Human Immunodeficiency Virus (HIV), AIDS (Acquired immunodeficiency syndrome)
Human immunodeficiency virus (HIV), AIDS (Acquired immunodeficiency syndrome)
What sample is needed to detect Human Immunodeficiency Virus (HIV)?
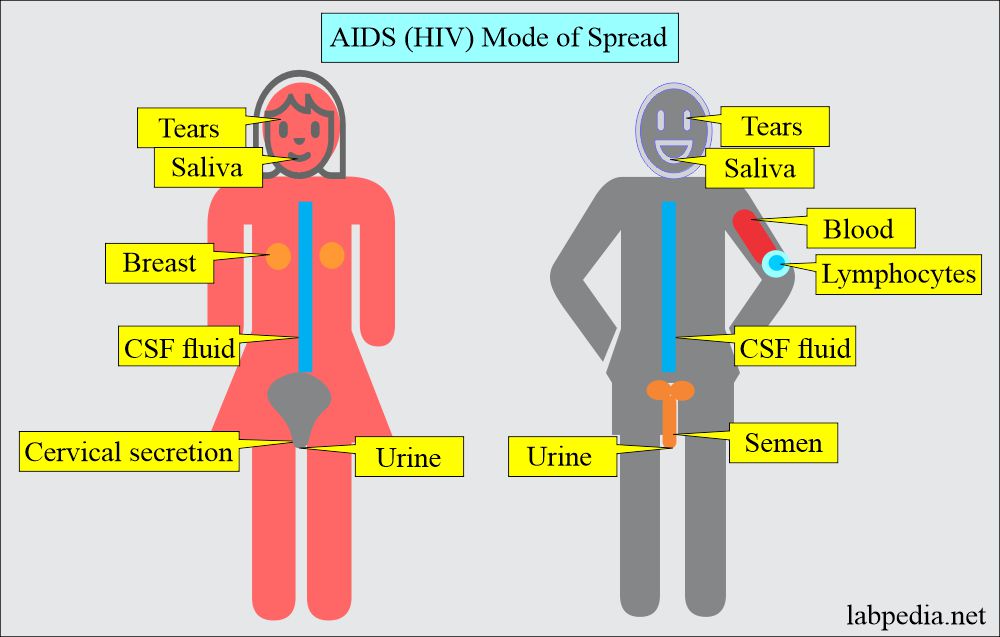
- For serological tests, the serum is the best sample.
- These tests can be done on plasma as well.
- Oral fluids.
- Urine.
- Cerebrospinal fluids.
- Genital secretions.
- Tears.
- Breast milk.
What are the indications for Human immunodeficiency virus (HIV) diagnosis?
- These serological tests are done to diagnose HIV infection.
- For the diagnosis of Acquired Immune Deficiency Syndrome.
How will you define Human immunodeficiency virus (HIV)?
- Human immunodeficiency viruses (HIV) are retroviruses; their genetic (genome) information comprises RNA viruses.
- Formerly, it was called Human T-lymphocytic virus III (HTLV III).
- It is a non-oncogenic retrovirus and is the causative agent of acquired immune deficiency syndrome (AIDS).
- It was first described in 1981, and the virus was isolated by the end of 1983.
- HIV-2 is recently described as a virus that is not distinguishable from AIDs, seen in Africans and a small number of European and South Americans.
- Blood tests for HIV-1 will not detect all HIV-2 cases. So please, for blood donation, advise both HIV-1 and HIV-2.
How will you discuss the microbiology of the Human immunodeficiency virus (HIV)?
- HIV is also called a human T-cell lymphotropic virus.
- HIV is also called the Human T-lymphocyte virus (HTLV).
- This virus measures 80 to 130 nm in diameter.
- This is a single-stranded RNA virus, icosahedral and enveloped.
- It contains a reverse transcriptase enzyme, which makes RNA into DNA.
- This is a member of the retrovirus family.
What are the Types of Human immune deficiency virus (HIV)?
- HTLV III or LAV (lymphadenopathy-associated virus).
- HIV type I. This is common in the USA and Western Europe.
- HIV type II. This is more common in West African countries.
What is the difference between the two types of Human Immunodeficiency Virus (HIV)?
| Property | HIV-I | HIV-II |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the viral genome of Human Immunodeficiency Virus (HIV)?
