Lipoprotein:- Part 2 – Low-Density Lipoprotein (LDL), LDL- Cholesterol (Bad cholesterol)
Low-Density Lipoprotein (LDL)
What sample is needed for low-density lipoprotein (LDL)?
- This is done in the serum.
- Plasma with EDTA can be used, but not with oxalate.
- Get a sample after 12 hours of fasting.
- The sample is stable for 1 to 3 days at 4 °C.
What are the indications for Low-density lipoprotein (LDL)?
- To assess lipid profile.
- To assess the risk of heart disease.
- To monitor the therapy in case of abnormal findings.
How will you discuss the pathophysiology of lipoprotein?
- Lipids are synthesized in the liver and intestine and then transported to many tissues for their metabolic function.
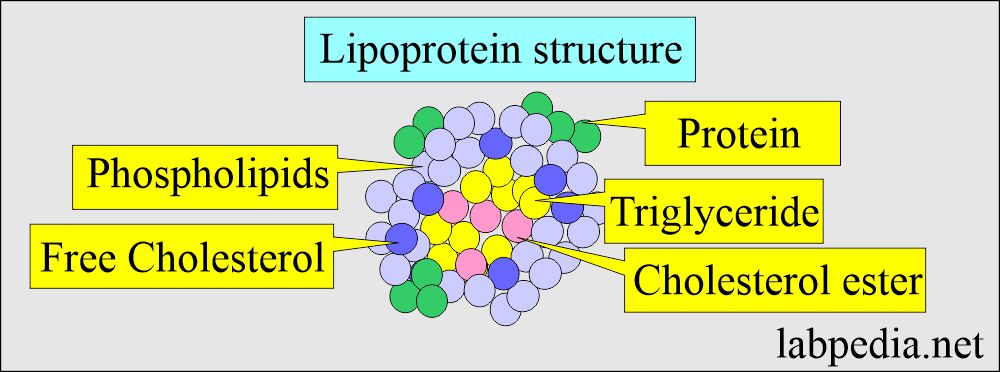
- The lipids are insoluble, so these are transported as macromolecule complexes called lipoproteins.
- Lipoprotein’s simple structure is explained in the following diagram.
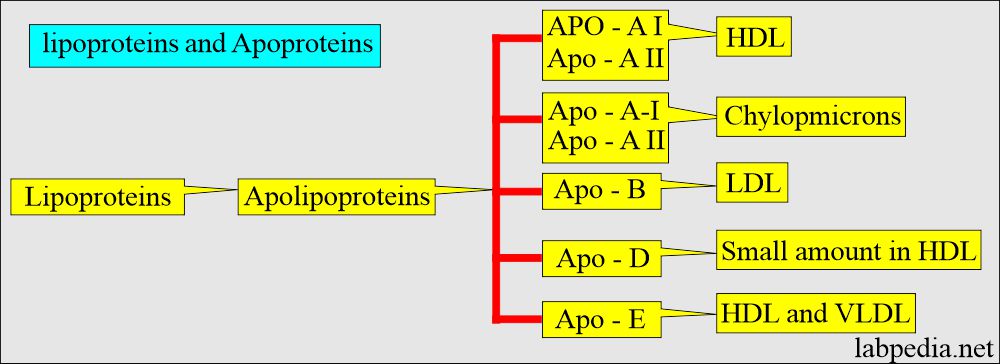
- The outer covering lipoproteins are called Apoproteins, and these are classified into:
- Apo-1.
- Apo-II.
- Apo- B.
- Apo-D.
- Apo-E.
- Apolipoproteins are a hydrophilic component of lipoproteins.
- Lipids like cholesterol and triglycerides are hydrophobic and need to be placed in water-soluble micellar structures (Apolipoproteins) to be transported in the plasma.
