Lipoprotein: – Part 1 – High-Density Lipoprotein (HDL), HDL-Cholesterol (HDL-C), Lipoprotein
High-Density Lipoprotein (HDL)
What sample is needed for High-Density Lipoprotein (HDL)?
- This test is done on the serum.
- A fasting sample is preferred. Advised the patient to fast for 12 to 14 hours.
- This test can be done on plasma as well.
- Serum or plasma can be stored at 4 °C for 4 days (5 to 7 days).
What are the precautions for High-Density Lipoprotein (HDL)?
- Don’t use oxalate, fluoride, citrate, or heparin to collect blood.
- HDL values are age and sex-related.
- HDL value is increased in Hypothyroidism and decreased in Hyperthyroidism.
- Drugs that increase the value are oral contraceptives, aspirin, phenothiazine, steroids, and sulphonamides.
- Smoking and alcohol decrease HDL value.
What are the Indications for High-Density Lipoprotein (HDL)?
- Advised to evaluate coronary artery disease risk.
- This can be advised as part of a lipid profile.
How will you discuss the pathophysiology of Lipoproteins?
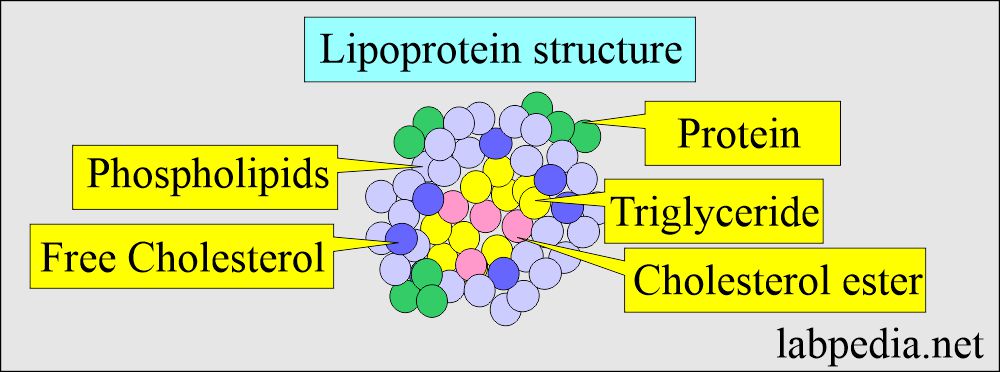
- Lipoproteins are insoluble and are transported in the plasma as a macromolecular complex.
- Lipoproteins are sphericle particles with:
- Nonpolar lipids are triglycerides and free cholesterol.