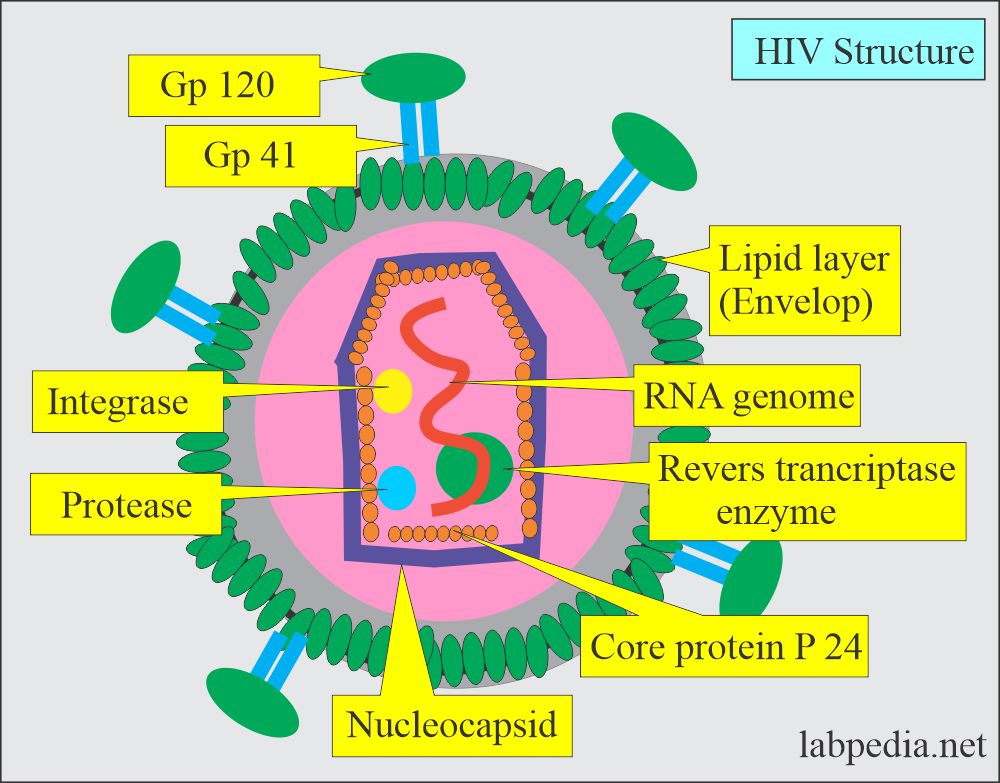
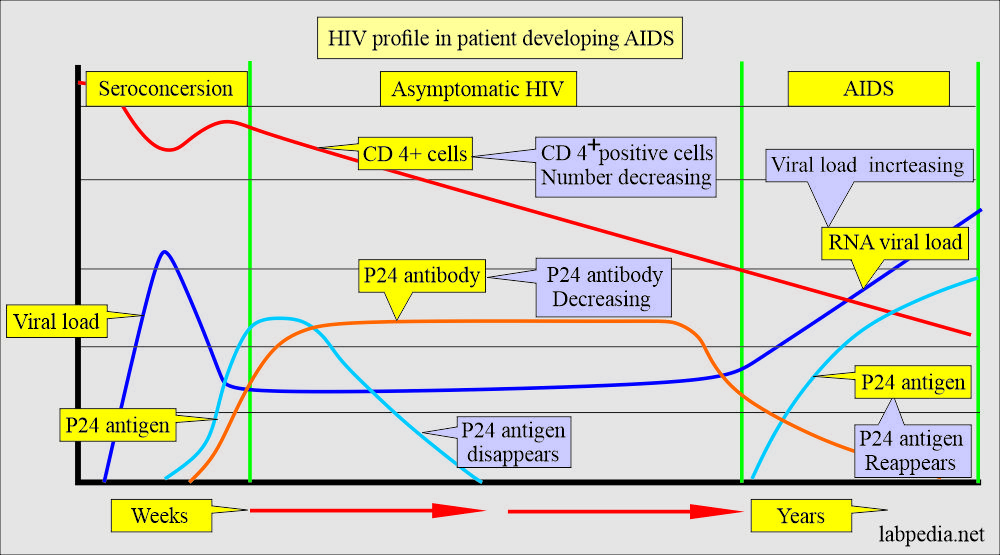
- Gag forms group-specific protein antigens, and these proteins are named p24 and p18.
- Env forms envelope proteins necessary for the interaction and presentation of target cells. These are gp120 and gp41.
- Pol forms polymerase, reverse transcriptase enzymes, and other enzymes like protease and integrase.
What is the mechanism of injury due to Human Immunodeficiency Virus (HIV)?
