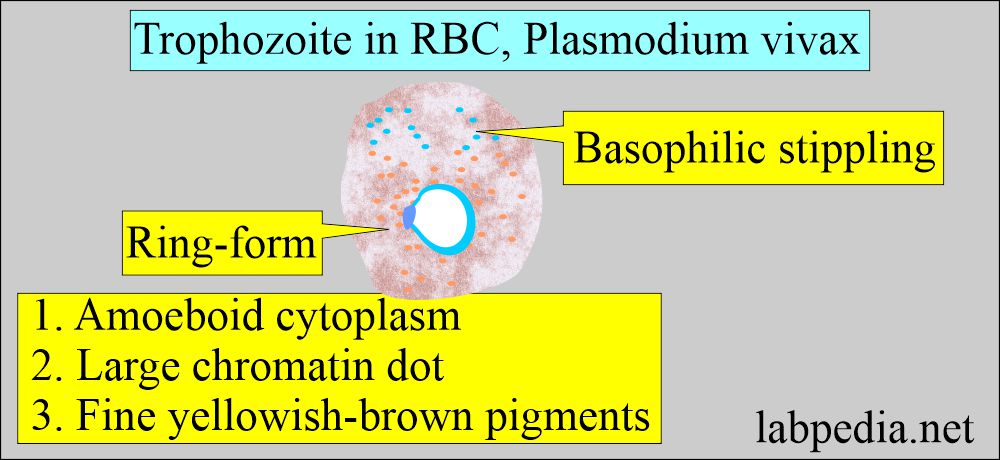
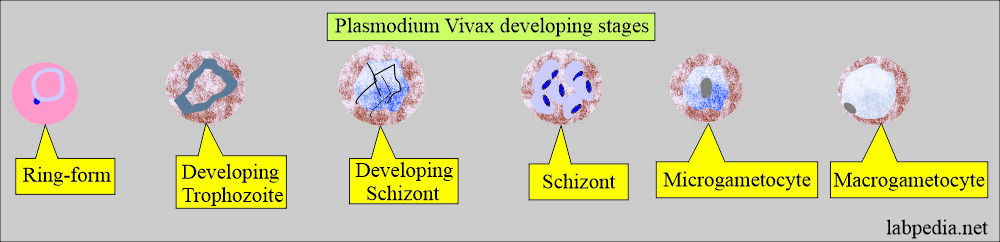
- Plasmodium vivax shows ring form with chromatin dot and cytoplasm.
- It measures 1/3 of the RBC.
- Trophozoite may show remnants of the cytoplasm.
- It has an irregular and amoeboid appearance and a large chromatin dot.
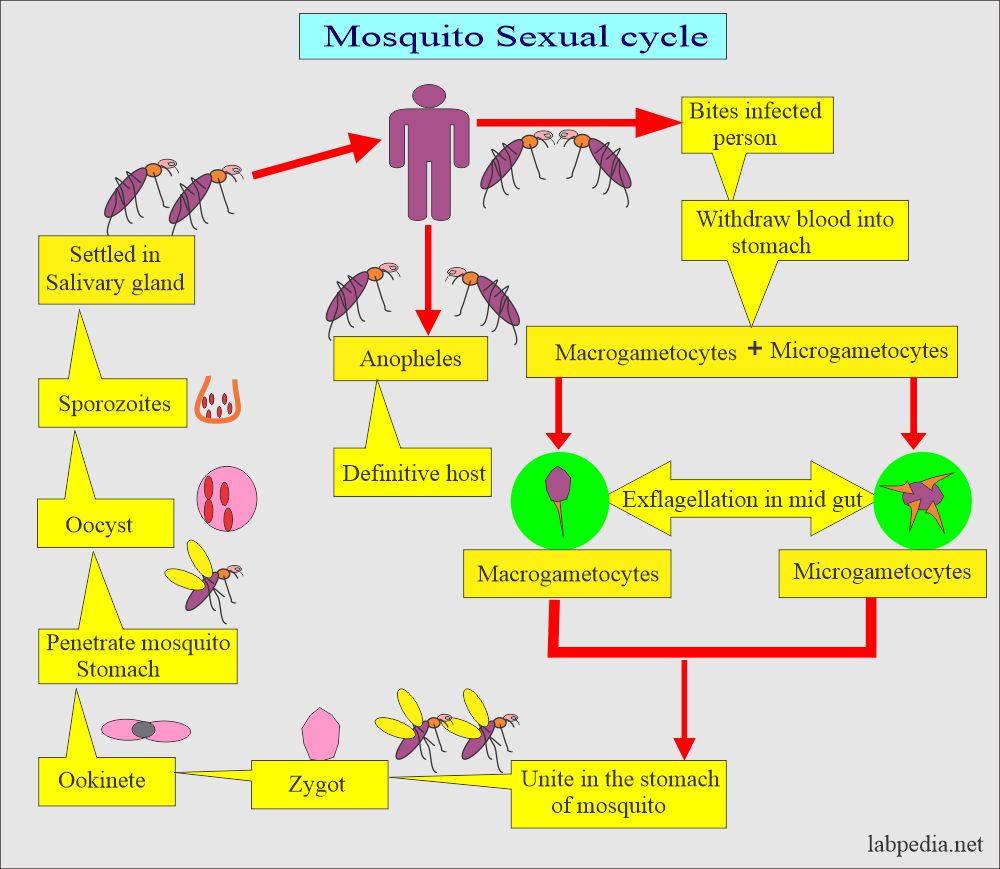
How will you discuss the sexual cycle of Plasmodium vivax?