- Polar lipids are phospholipids and free cholesterol.
How will you classify Lipoprotein?
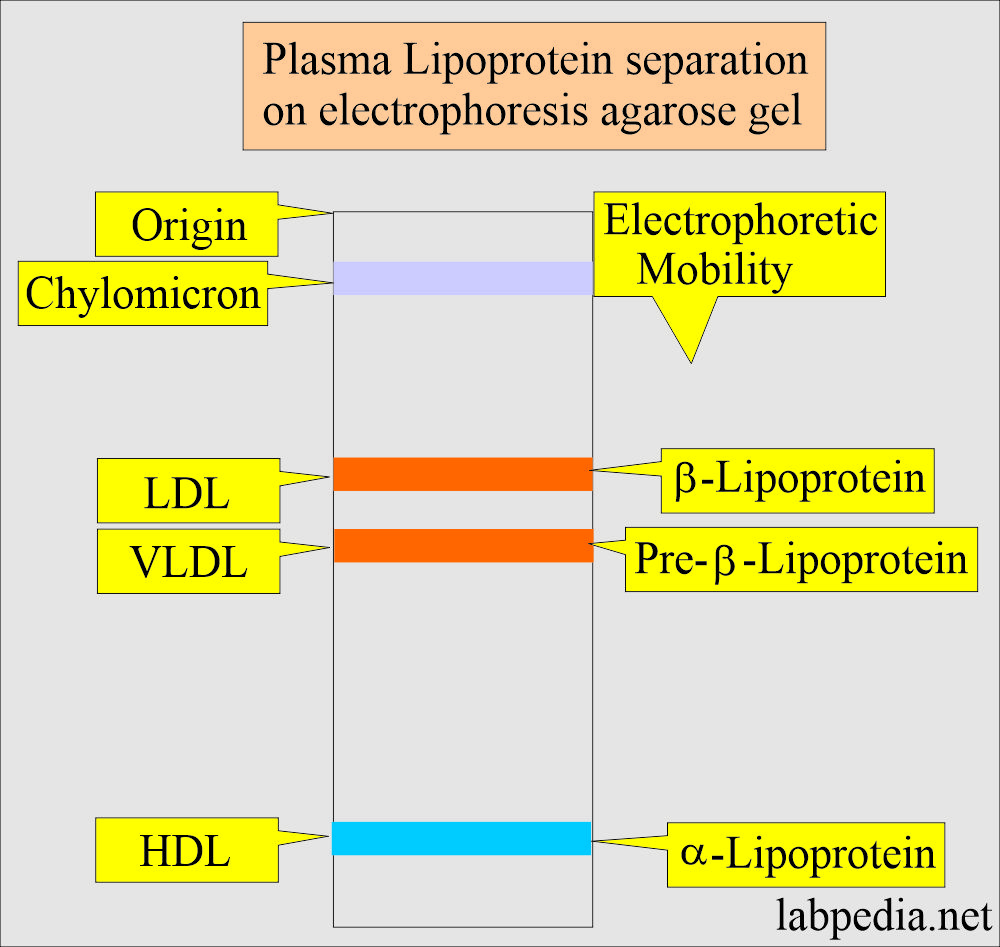
- It is classified on electrophoresis based on its physical and chemical structure as follows:
-
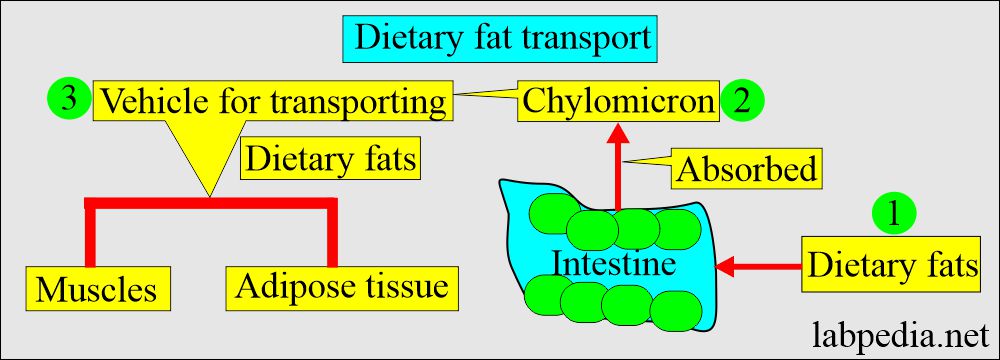
Chylomicron:
- These are primarily triglycerides.
- These are the vehicles where lipids are absorbed from the intestine and can enter the bloodstream.
-
LDL:
- Beta-lipoprotein is the primary carrier of cholesterol.
- It arises primarily from the degradation of VLDL into LDL1, called intermediate-density lipoprotein (IDL).
- LDL-1 is short-lived, and it is converted into LDL-2.
- LDL-2 will remove some of the triglyceride load.
- LDL is a membrane protein.
- There are tissue receptors on the cells, which are engulfed by the cells and degraded by the lysosomal enzymes.
-
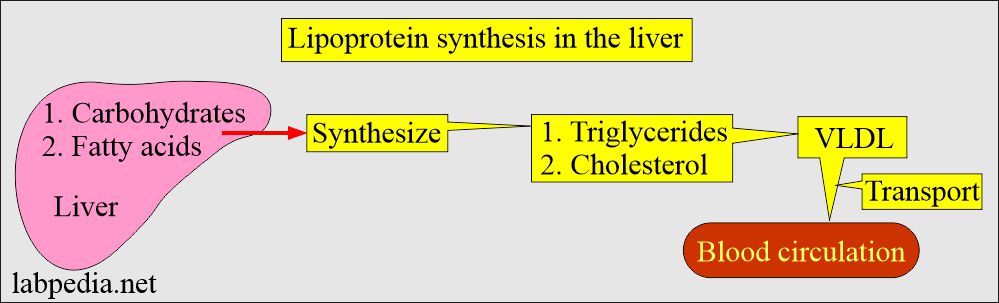
VLDL:
- It is Pre-beta – lipoproteins, which are mainly triglycerides.
- It originates in the liver and transports triglycerides from the liver to other tissues.
-
HDL:
- α–Lipoproteins are mainly proteins with a small amount of cholesterol.
- It arises from the liver and intestine and primarily contains apolipoproteins A-I and A-II.