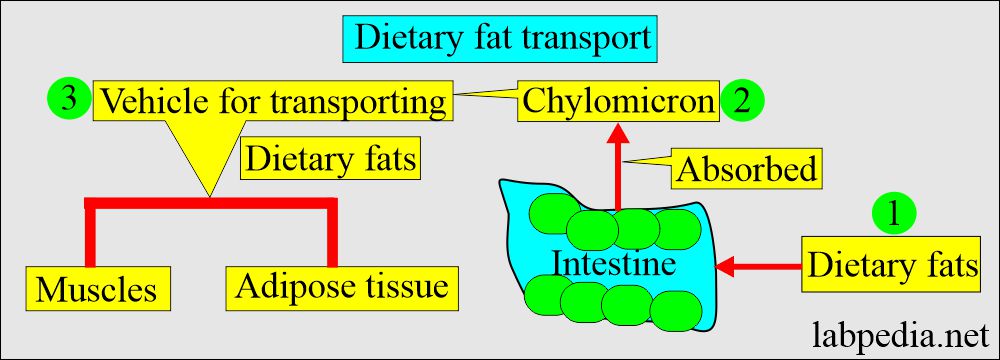
- Fats are absorbed from the intestine as chylomicrons, which transport the dietary fats to the muscles and the adipose tissue.
Low-density lipoprotein (LDL)
- This is the cholesterol carried in the circulation by LDL (Low-density lipoprotein).
- LDL has a longer half-life of 3 to 4 days than its precursors of VLDL.
- The liver and intestinal mucosal cells produce LDL.
- LDL catabolism takes place in the liver and peripheral tissue.
- LDL differs from VLDL because of its lower cholesterol contents and lack of C or E apoproteins.
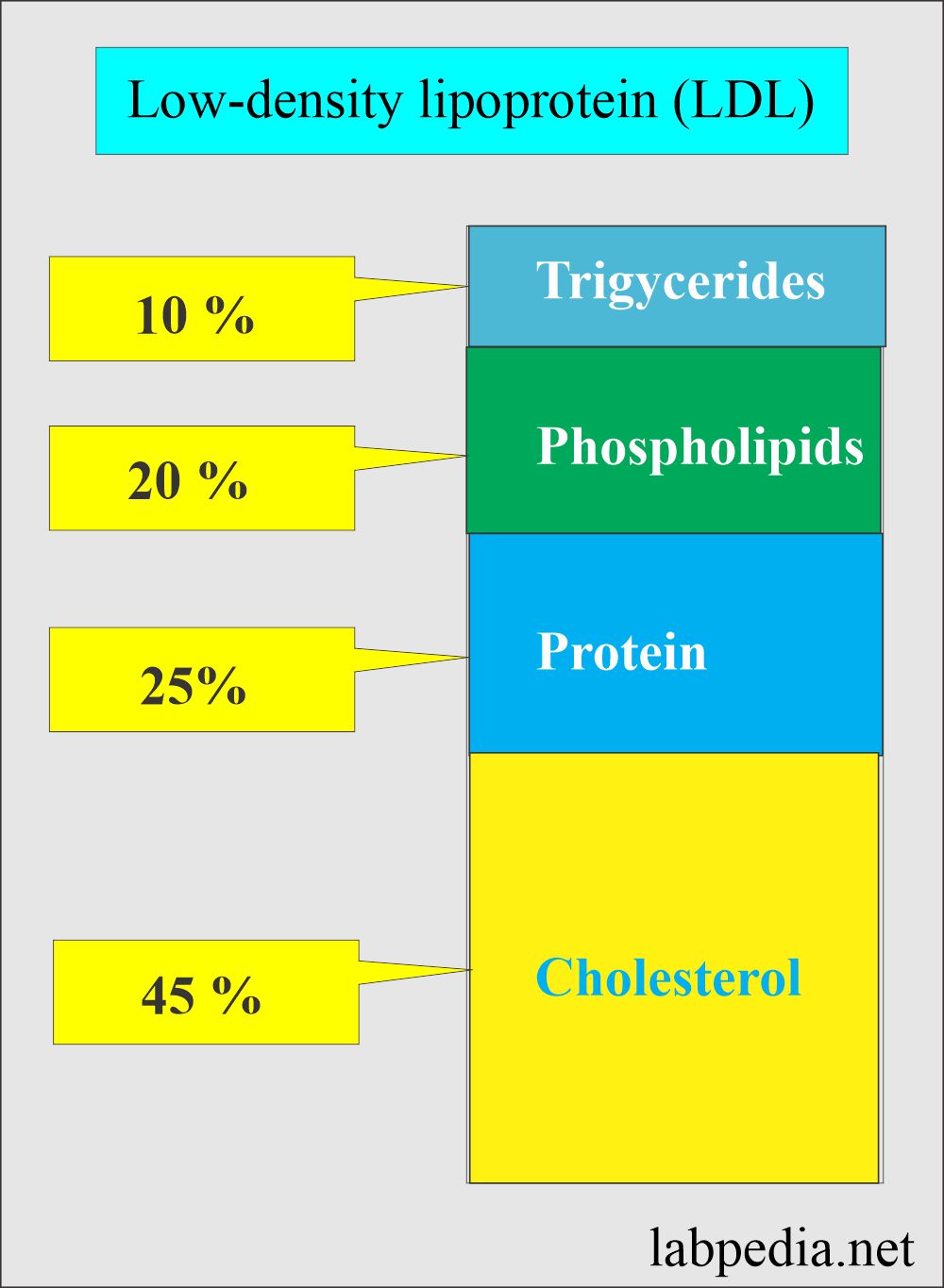
What are the contents of Low-density lipoprotein (LDL)?
