Helicobacter Pylori, H. Pylori, Presentations and Diagnosis
Helicobacter Pylori
What sample is needed for Helicobacter Pylori?
- It is done on the patient’s serum using techniques like ELISA.
- H. pylori can be diagnosed with a duodenal biopsy.
- H. pylori sample can be cultured.
- Various samples available are:
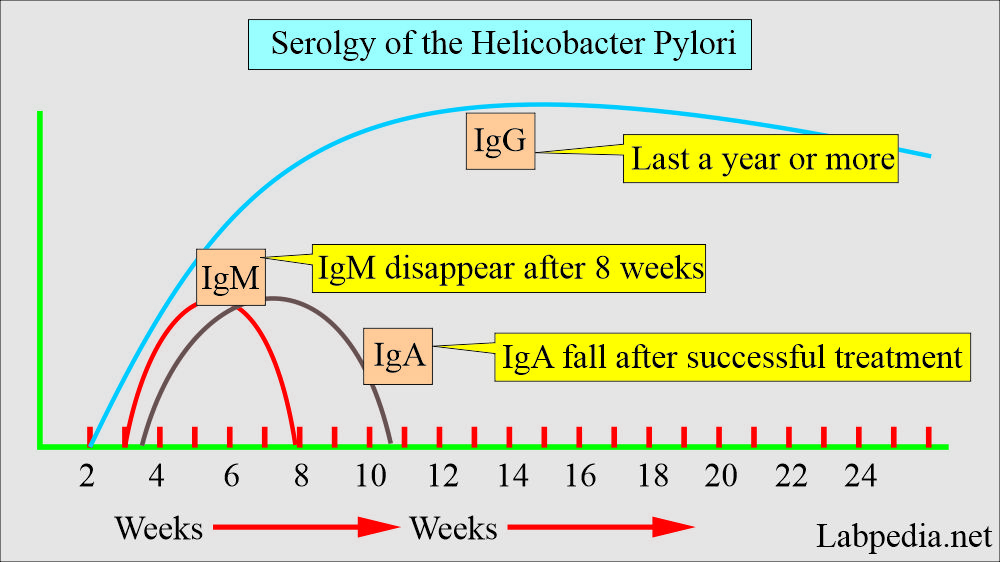
- Serum, for specific antibodies. This is a non-invasive method and easy to perform. This antibody appears after 2 months of infection and remains elevated for over a year after the treatment.
- Initially, IgM is formed, followed by IgG and IgA. These are found in the blood and the mucosa and are high titer in chronic cases.
- Types of antibodies:
- IgG – anti-H. pylori
- IgA – anti- H. pylori.
- IgM – anti-H. pylori
- Biopsy:
- These bacteria can be seen in the gastric mucosal biopsy. (Giemsa stain shows these bacteria). This is a more specific and confirmatory test.
- Culture:
- A sample of mucus can be obtained through a gastroscope for culture.
- Rapid urease test:
- For this test, the sample can be gastric mucosa or gastric mucus.
- Breath test:
- This detects gastric urease and measures CO2 in the breath. The patient needs to be at rest for this test.
- The stool examination:
- The stool is examined for the H. Pylori antigen. Try to do the test on the fresh sample.
What are the precaxutions taken for Helicobacter Pylori?
- For culture, stop antibiotics, antacids, and bismuth therapy 5 to 14 days before the procedure.
What are the Indications for Helicobacter Pylori?
- These tests are used to diagnose H. Pylori infection.
- In the patient with chronic gastric or duodenal ulcers.
How will you define Helicobacter Pylori?