- It is a cholesterol scavenger and removes cholesterol from the tissues.
- HDL will esterify cholesterol and carry it to the liver for removal.
- HDL converts cholesterol into bile acids and excretion into bile.
- The outer covering lipoproteins are called Apoproteins, and these are classified into:
- Apo-1.
- Apo-II.
- Apo- B.
- Apo-D.
- Apo-E.
How will you classify Apolipoprotein?
| Apolipoproteins | Type of lipoprotein | Molecular mass in Da |
|
|
|
|
|
|
|
It is secreted with chylomicron and transferred to HDL |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- Apolipoproteins are a hydrophilic component of lipoproteins.
- Lipids like cholesterol and triglycerides are hydrophobic and must be placed in water-soluble micellar structures (Apolipoproteins) to be transported in the plasma.
- In the case of endogenous pathways, the lipoproteins are synthesized in the liver from carbohydrates and fats.
How will you summarize Lipoproteins?
| Type of lipoprotein | Apoprotein contents | Electrophoresis pattern | The main type of lipids | % of Apoprotein | Origin tissue | Functions |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
High-density lipoprotein (HDL)
- HDL cholesterol is synthesized and secreted into the liver and intestine.
- This can be separated by electrophoresis and ultracentrifugation.
- HDL comprises phospholipids and apolipoprotein (Apo A-1 and Apo – A-II), almost 90% of the total protein.
- The ratio of Apo- A-1 to Apo- A-11 is ∼ 3:1 by weight.
- HDL from the intestine does not contain Apo-C or Apo-E and only contains Apo-A.
- The dominant Apoprotein is Apo-A I (67%), followed by A-II, C, and E.
- This may be responsible for the transport of dietary cholesterol.
- HDL plays a role in transporting cholesterol to the liver from the tissue excreted in the bile.
- HDL transports cholesterol to the liver, where cholesterol is the precursor of the bile acids or part of the VLDL component.
- While lipoproteins transport cholesterol, triglycerides, and other insoluble fats.