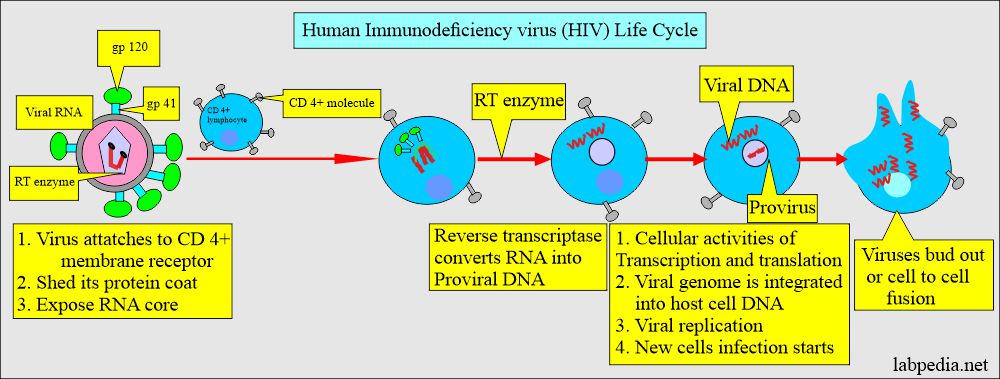
- HIV has receptors on the CD4+ cells, Helper cells, and macrophages.
- Virus gp 120 attaches to CD4+ molecules on cells in the lymphocytes.
- It is then internalized in the cell with the help of the reverse transcriptase enzyme.
- It changes RNA to DNA and integrates with the target cell DNA with the help of viral integrase.
- These are known as provirus.
- This will enter into the DNA of the host.
- Now, this may become latent.
- When the virus is assembled and leaves the cells, it buds out, incorporating the host cell membrane into its coat.
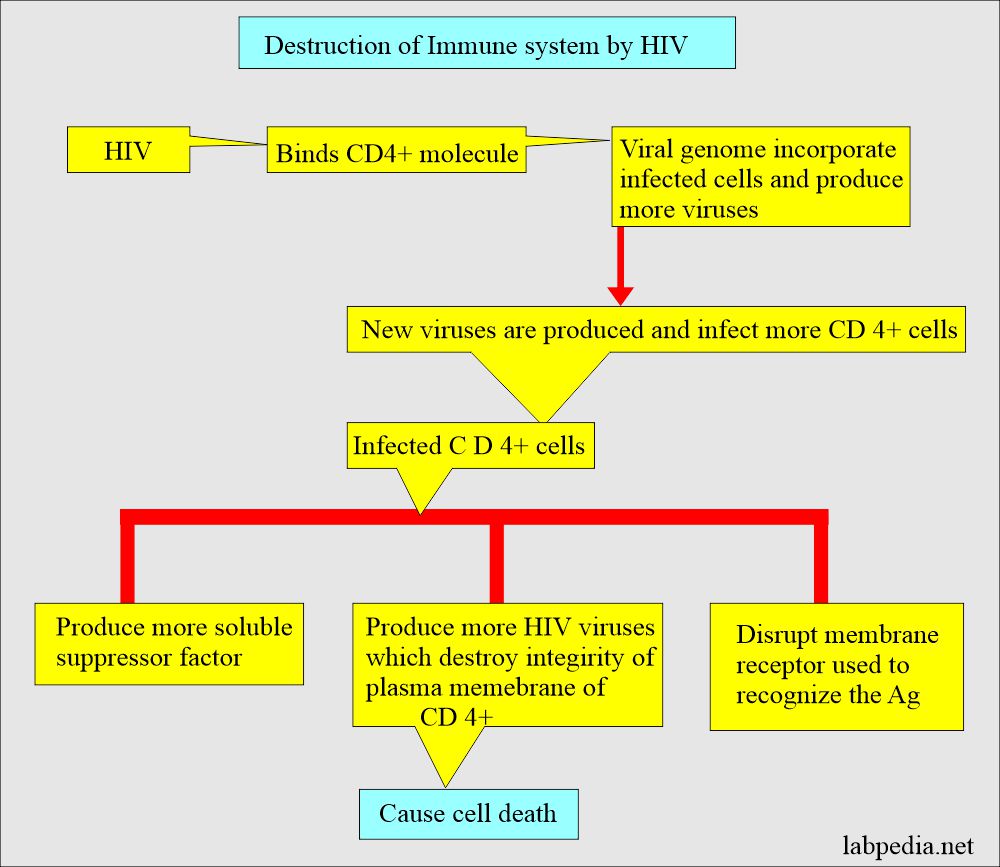
- HIV leads to the destruction of the host immune system, which can be summarized below:
- HIV destroys T-lymphocytes, mainly T lymphocytes, which are CD4-positive cells (T-helper cells).
- HIV damages the immune system and leads to acquired immune deficiency syndrome (AIDS).