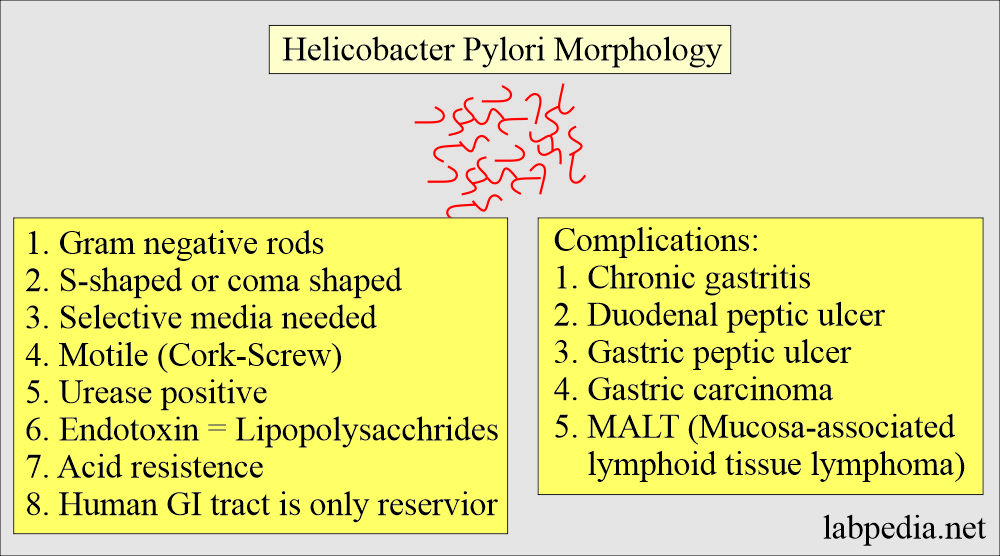
- Helicobacter Pylori was formerly called Campylobacter pylori or pyloridis.
- It is S-shaled, curved, “gull-winged” like Campylobacter.
- It is a gram-negative bacillus found in the mucus covering the gastric mucosa.
- It lies next to gastric lining epithelial cells and gastric pits.
Discuss the Helicobacter Pylori Bacteriology?
- This is a small gram-negative, spiral rod bacillus discovered in 1982.
- Helicobacter pylori (H.pylori) was known as Campylobacter pylori.
- These are strongly urease positive.
- Gram-negative spiral-shaped rods.
- It has a common feature with Campylobacter.
- It has multiple flagella at one pole and is actively motile.
- H. Pylori growth takes 3 to 6 days when grown at 37 °C in a microaerophilic atmosphere.
- Culture media used are:
- Skirrow medium.
- Can add vancomycin, polymyxin B, and trimethoprim.
- Chocolate medium and selective media with antibiotics.
- The colonies are translucent and measure 1 to 2 mm in diameter.
- These colonies have characteristic morphology.
- H. pylori is oxidase-positive and catalase-positive.
- Bacteria are motile and strong producers of urease.
What are the complications and associations of Helicobacter Pylori infection?
- This bacteria causes gastritis and gastric and duodenal ulcers.
- This may even cause an oesophageal ulcer.
- This bacteria is also associated with gastric carcinoma.
- H. pylori is lying in the mucous of the gastric mucosa.
- This bacteria is seen in various conditions:
- It is found in acute and chronic gastritis in the stomach antrum and is positive in 90% of patients with duodenal ulcers.
- 95% to 98% of the patients with a duodenal ulcer (another reference says 100%).
- 70% (70% to 75%) positive in gastric ulcers.
- This is also seen in gastric ulcers in 60% to 70% of patients.
- 20% to 25% of patients with gastric cancer are positive for H.Pylori.
- 10% of healthy people in the younger age group, around 30 years, are positive for H.pylori.
- It is positive in 50% of the cases with non-ulcer dyspepsia.
- The positivity of H. pylori increases with increasing age.
- It is found in acute and chronic gastritis in the stomach antrum and is positive in 90% of patients with duodenal ulcers.
- Gastric colonization by H. pylori increases with age.
- Most of the people with H. Pylori colonization are asymptomatic.
- Helicobacter pylori antibodies are found in 20% to 25% of healthy US citizens.
- It shows that Helicobacter Pylori infection is subclinical.
How will you discuss the pathophysiology of Helicobacter Pylori infection?
