March 6, 2024
Glucose-6-phosphate dehydrogenase deficiency (G6PD)
What sample is needed for Glucose-6-phosphate Dehydrogenase deficiency (G6PD)?
- Take blood in EDTA or heparin.
- Avoid hemolysis.
- Don’t use oxalate or fluoride in the blood.
- It is stable for over 20 days at 4 °C and 5 days at 25 °C.
- Collect blood in a colored bottle.
What are the Indications for Glucose-6-phosphate Dehydrogenase (G6PD) deficiency?
- This test is advised to rule out the deficiency of G6PD in a patient who develops hemolytic anemia after taking drugs or food.
What are the precautions needed for Glucose-6-phosphate dehydrogenase deficiency (G6PD)?
- Raised levels of reticulocytes may give false high G6PD.
- G6PD may be normal after the hemolytic episode for the first 6 to 8 weeks.
- Repeat the test when the anemia is recovered.
How will you define Glucose-6-phosphate dehydrogenase deficiency (G6PD)?
- G6PD is a sex-linked (X-linked) disorder. This is a recessive trait carried on the female (X) chromosome.
- The chromosome-affected gene is Xq28.
- It consists of 515 amino acids and a molecular weight of 59 kDa.
- Affected males inherit this gene from their mothers, who are usually asymptomatic, and the disease is severe in males (XY).
- The disease is very severe if the female has both X genes defective.
- So, females act as carriers of this disease with one defective X chromosome.
Glucose-6-phosphate Dehydrogenase deficiency (G6PD): G-6-PD role in the stability of the RBC membrane
What is the distribution of Glucose-6-phosphate dehydrogenase deficiency (G6PD)?
- This is common in some ethnic groups of African-American men. About 11% of African-American males are affected.
- To a lesser extent, people whose ancestors came from Mediterranean countries like Italy, Greece, or Turkey.
- It is also seen in some areas of India.
- It is also seen in the Jewish population.
- The condition is commonly asymptomatic, but there may be acute hemolysis crises after taking some drugs, ingesting fava beans, and viral or bacterial infections.
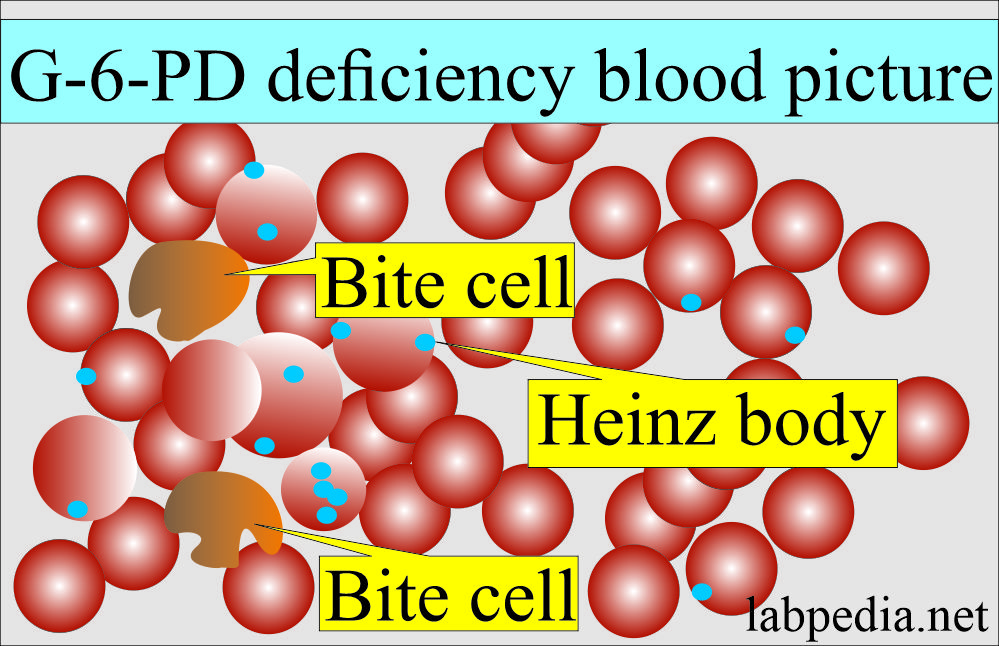
- Hemolytic crises are associated with the formation of Heinz bodies in Peripheral blood RBCs.
