Liver:- Part 4 – Neonatal Jaundice Classification and Diagnosis
Neonatal Jaundice
What sample is needed for Neonatal Jaundice?
- The blood of the neonate is needed.
- In difficult cases, it may get blood from the femoral vein.
- Blood can be obtained from the finger or the heel prick.
How will you define the importance of neonatal jaundice?
- Neonatal jaundice appears in the early days of the newborn.
- If jaundice persists beyond 14 days, it indicates some pathological cause.
- This may be a hemolytic disease of the newborn that starts in utero and causes jaundice, anemia, and hepatosplenomegaly in mature infants.
- The degree of severity of the disease ranges from mild anemia to mental retardation, brain damage, and kernicterus or stillbirth.
- The early diagnosis and the significance of unconjugated hyperbilirubinemia are the potentials for developing Kernicterus.
How will you define Kernicterus?
Definition of kernicterus:
- Kernicterus is the bilirubin staining of the central nervous system and basal ganglia with death or permanent neurologic or mental abnormalities.
- This disease was first studied in the 1950s, and Rh-induced hemolytic anemia was supposed to be the cause.
- 20 mg/dL of the unconjugated bilirubin in mature newborns or 15 mg/dL in premature newborns leads to kernicterus.
What are the causes of kernicterus?
- Acidosis.
- Respiratory distress.
- Very low birth weight.
- Infections.
- In these babies, kernicterus may develop at 15 mg/dL level, and few babies may develop this syndrome as low as 9 to 10 mg/dL of unconjugated bilirubin.
What are the signs and symptoms of kernicterus?
- It causes neurotoxicity.
- There is lethargy and gradual progress in opisthotonus and seizures.
- 70% of the affected neonates die within the first week.
- The rest will have severe brain damage.
- This can be prevented by blood exchange transfusion and phototherapy.
How will you treat kernicterus?
- Some physicians start phototherapy at 15 mg/dL bilirubin level.
- Phototherapy converts unconjugated bilirubin into soluble, nontoxic bilirubin isomers.
- Blood transfusion exchange will be given in severe hemolytic anemia crises.
What are the types of neonatal jaundice?
- Physiologic jaundice.
- Pathologic jaundice.
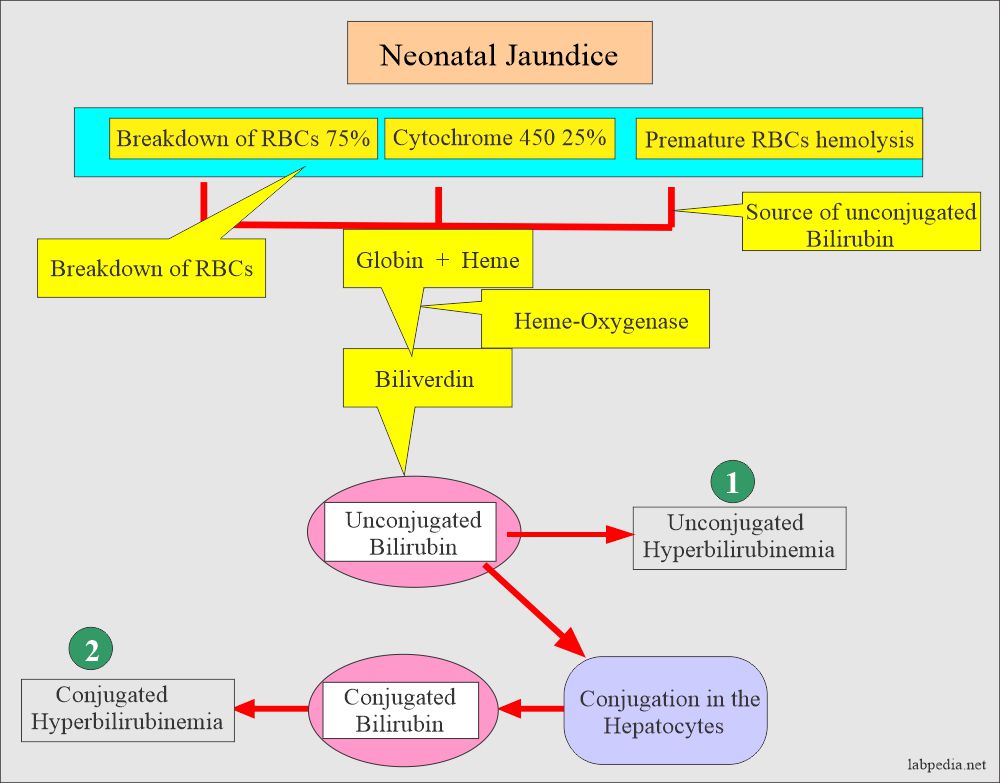
- Neonatal jaundice may be:
- Unconjugated hyperbilirubinemia:
- Physiologic jaundice.