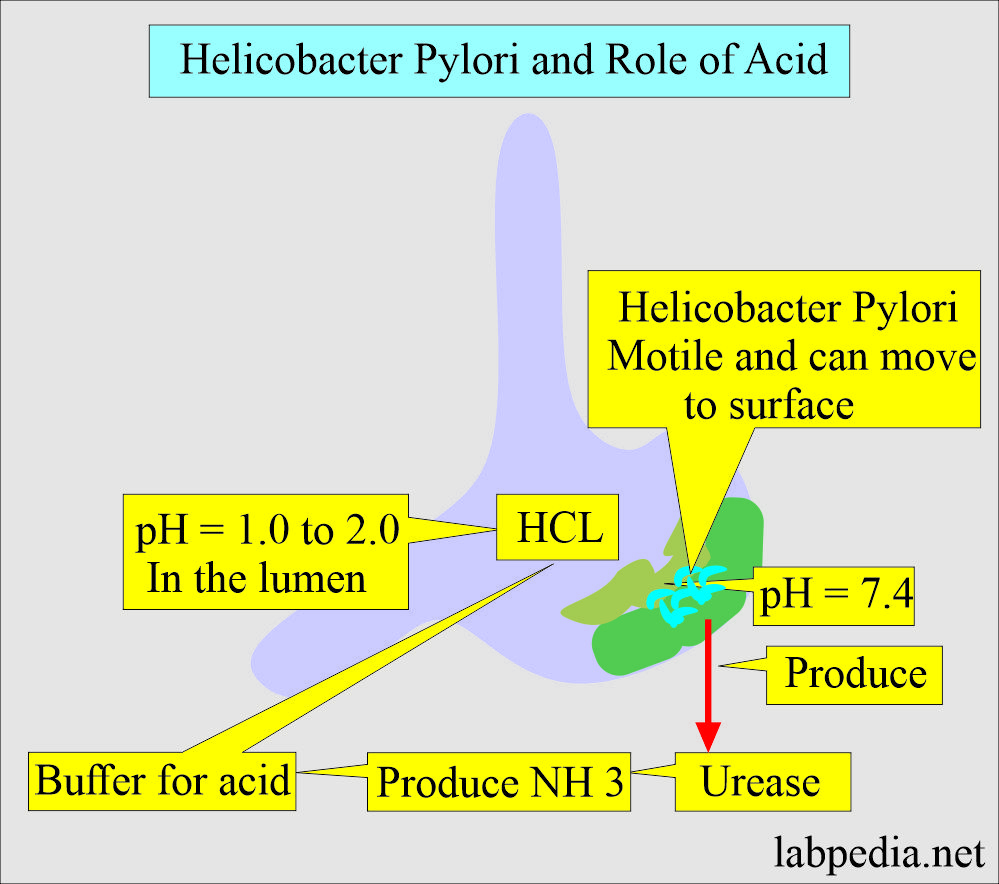
- H. Pylori growth has an optimum pH of 6.0 to 7.0 and would be killed, or it can not grow at the pH within the gastric lumen.
- Gastric mucus is impermeable to acid and acts as a buffer system.
- H. Pylori produces a protease enzyme that modifies gastric mucus and reduces the acid’s ability to diffuse through it.
- H. Pylori produces urease activity, leading to NH3 production and further acid buffering.
- H. Pylori was given to volunteers; later on, it was found that those people developed gastritis and hypochlorhydria.
- When antibiotics were given to these patients, they found improvement in gastritis and duodenal ulcers.
- Toxins and lipopolysaccharides may damage the mucosal cells, while NH3 can cause direct damage to the epithelial cells.
- Microscopic findings are:
- Gastritis is characterized by the infiltration of chronic and acute inflammatory cells.
- Neutrophils and mononuclear phagocytic cells are seen within the epithelium and lamina propria.
- There are vacuoles in the epithelial cells.
- The epithelium is damaged.
- There is glandular atrophy.
How will you discuss the pathogenesis of Ulcer due to Helicobacter Pylori?