- The presence of multiple chromatin dots characterizes schizonts.
- Cytoplasm often contains brown pigments.
- There are, on average, 12 to 24 merozoites, with an average of 16.
- These merozoites occupy the majority of RBC.
- Brown pigments may be found.
- Microgametocytes consist of large pink to purple chromatin mass.
- Brown pigments are usually seen.
- The round-to-oval homogenous cytoplasm and eccentric chromatin mass characterize macrogametocytes.
- A diffuse light brown pigment may be visible throughout the parasite.
- Schuffner dots are seen with Giemsa stain.
- Infected RBCs are enlarged and distorted.
What is the clinical presentation of Plasmodium vivax?
- The patient develops signs and symptoms after 10 to 17 days of incubation following the infection (bite from the mosquito).
- Early, there are flu-like symptoms.
- There may be nausea, vomiting, headache, muscle pain, and photophobia.
- The toxins of the parasite give rise to paroxysm, which occurs every 48 hours.
- If the infection becomes chronic, then it may cause damage to the kidney, brain, and liver.
How will you diagnose Plasmodium vivax?
- History of the patient in suspected areas.
- Blood smear:
- Make a blood smear when the patient has a fever. Thin and Thick smears are made.
- The thick smear is more helpful in finding M. Parasites.
- The thin smear is suitable for identifying the type of malarial parasite.
- Collect blood 6 to 8 hourly till 48 hours to declare negative for malaria.
- Giemsa stain is the best choice.
- Serologic methods:
- It is based on immunochromatic techniques. Tests often use a dipstick or cassette format and provide results in 2-15 minutes.
- Polymerase chain reaction (PCR):
- The PCR technique detects parasite nucleic acids. It is more sensitive than smear microscopy, but because of the time needed for this procedure, it is of limited value for diagnosing acutely ill patients.
How will you control Mosquitoes?
- Try to eliminate breeding places:
- Fill the vacant land and pump out the water.
- Remove the junk and water-retaining debris.
- Destroy the larvae:
- Clean the drains.
- Try to remove algae from the ponds.
- Add larva-eating fish to the ponds.
- Use of the insecticide:
- The best example is DDT.
- Use of mosquito repellent:
- Pyrethroid repellent.
- N, N- diethyl meta tolbutamide.
- Use of mosquito nets.
- Use clothes to prevent mosquito bites.
- Train people for malaria prevalence.
- Train the people for the detection of malaria, treatment, and follow-up.
Duration of the various cycles in malarial parasites:
| Type of malarial parasite | Sexual cycle in the mosquito | Length of asexual cycle | Length of the sexual cycle |
| Plasmodium falciparumm | 9 to 10 days | 5 to 7 days | 36 to 48 hours |
| Plasmodium vivax | 8 to 9 days | 8 days | 48 hours |
| Plasmodium ovale | 14 days | 9 days | 48 hours |
| Plasmodium malariae | 15 to 20 days | 15 to 16 days | 72 hours |
Questions and answers:
Question 1: What is the infective stage of the malarial parasite?
Question 2: Why is plasmodium vivax called benign tertiary malaria?