- HIV infection may be present for as long as 10 years before the patients develop signs and symptoms or become AIDs patients.
How will you see Human Immunodeficiency Virus (HIV) infecting other cells on E/M?
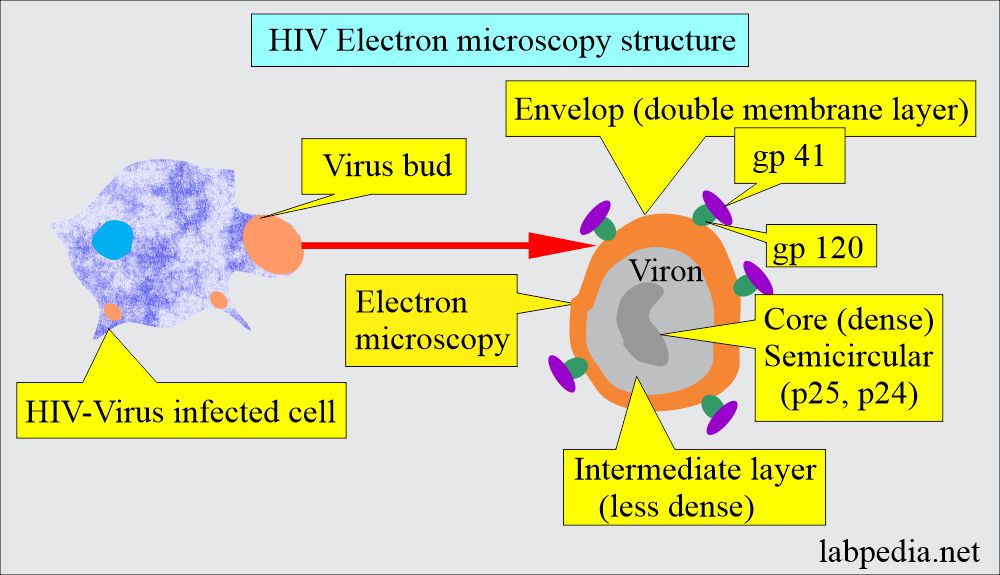
- Virus buds out of the cells and on electron microscopy show virus bud. This has a double-layer envelope, a dense core, and a less dense intermediate layer.
What is the Human Immunodeficiency Virus (HIV) mode of transmission?
Body fluids with high concentrations of Human Immunodeficiency Virus (HIV):
- Blood and contaminated blood products.
- Semen
- vaginal fluid
- breast milk (contaminated).
- other body fluids containing blood
- Tears.
- There is a transplacental spread.
- Infants exposed to the virus during gestation or delivery.
- 2.8% mode of transmission is not known in the USA.
- 50% are homosexual.
- Between men is 60%.
- Between men and women, it is 12%.
- 20% are I/V drug users.
- 20% are blood transfusions before 1985.
- 10% are heterosexual.
- Roughly 40 million people are living with HIV/AIDS,
- 37.1 million adults.
- 18.5 million women.
How will Human Immunodeficiency Virus (HIV) spread?
- The most common route is sexual:
- Oral sex.
- Anal sex.
- Vaginal sex.
- Another mode of spread is:
- Blood.
- Blood products.
- Perinatal exposure.
- In the USA, the mode of transmission:
- Homosexual/Bisexual 50%.
- I/V drug users 20%.
- Blood transfusion before 1985 was 20%.
- Heterosexual 10%.
- The dose of HIV is not exactly known, but it is estimated that 10 to 100 viruses may cause infection.
What are the High-risk patients?
- Homosexuals in males.
- Bisexual men and women with multiple partners.
- Intravenous drug abusers.
- Contaminated blood transfusion.
- Infants exposed during delivery to positive mothers
What is the dose of Human Immunodeficiency Virus (HIV) needed for infection?
- It is unknown, but a rough estimate is 10 to 100 viruses that may lead to infection.