- Hemolytic disease.
- Breast milk hyperbilirubinemia.
- Conjugated hyperbilirubinemia:
- Idiopathic neonatal hepatitis.
- Biliary atresia.
What are the causes of neonatal jaundice?
- Hemolytic disease of the newborn.
- Bacterial sepsis.
- Toxoplasma infection.
- Cytomegalovirus.
- G-6PD deficiency.
- Extensive bruising.
- Other minor causes are:
- Breastfeeding.
- Race.
- H/O maternal smoking.
- H/O prematurity.
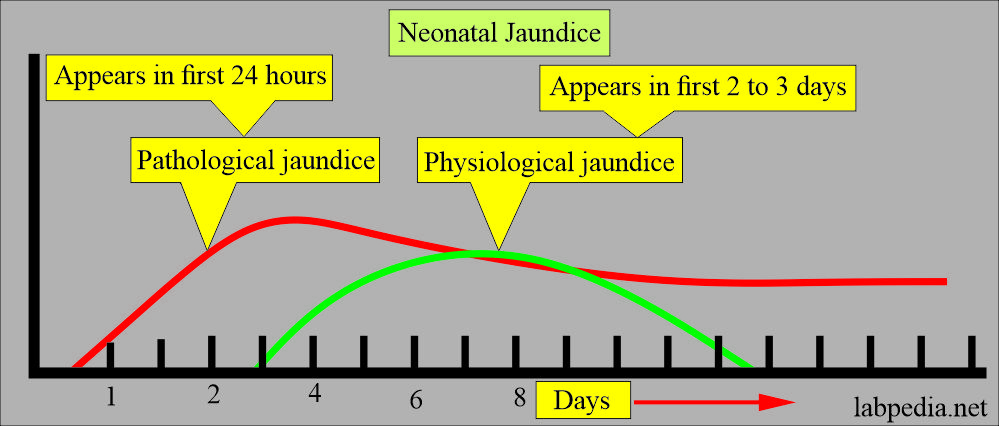
How will you discuss the Physiologic jaundice?
- This is a benign type of jaundice.
- This results from the insufficient hepatocyte enzyme, so unconjugated bilirubin is increased.
- This jaundice appears in the first 2 to 3 days.
- It is pathological jaundice if it goes to 10 to 12 mg/dL on the first day.
- Bilirubin rarely goes above 5 mg/dL per day.
- 90% is unconjugated.
- The peak level lasts 4 to 5 days, and serum bilirubin level is around 5 to 6 mg/dL.
- This jaundice lasts for roughly 2 weeks.
- This is treated by phototherapy (450 nm light source).
- Light converts bilirubin to a stable, nontoxic isomer.
How will you discuss the Pathologic jaundice?
- The most common cause is the hemolytic disease of the newborn (HDN).
- There is severe hyperbilirubinemia.
- The blood-brain barrier is not well developed, so unconjugated bilirubin can cross this barrier.