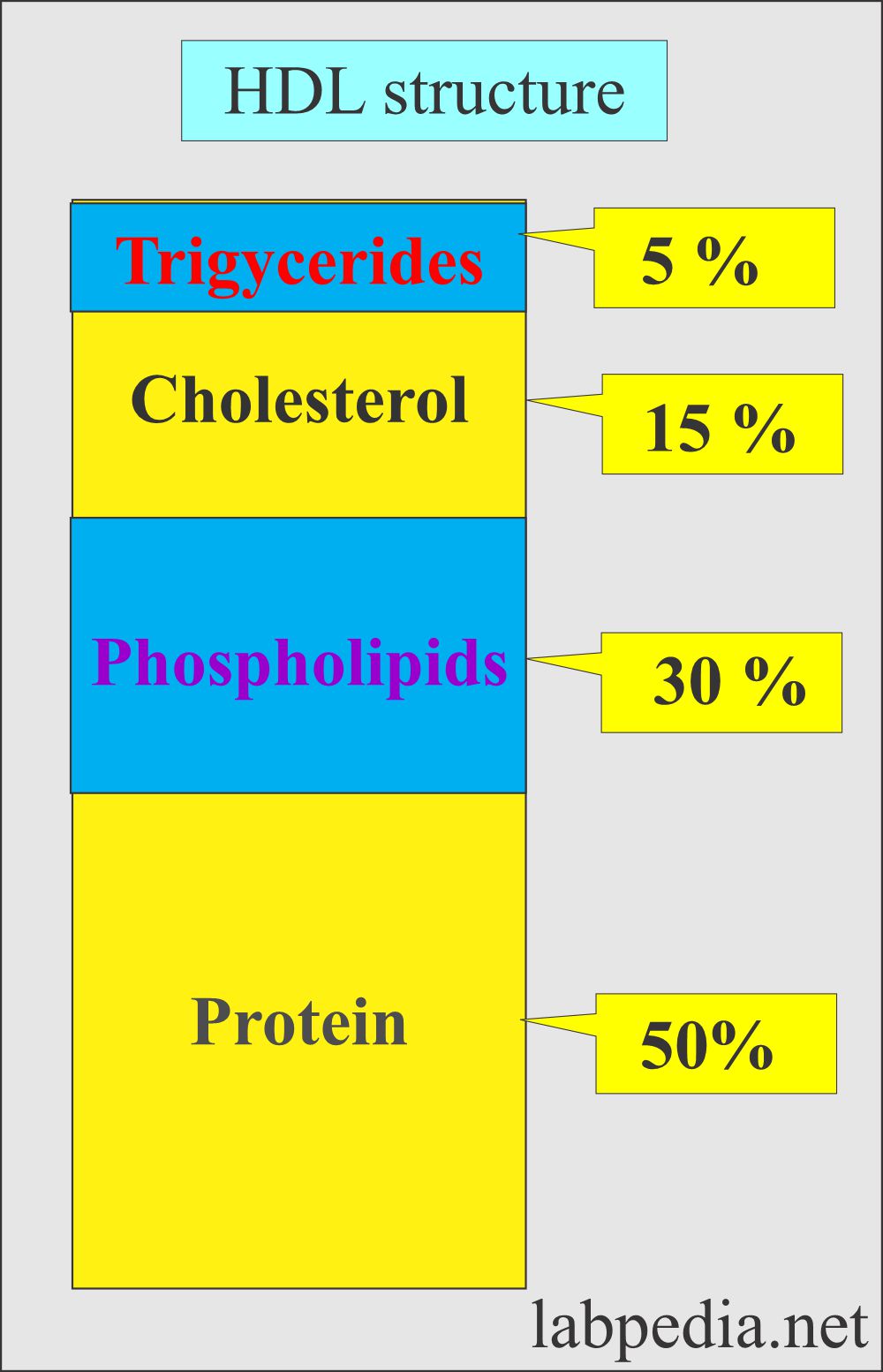
- HDL (Composition) consists of the following:
- Cholesterol = 6%.
- Cholesterol ester = 13%.
- Triglycerides = 3%.
- Phospholipids = 28%.
- Protein = 50%.
- HDL has very few triglycerides.
- There is a high percentage of proteins, phospholipids, and cholesterol.
- Another source says:
- Triglycerides = 5%
- Cholesterol = 15%
- Phospholipids = 30%
- Proteins = 50%
- The ratio of esterified and free cholesterol is 3:1.
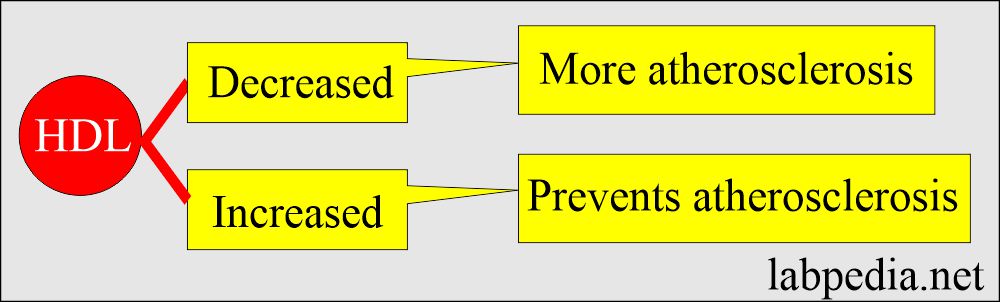
- The decreased level of HDL is atherogenic.
- HDL Raised level protects against atherosclerosis by removing the cholesterol from the arteries and taking it to the liver.
- HDL and LDL may combine to maintain cellular Cholesterol balance by moving cholesterol into the arteries and HDL removing it from the arteries.
- HDL-C is good cholesterol proportional to coronary artery disease (CAD) risk.
- The treatment is not indicated when a high HDL with a high cholesterol level exists.
What are the Functions of High-density lipoprotein (HDL)?
- HDL is the carrier of cholesterol from the peripheral tissue.
- HDL carries cholesterol from peripheral tissue to the liver for excretion in the bile, a process known as reverse cholesterol transport.
- HDL has a protective role by preventing cellular uptake of cholesterol and lipids.
- HDL protects against cardiovascular diseases.
What is the relationship between HDL and coronary heart disease?
| Risk of heart disease | Male | Female |
|---|---|---|
|
|
|
|
|
|
|
|
|
What is the total cholesterol/HDL-cholesterol ratio?
- The ratio is very important to know the risk of coronary heart disease.
- A high ratio is associated with increased risk.
- The normal ratio should be at least 5:1, and the best is 3:1.
What is the relationship between Total cholesterol/HDL-cholesterol Ratio Risk for Coronary disease?
| Risk | Women | Men |
|
|
|
|
|
|
|
|
|
|
|
|
- HDL-cholesterol level of 70 mg/dl or greater is associated with longevity of life.
What is the normal High-density lipoprotein (HDL)?