- Cholesterol = 45%
- Triglycerides = 10%
- Phospholipids = 20%
- Protein = 25%
- Another source (Teitz Fundamental of Clinical Chemistry):
- Cholesterol 8%.
- Cholesterol esters 42%.
- Triglycerides 6%.
- Phospholipids 22%.
- Apoproteins 22%.
What are the functions of Low-Density Lipoprotein (LDL)?
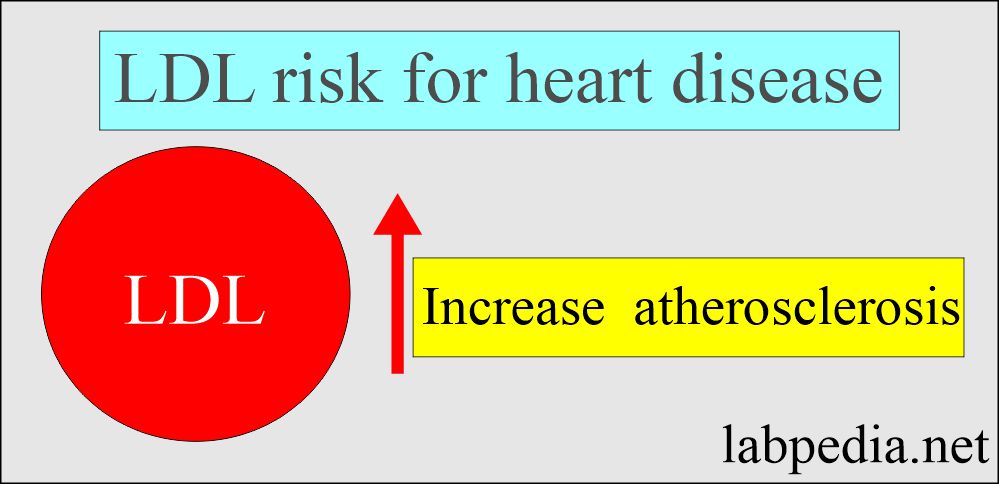
- This is called bad cholesterol.
- Most of the cholesterol carried by the LDL is deposited in the lining of the blood vessels.