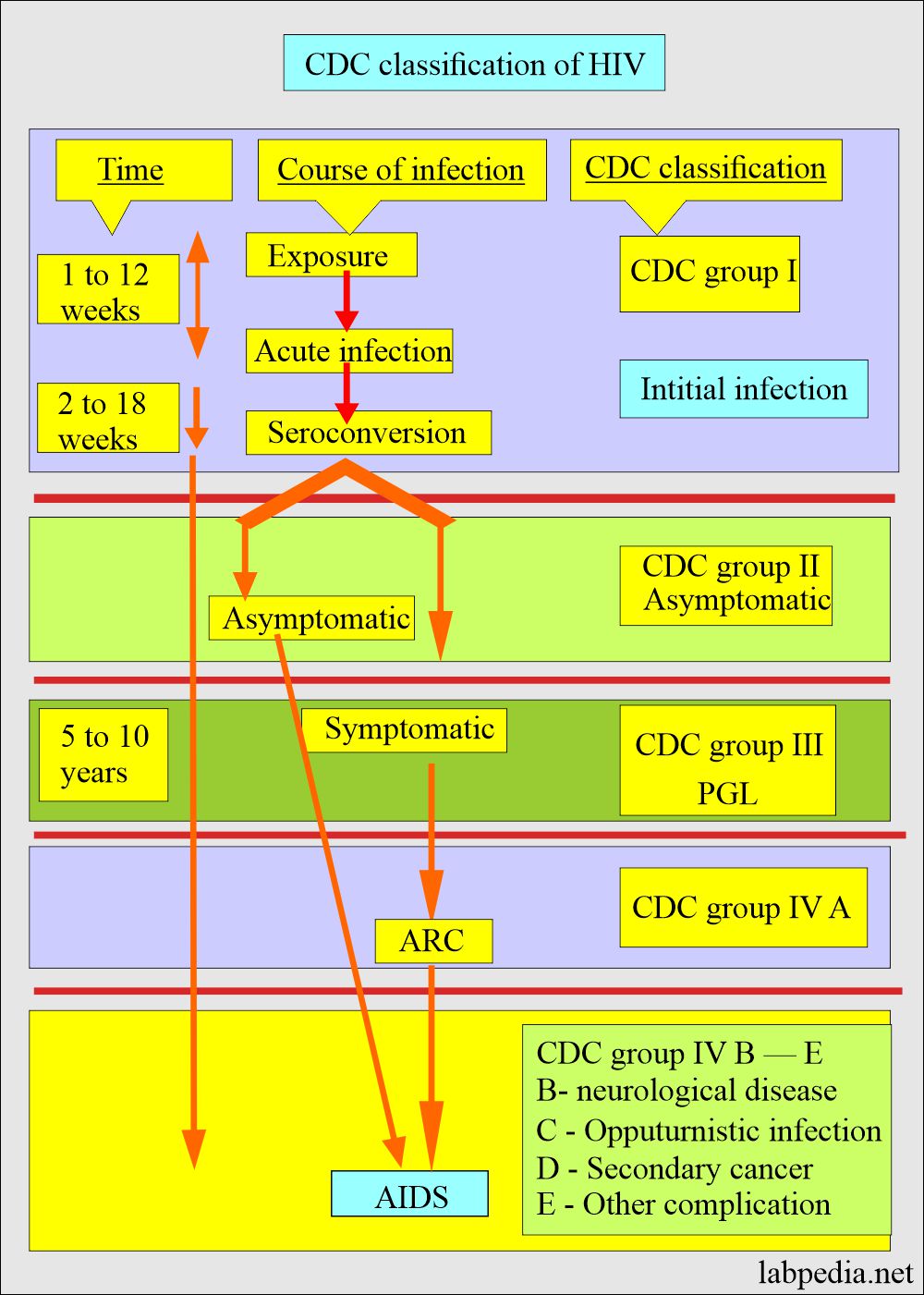
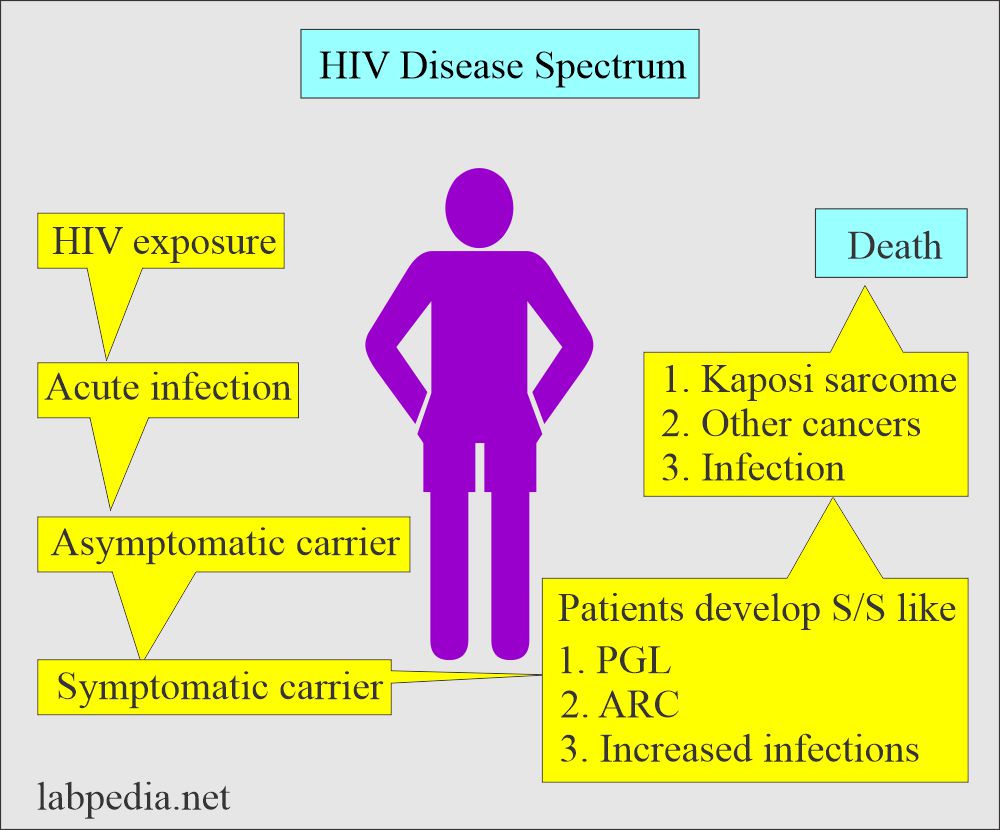
What are the stages of Human Immunodeficiency Virus (HIV) infection?
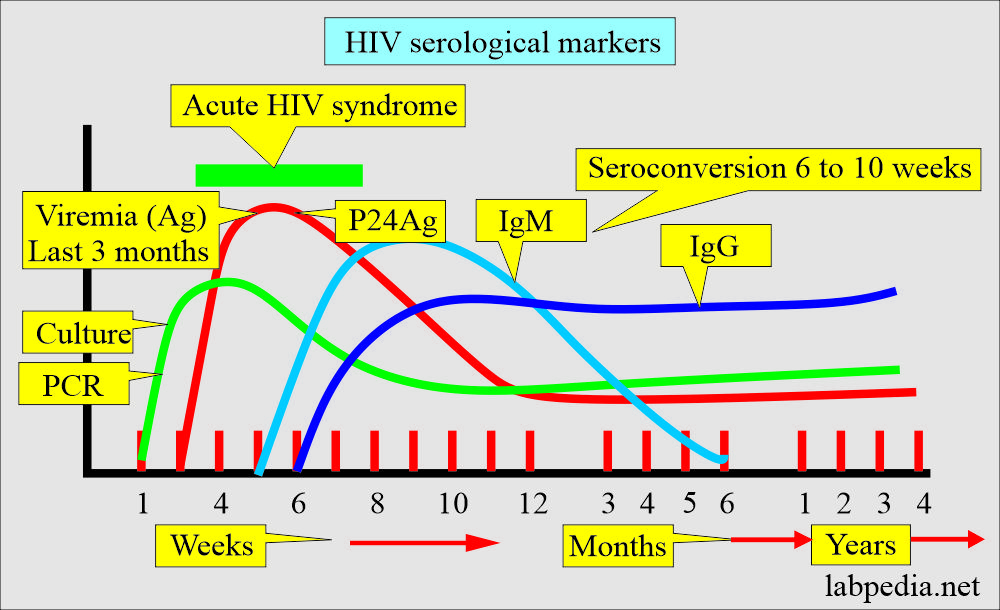
Stage 1: Acute infection:
- After 2 to 4 weeks, the infected patients will have early flu-like symptoms.
- These patients are very contagious. These patients may not come to know that they have an infection.
- You must advise the fourth-generation antibody/antigen test or nucleic test to diagnose these patients.
Stage 2: HIV inactive or dormant or clinical latency :
- This is the stage called asymptomatic HIV infection or chronic infection.
- This stage may last for a longer period or decades.
- These patients may still spread the disease to other people.
- The CD4+ cell number starts decreasing, and viral loads increase.
- Patients may start having symptoms, and the viral level is going up, and patients may go into stage III.
Stage 3: Acquired immune deficiency syndrome:
- This is the most severe phase of HIV infection.
- The immune system is severely damaged, and these patients are prone to get the opportunity for infection.
- Without treatment, these patients may live for about 3 years.
- CDC revised the Classification based on the number of CD4+ lymphocytes. With the decrease in CD4+ cells, the patient will end up with AIDS.
| CD4+ cells | CD4+ cells % | Clinical category A
|
Clinical category B
|
Clinical category C
|
| ≥ 500/ mL | > 29% | A1 | B1 | C1 |
| 200 to 400/ mL | 14 to 28% | A2 | B2 | C2 |
|
< 200/ mL Aids indicator |
>14% | A3 | B3 | C3 |
- A = ARC (Aids-related complex)
- B = Neurological disease.