Source 1
HDL-Cholesterol
| Age | Male mg/dL | Female mg/dL |
| Cord blood | 6 to 53 | 13 to 56 |
| 5 to 9 year | 38 to 75 | 36 to 73 |
| 10 to 14 year | 37 to 74 | 37 to 70 |
| 15 to 19 year | 30 to 63 | 35 to 74 |
| 20 to 24 year | 30 to 63 | 33 to 79 |
| 25 to 29 year | 31 to 63 | 37 to 83 |
| 30 to 34 year | 28 to 63 | 36 to 77 |
| 35 to 39 year | 29 to 62 | 34 to 82 |
| 40 to 44 year | 27 to 67 | 34 to 88 |
| 45 to 49 year | 30 to 64 | 34 to 87 |
| 50 to 54 year | 28 to 63 | 37 to 92 |
| 55 to 59 year | 28 to 71 | 37 to 91 |
| 60 to 64 year | 30 to 74 | 38 to 92 |
| 65 to 69 year | 30 to 75 | 35 to 96 |
| >70 year | 31 to 75 | 33 to 92 |
- To convert into SI unit x 0.0259 = mmol/L
Source 2
HDL
- Male = >50 mg/dL
- Female = >55 mg/dL
Another source
HDL
- Men= 36 to 65 mg/dl or > 45 mg/dl (>0.75 mmol/L).
- Women= 35 to 80 mg/dl or > 55 mg/dl (>0.91 mmol/L).
Abnormal values of HDL:
| HDL value | Risk for coronary disease (CAD) |
|
|
|
|
|
|
|
|
|
|
| Critical values | |
|
|
|
|
What conditions will you see increased High-Density Lipoprotein (HDL)-C?
- When it is >60 mg/dL.
- Chronic liver diseases like cirrhosis, hepatitis, and alcoholism.
- Long-term vigorous exercises.
- Familial hyper-alpha-lipoproteinemia.
- The increased level may be due to some drugs.
- Estrogen therapy.
- Moderate intake of alcohol.
- Insulin therapy.
- Hypobetalipoproteinemia.
What conditions will you see decreased High-Density Lipoprotein (HDL)-C?
- When it is <40 mg/dL.
- Poorly controlled diabetes
- Cholestasis.
- Chronic renal failure, uremia, and nephrotic syndrome.
- Hypertriglyceridemia.
- Familial hypo-alpha-lipoproteinemia.
- Alpha and beta – lipoproteinemia.
- The decreased level may also be seen in some of the drugs.
- Steroids.
- Antihypertensive drugs.
- Diuretics.
- Beta-blockers.
- Thiazide.
- The secondary causes are:
- Stress and recent illnesses like AMI, stroke, and surgery.
- Starvation and a nonfasting sample are 5% to 10% lower.
- Diabetes mellitus.
- Hypothyroidism.
- Liver diseases.
- Uremia and nephrosis.
How will you summarize the characteristics of the lipoproteins?
| Characteristics | Chylomicron | HDL | LDL | VLDL |
| Plasma appearance | Creamy layer, slightly turbid | Clear | Clear or yellow-orange tint | Turbid to opaque |
| Size (diameter nm) | >70.0 | 4 to 10 | 19.6 to 22.7 | 25 to 70 |
| Electrophoretic mobility | Origin | α – region | β – region | Pre-β-region |
| Molecular weight | 0.4 to 30 x 109 | 3.6 x 109 | 2.75 x 109 | 5 to 10 x 109 |
| Synthesized in (Tissue of origin) | Intestine | Intestine and liver | Intravascular | Liver and intestine |
| Composition by weight in % | ||||
| Cholesterol esterified | 5 | 38 | 49 | 11 to 14 |
| Cholesterol unesterified | 2 | 10 | 13 | 5 to 8 |
| Triglycerides | 84 | 9 | 11 | 44 to 60 |
| Phospholipids | 7 | 22 | 27 | 20 to 23 |
| Proteins | 2 | 21 | 23 | 4 to 11 |
| Triglycerides | Markedly raised | Normal | Normal/ Raised | Moderately to Markedly raised |
| Clinical significance of | Pancreatitis and acute abdomen | Decreased risk of CAD | Increased risk of CAD | Increased risk of CAD |
| Functions | Transport dietary lipids to tissue | Carry cholesterol from tissue to liver | Carries cholesterol to tissue | Transport endogenous TG from the liver to adipose tissue |
Questions and answers:
Question 1: What is the role of HDL.
Question 2: What is the role of LDL.