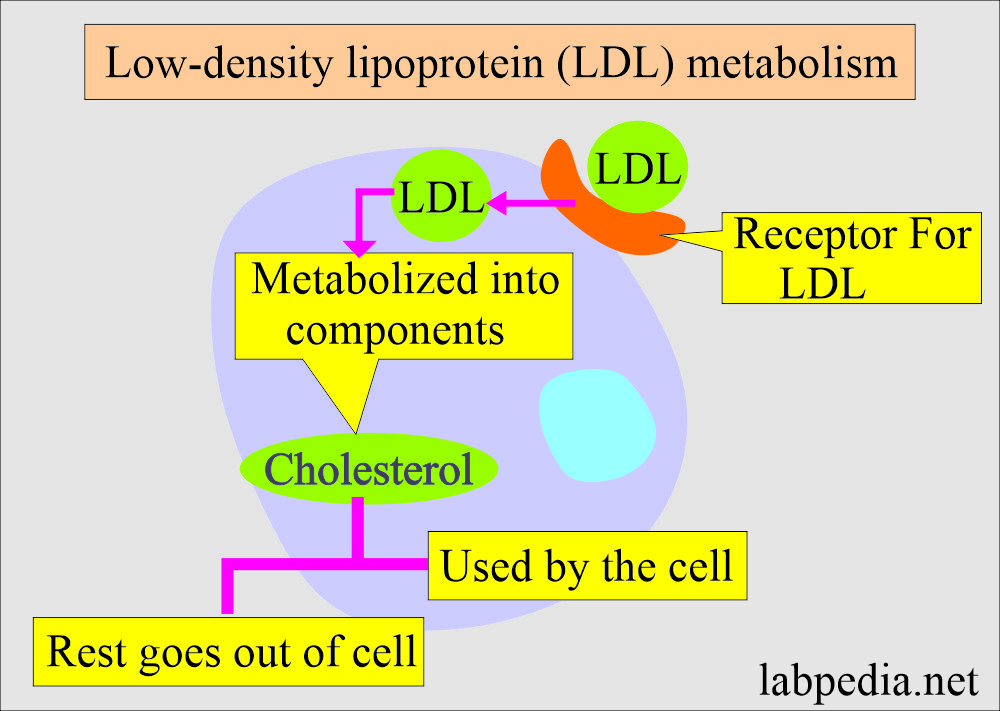
- LDL molecules are taken into the cell through LDL receptors.
- Once inside the cells, LDL is metabolized into its components.
- One of the components, cholesterol, is partly used by the cells and partly goes out into the blood circulation.
- LDL through cholesterol has an atherogenic role.
- LDL increases the risk of atherosclerosis in the coronary arteries (A high LDL level is atherogenic).
- LDL also causes peripheral vascular disease.
- LDL provides cholesterol to other body cells and leads to atherosclerosis of the vessels.
- LDL levels can be lowered by diet, exercise, and statin.
- LDL is mainly metabolized in the liver.
What is the normal low-density lipoprotein (LDL)?
Source 1
LDL-Cholesterol:
| Age | Male mg/dL | Female mg/dL |
| Cord blood | 20 to 56 | 21 to 58 |
| 5 to 9 year | 63 to 129 | 68 to 140 |
| 10 to 14 year | 64 to 133 | 68 to 136 |
| 15 to 19 year | 62 to 130 | 59 to 137 |
| 20 to 24 year | 66 to 147 | 57 to 159 |
| 25 to 29 year | 70 to 165 | 71 to 164 |
| 30 to 34 year | 78 to 185 | 70 to 156 |
| 35 to 39 year | 81 to 189 | 75 to 172 |
| 40 to 44 year | 87 to 186 | 74 to 174 |
| 45 to 49 year | 97 to 202 | 79 to 186 |
| 50 to 54 year | 89 to 197 | 88 to 201 |
| 55 to 59 year | 88 to 203 | 89 to 210 |
| 60 to 64 year | 83 to 210 | 100 to 224 |
| 65 to 69 year | 98 to 210 | 92 to 221 |
| >70 year | 88 to 186 | 96 to 206 |
- To convert into SI unit x 0.0259 = mmol/L
What is the risk of coronary artery disease based on Low-Density Lipoprotein (LDL)?
| Risk for coronary heart disease | LDL level |
|
|
|
|
|
|
Another source of Low-Density Lipoprotein (LDL) safe values:
- Adult = <130 mg/dL
- Children = <110 mg/dL
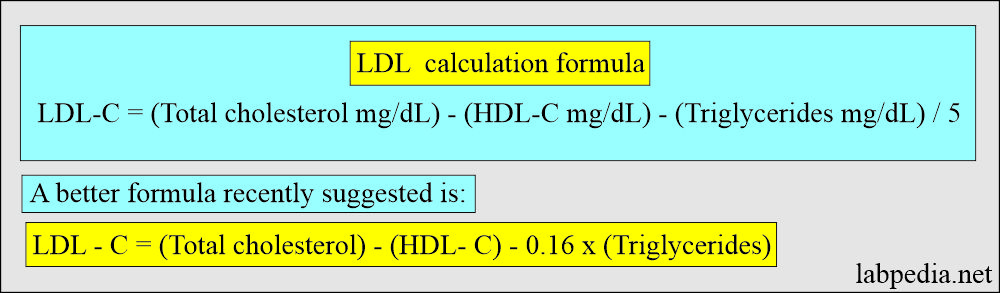
How will you calculate Low-density-lipoprotein (LDL)?