- C 1 = opportunistic infection.
- C 2 = Secondary infection like candidiasis and H. Zoster.
- A 3, B 3, C 3 = Considered to have AIDS.
What are the common symptoms of Human Immunodeficiency Virus (HIV)?
- The incubation period is:
- 50% of the cases developing AIDs syndrome takes roughly 10 years.
- 20% are symptom-free for more than 10 years.
- 20% to 30% show a sign of infection.
- Initial stage shows:
- Headaches, diarrhea, sore throat, myalgia, and arthralgia.
- The patients will have weakness and weight loss.
- Fever and chills.
- Sweating.
- There is a macular rash.
- There are neurologic symptoms.
- Lymph nodes are swollen (lymphadenopathy).
- CD4+ cell number drops to <200 cells/cmm.
- These are highly infectious.
What will be the presentation of Human Immunodeficiency Virus (HIV) positive patients?
- Fatigue and night sweating.
- Persistent diarrhea.
- Weight loss.
- Frequent infections like Herpes and candidiasis.
- Candidiasis shows a thrush and vulvovaginal infection.
- HIV infection may lead to Kaposi’s sarcoma, B- cell lymphoma, and anal carcinoma.
What are the symptoms when you suspect Human Immunodeficiency Virus (HIV)?
- Two or more of the following signs and symptoms are needed to suspect HIV when these are persistent for more than 3 months:
- Pyrexia is more than 38 °C.
- History of chronic diarrhea.
- Weight loss of more than 10%.
- Mailase and lethargy.
- Persistent generalized lymphadenopathy (PGL).
- Night sweating.
- Oral candidiasis.
- Hairy leukoplakia.
- Herpes Zoster infection.
What are AIDS-related diseases?
| Etiology | Disease |
| Tumors | Kaposi’s sarcoma |
| Lymphomas | |
| Cancers | |
| Cervical cancer | |
| Bacterial infections | Mycobacterium tuberculosis |
| Salmonellosis | |
| Pneumonia | |
| Atypical mycobacterial infection | |
| Viral diseases | Herpes simplex |
| Cytomegaloviral pneumonia | |
| Cytomegaloviral retinitis | |
| Encephalopathy | |
| Dementia | |
| Diarrhea | |
| Fungal diseases | Candidiasis |
| Cryptococcosis | |
| Parasitic diseases | Pneumocystis carinii |
| Toxoplasmosis | |
| Cryptosporidiosis |
How long does Human Immunodeficiency Virus (HIV) live outside the body?
- HIV does not survive outside the body, making the possibility of environmental transmission remote.
- CDC studies have shown that drying even these high concentrations of HIV reduces the amount of infectious virus by 90 to 99% within several hours.
- HIV is unable to reproduce outside its living host. Therefore, it does not spread or maintain infectiousness outside its host.
How many Health care workers are at risk?
- Although HIV transmission is possible in healthcare settings, it is extremely rare.
- Careful practice of infection control procedures is necessary.
- Protects patients and healthcare providers from possible HIV transmission in medical and dental offices and hospitals.
How will you diagnose Human Immunodeficiency Virus (HIV)?
- Screening test.
- This test detects antibodies. These are not confirmatory tests. These have to be confirmed by ELISA.
- These tests are done in blood banking to screen donors.
- This can also be done to screen blood products.
- ELISA
- This test is more specific than the screening antibody test.
- These tests detect viral antibodies and not antigens.
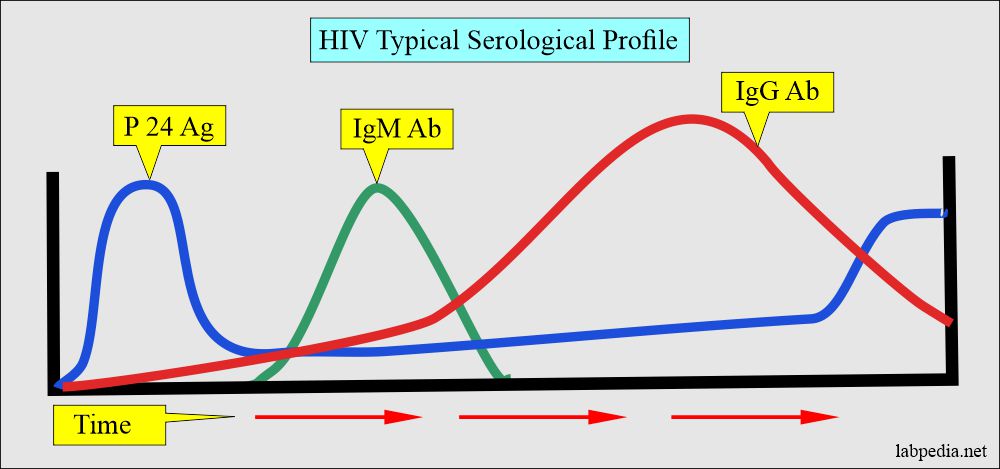
- There is a window period in which the patient will be negative before seroconversion for the test to become positive.