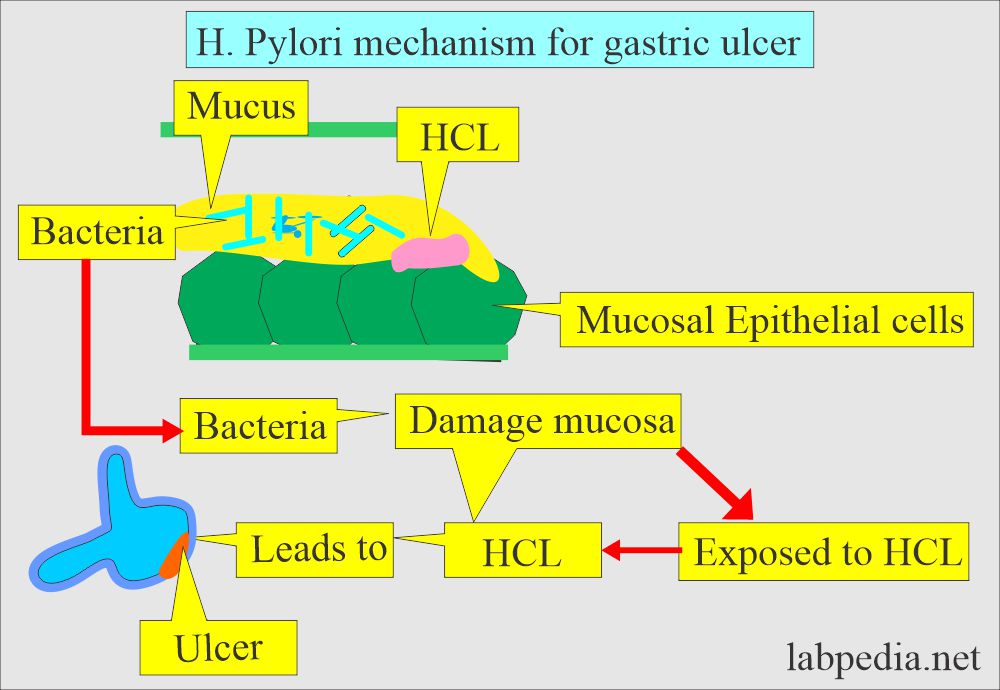
- These bacteria enter the body and damage the lining of the stomach mucosa.
- The stomach mucus protects the mucosa from acid (HCl).
- When these bacteria cause damage to the mucosa, then acid can get through the lining, leading to ulcer formation.
- These bacteria may be dormant, and the patient may be asymptomatic.
What is the mode of the spread of Helicobacter Pylori?
- Its transmission is from person to person.
- These bacteria can enter the body from:
- Food.
- Water.
- Utensils.
- Saliva and body fluids through close contact.
How will you discuss the clinical presentation of Helicobacter Pylori infection?
- The incidence of H. pylori is age-related.
| Age of the group | Positive antibodies |
|
|
|
|
|
|
|
|
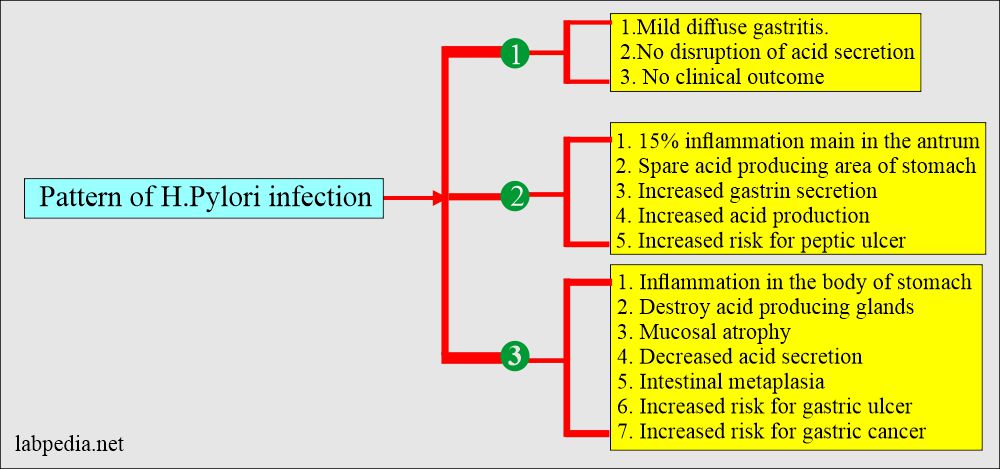
- H. pylori is associated to a lesser degree with focal areas of gastritis in the body of the stomach.
- In the case of acute infection:
- There may be nausea and abdominal pain.