The following formula can calculate the LDL:
- LDL = Total cholesterol – X
- X = (Triglycerides ÷ 5) – HDL
- LDL = Total cholesterol – ([triglycerides ÷ 5] – HDL)
- Another formula is :
- LDL = Total cholesterol – HDL-chol – X
- X = Triglycerides ÷ 5
- OR LDL = Total cholesterol — (HDL cholesterol + 1/5 x Triglycerides)
NOTE: These formulas only help if the fasting triglycerides value is < 400 mg/ dl.
What is the significance of Low-Density Lipoprotein (LDL?
- An elevated level is a major risk factor for atherosclerosis.
What are the conditions where you will see increased Low-Density Lipoprotein (LDL)?
- Familial hyperlipidemia type 2.
- Familial hypercholesterolemia.
- Glycogen storage diseases.
- The secondary causes are :
- Hypothyroidism.
- Nephrotic syndrome.
- Multiple myelomas.
- Dysglobulinemia.
- Liver disease with obstruction.
- Diabetes mellitus.
- Chronic renal failure.
- A diet high in cholesterol and saturated fats.
- Alcohol intake.
- Hepatoma.
What conditions will you see decreased Low-Density Lipoprotein (LDL)?
- Hypolipoproteinemia.
- Hyperthyroidism.
- Hyperlipoproteinemia type 1.
- Chronic anemias.
- Hepatocellular diseases.
- Chronic pulmonary disease.
- Reye’s syndrome.
- Acute stress is like a burn.
- Inflammatory joint disease.
What is the relationship between NCEP classification of total cholesterol and LDL in adults for coronary disease?
| Category | Total cholesterol | LDL-cholesterol |
|---|---|---|
|
|
|
|
|
|
|
|
|
- NCEP = National Cholesterol Education Program.
How will you explain Adult Treatment Panel III (ATP III) for the classification of cholesterol?
- Total cholesterol mg/dL
- Desirable level = < 200 mg/dL
- Borderline level = 200 to 239 mg /dL
- High level = > 240 mg/ dL.
- LDL mg/dL
- Optimal level = <100 mg/ dL.
- Near-optimal level = 100 to 129 mg/dL.
- Border line level = 130 to 159 mg/dL.
- High level = 160 to 189 mg /dL.
- Very high level = >190 mg/ dL.
- HDL mg/dL
- Low level = <40 mg / dL.
- High level = >60 mg / dL.
What are ATP III (Adult Treatment Panel) recommendations for Low-Density Lipoprotein (LDL)?