- The damage to the brain is called Kernicterus.
- In kernicterus, there is yellowness of the subthalamic nucleus, hippocampus, thalamus, putamen, cerebellar nuclei, cranial nerves, and globus pallidus.
- Differentiating points from physiologic jaundice are:
- The appearance of jaundice within the first 24 hours of birth.
- The persistent rise in the bilirubin is beyond one week.
- Persistent jaundice beyond 10 days.
- Bilirubin level exceeding 12 mg/dL.
- If there is a single-day rise of 5 mg/dL.
- Conjugated bilirubin may exceed 2 mg/dL.
Criteria of pathological jaundice:
| Bilirubin level | Criteria of pathological jaundice |
|
|
|
|
|
|
|
|
|
|
|
|
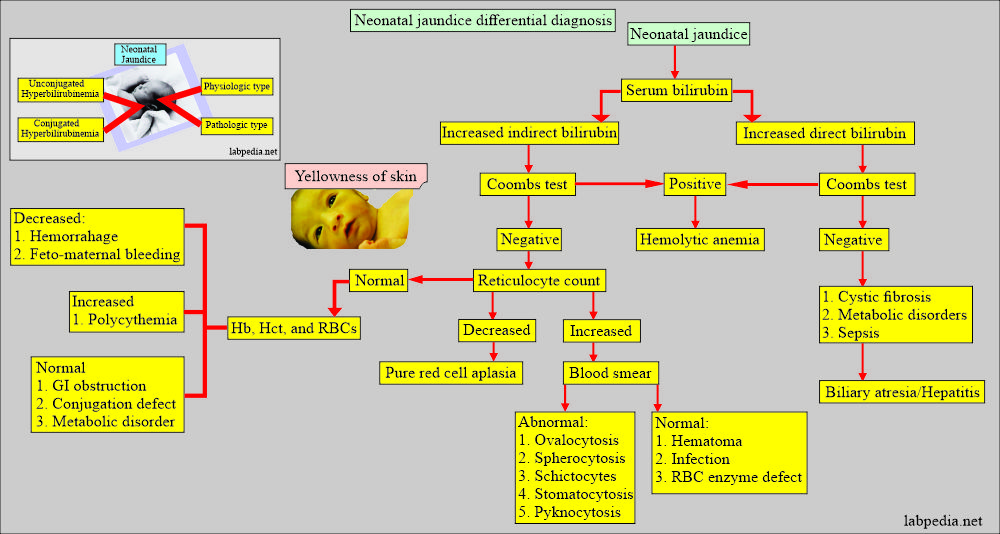
What is the differential diagnosis of neonatal jaundice?
- Jaundice appearing in the first 24 hours suggests:
- Hemolytic disease of the newborn, Erythroblastosis fetalis.
- Sepsis.
- Concealed hemorrhage.
- TORCH infection.
- Jaundice appearing between 3 to 7 days of birth suggests:
- Bacterial infections like urinary tract,
- Jaundice appearing after one week of birth suggests:
- Bacterial sepsis.
- Extrahepatic biliary atresia.
- Cystic fibrosis.
- Breast milk jaundice.
- Congenital absence of bile duct.
- Neonatal hepatitis. Galactosemia.
- Hemolytic anemia (G6PD deficiency and hereditary spherocytosis).
How will you treat Neonatal Jaundice?
- Phototherapy may be considered when the bilirubin level is:
- Above 10 mg/dL before 12 hours of birth.
- Above 12 mg/dL before 18 hours of birth.
- Above 14 mg/dL before 24 hours of birth.
- Phototherapy converts unconjugated bilirubin into a molecule that can be excreted without conjugation.
- Phototherapy is not good for conjugated hyperbilirubinemia.
- Blood exchange transfusion is considered when the bilirubin level exceeds 20 mg/dL.
Questions and answers:
Question 1: When pathological jaundice appears?
Question 2: How you will prevent kernicterus?