- These S/S may last for many days.
- Histologically, there is gastritis with infiltration by neutrophils.
- The above stage may go into a chronic stage.
- There is diffuse mucosal involvement (chronic gastritis).
- There is the infiltration of neutrophils and lymphocytes.
- Chronic H. pylori infection with gastritis may be seen in 30% to 50% of the patients, which may be asymptomatic.
- Chronic or recurrent duodenal ulcer is associated with excessive acid production and Helicobacter Pylori presence.
- In the case of Zollinger-Ellison syndrome duodenal ulcers, H. pylori infection is almost negative.
How will you discuss the pattern of H. pylori infection?
What is the outcome of Chronic H. Pylori infection?
- 10% develop a duodenal or gastric ulcer.
- 0.1 to 3% develop gastric cancer.
- 0.01% develop B-lymphocytes lymphoma called MALT, mucosa-associated lymphoid tissue lymphoma.
What is the normal value of Helicobacter Pylori?
H. pylori antibody
- The negative antibody by Eliza indicates that there is no infection.
- The positive antibody test indicates the IgG-H-Pylori antibody in serum.
How will you diagnose Helicobacter Pylori?
- Culture of the tissue:
- The gold standard for diagnosis is the endoscopic gastric mucosa biopsy for culture.
- This biopsy is placed in the isotonic saline of 2 to 3 mL.
- It is plated on enriched media (chocolate agar or selective media Skirrow’s).
- It is then incubated for 5 to 7 days at 37 °C.
- 75% of cases are positive for culture.
- If you do Giemsa stain on the biopsy, will detect 90% of the cases.
- Warthin-Starry silver stain has better results than Grams and Giemsa stain.
- Culture takes several weeks before the final result comes.
- Rapid Urease test:
- This bacteria produces a urease enzyme that acts on urea. This makes the basis for other tests. This can be done by:
- Gastric mucosa tissue.
- The gastric mucosa is placed on the paper, and its color will change.
- The special tablet is placed in the test tube, and gastric mucosa is added.
- This bacteria produces a urease enzyme that acts on urea. This makes the basis for other tests. This can be done by:
- The breath test:
- It is noninvasive because H. pylori can produce CO2 by the urease enzyme acting on urea.
- The patient is given radiolabel Carbon-13 or carbon-14. It is given orally.
- Then, expired air is tested for radioactivity 20 to 120 minutes later.
- This test sensitivity is >95%, and specificity is also >95%.
- This test is considered the gold standard test, not the culture.
- Serology :
- These tests of the Helicobacter Pylori (antibody test) are:
- The anti-IgG H. pylori are most commonly used.
- Its level rises after two months of infection and remains raised for a year after the treatment.
- The anti-IgM rises first in about 3 to 4 weeks after the infection.
- It disappears in 2 to 3 months after the treatment.
- IgM and IgA antibody levels fall after the treatment in about 4 weeks.
- While IgG level is not affected by the treatment.
- By ELIZA: Antibodies are positive in almost 100% of the duodenal ulcer.
- 80% in gastric ulcers.
- Positivity increases with increasing age.
- Positive results do not confirm the diagnosis, but negative results rule out H. pylori infection.
- H. pylori antigen:
- It is done on a fresh stool.
What are the causes of a raised level of a breath test for H. pylori?
- Acute and chronic gastritis.
- Gastric ulcer.
- Recurrent duodenal ulcer.
- Carcinoma of the stomach.
What is the outcome of H. Pylori infection?
| Outcome | Disease |
|---|---|
|
|
|
|
|
|
|
|
|
|
What are the common tests for the diagnosis of H. Pylori infection?
| Diagnostic test | Interpretations |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you treat Helicobacter Pylori?
- Usually, a gastroenterologist advises the tripple regime.
- Most clinicians advised Amoxicillin, clarithromycin, and PPI.
- Some advised clarithromycin, metronidazole, and tinidazole.
- In addition, proton pump inhibitors and H2 blockers are advised.
- Avoid non-steroidal anti-inflammatory drugs.
Questions and answers:
Question 1: What is the outcome of H. Pylori infection?
Question 2: What are the bases of the breath test?