- It is used for clinical diagnosis, blood screening, and blood products.
- This cannot detect HIV infection in the early phase because there is an interval of 2 to 12 weeks, which may even be 6 months.
- The person who is infected with HIV becomes seropositive. This time period is called the window period.
- This is positive in 99% of the cases of patients who have had an infection of HIV for the last 12 weeks or more.
- Oral fluid:
- Oral fluid for the antibody to HIV is available instead of serum or plasma.
- This is a simple, non-invasive, and safe method.
- This is easier for the population screening and user-friendly.
- This portable method can identify more infected people with the goal of early detection, treatment, and prevention.
- This method will decrease the transmission of the disease in the population.
- Western blot:
- It is a confirmatory test.
- This test is done to validate the reactive ELIZA.
- The p24 antigen:
- P24 antigen capture assay may detect the patient’s peripheral blood.
- This may be found as an antigen or antibody to p24.
- p24 antigen can be used to find the neonatal HIV infection; this detects before there is seroconversion and find the progress of AIDS.
- HIV in the urine.
- This test was approved in 1996 by the USA Food and Drug Administration.
- In 1998, a license was given for the HIV 1- antibody.
- This is useful when there is difficulty with venipuncture.
- This is easier, more convenient, safer, and cheaper than the serum test.
- HIV viral load.
How will you interpret serologic tests for Human Immunodeficiency Virus (HIV)?
- Serologic antibody test, when positive, should be repeated by the ELISA.
- When ELISA is positive, confirm by the western blot or by immunofluorescence assay (IFA).
- Viral RNA may do to confirm HIV.
- Repeat the test in positive ELISA and negative western blot or IFA after 3 to 6 months.
- The patient with positive ELISA does not have AIDS until the patients develop signs and symptoms of diminished immunity.
- Rarely false-positive results may occur.
- HIV RNA antigens may be detected to confirm the diagnosis.
- p24 antigen (protein p24) may be detectable as early as 2 to 4 weeks after infection.
- Recently, oral fluids have been taken to detect antibodies against HIV.
- Urine may be tested for the HIV antibody.
What are the False-positive tests for Human Immunodeficiency Virus (HIV)?
- These are seen in patients with autoimmune diseases.
- In patients with:
- Lymphoproliferative diseases.
- Lymphoma.
- Leukemias.
- In patients with syphilis.
What are False-negative tests for Human Immunodeficiency Virus (HIV)?
- These are seen in the early stage of infection.
- Or in the end stage of HIV infection.
What are the various serological markers for HIV?
| Test | Detection | Purpose of the test |
|---|---|---|
| ELISA | Ab to HIV | Screening test |
| Western blot | Ab to HIV | confirmatory test |
| P24 Ag | HIV-1 core protein | support western blot |
| Urine for HIV | Ab to HIV | screening test |
| HIV load | HIV- RNA | marker for diagnosis and AIDS |
| Home Screening | Ab to HIV | Screening test |
| oral mucosa sample | Ab to HIV | Screening test |
How will you treat Human Immunodeficiency Virus (HIV)?
What are the recommendations for antiviral treatments?
| CD4+ count | HIV viral load (copies/mL) | Treatment |
|---|---|---|
| <350/cmm | <5000 | Treatment recommended |
| 5000 to 30,000 | Treatment recommended | |
| >30,000 | Treatment recommended | |
| 350 to 500/cmm | <5000 | Consider treatment |
| 5000 to 30,000 | Treatment recommended | |
| >30,000 | Treatment recommended | |
| >500/cmm | <5000 | Defer treatment |
| 5000 to 30,000 | Consider treatment | |
| >30,000 | Treatment recommended |
- Antiviral therapy like zidovudine (AZT), Zalcitabine (ddC), and Lamivudine (3TC).
- Treatment for opportunistic infection is needed.
How will you prevent Human Immunodeficiency Virus (HIV)?
- Avoid contact with infected blood.
- Avoid contact with infected blood products and body secretion.
- Compulsory screening of the donor’s blood.
- Educate about safe sex.