| Risk Group | Risk Factors | Target or desirable level of LDL |
| Presence of coronary heart disease (CHD) or CHD-equivalent |
|
<100 mg/dL |
| 2 or more major risk factors | Major risk factors are:
|
<130 |
| >2 major risk factors | Above are the major risk factors | <160 mg/dL |
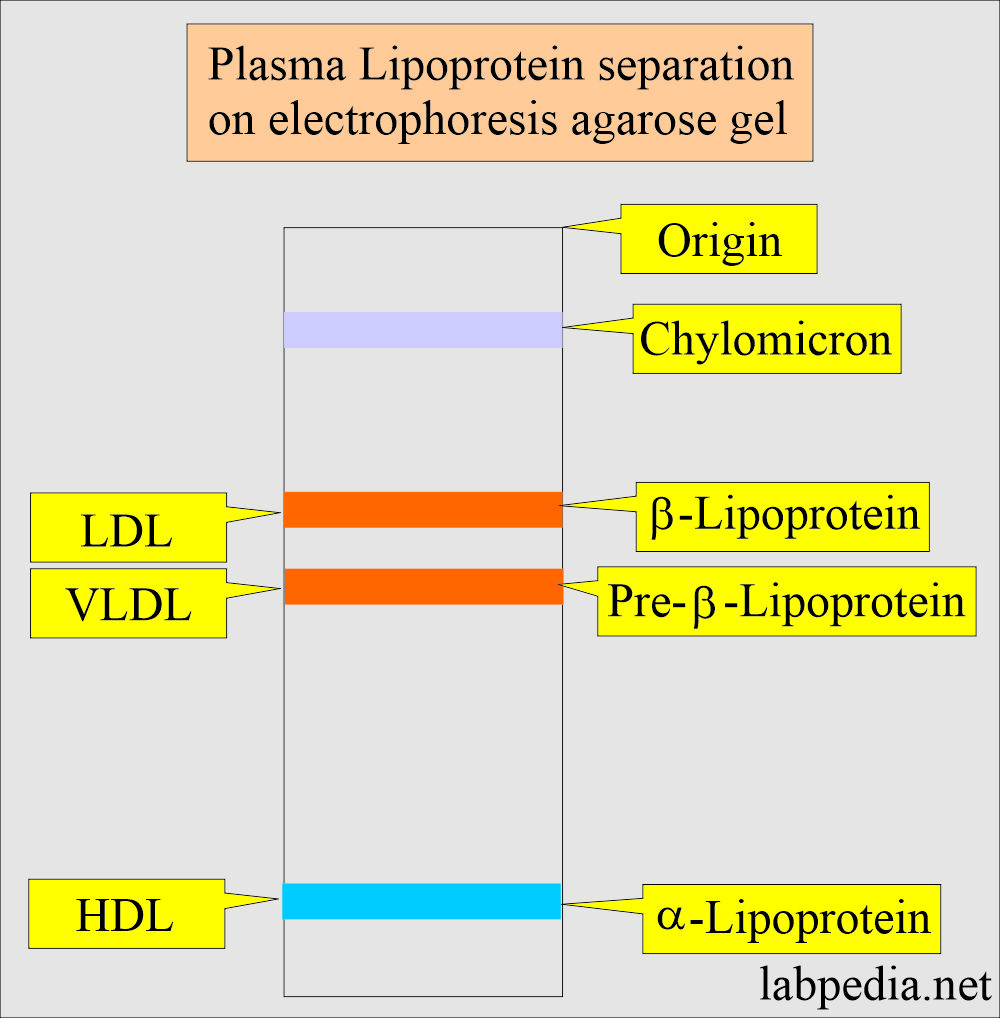
How will you summarize the characteristics of the lipoproteins?
| Characteristics | Chylomicron | HDL | LDL | VLDL |
| Plasma appearance | Creamy layer, slightly turbid | Clear | Clear or yellow-orange tint | Turbid to opaque |
| Size (diameter nm) | >70.0 | 4 to 10 | 19.6 to 22.7 | 25 to 70 |
| Electrophoretic mobility | Origin | α – region | β – region | Pre – β region |
| Molecular weight | 0.4 to 30 x 109 | 3.6 x 109 | 2.75 x 109 | 5 to 10 x 109 |
| Synthesized in (Tissue of origin) | Intestine | Intestine and liver | Intravascular | Liver and intestine |
| Composition by weight in % | ||||
| Cholesterol esterified |
|
|
|
|
| Cholesterol unesterified |
|
|
|
|
| Triglycerides |
|
|
|
|
| Phospholipids |
|
|
|
|
| Proteins |
|
|
|
|
| Triglycerides | Markedly raised | Normal | Normal/ Raised | Moderately to Markedly raised |
| Clinical significance of | Pancreatitis and acute abdomen | Decreased risk of CAD | Increased risk of CAD | Increased risk of CAD |
| Functions | Transport dietary lipids to tissue | Carry cholesterol from tissue to liver | Carries cholesterol to tissue | Transport endogenous TG from the liver to adipose tissue |
Questions and answers:
Question 1: What is the risk of LDL for coronary artery disease?
Question 2: What will happen to LDL in hyperthyroidism?