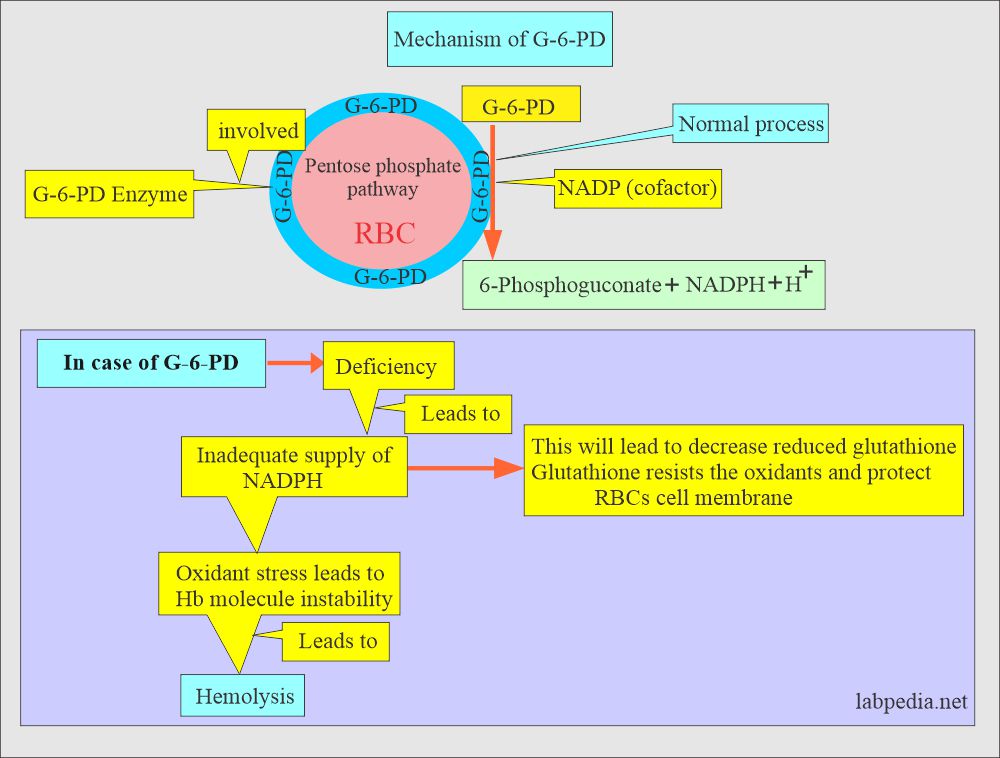
How will you discuss the Pathogenesis of Glucose-6-phosphate dehydrogenase enzyme deficiency?
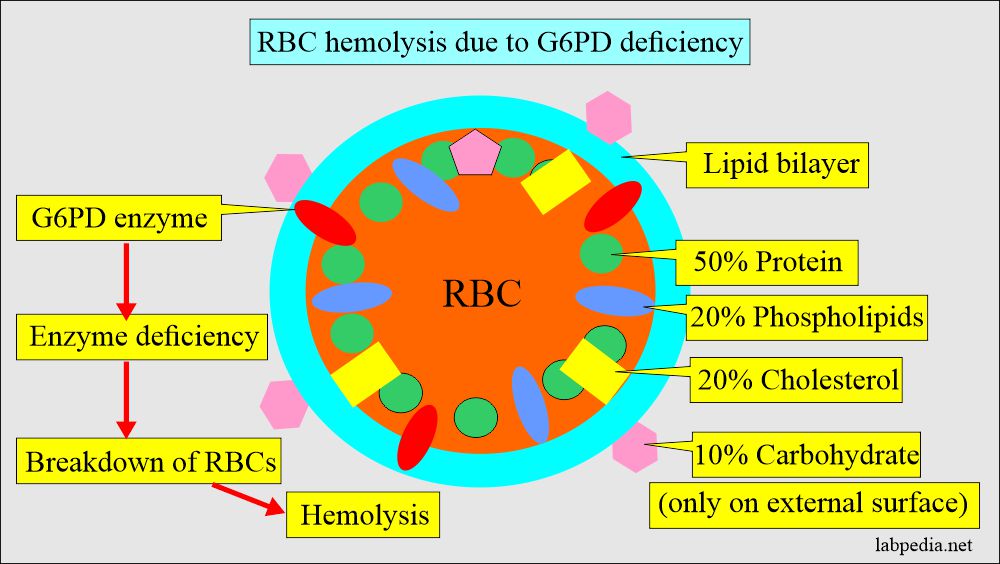
- An enzyme deficiency was detected in the RBC.
- Screening should be done several days after the crisis when the patient is no longer jaundiced.
- This is an RBC G6PD enzyme defect. Most patients are asymptomatic with normal Hb and blood smear.
- Patients are susceptible to oxidative crises precipitated by drugs (e.g., Dapsones, sulphonamides, antimalarial, aspirin, phenacetin, and nitrofurantoin) and exposure to fava beans.
- G6PD deficiency causes the precipitation of hemoglobin and cellular membrane changes in RBCs, which may lead to hemolysis.
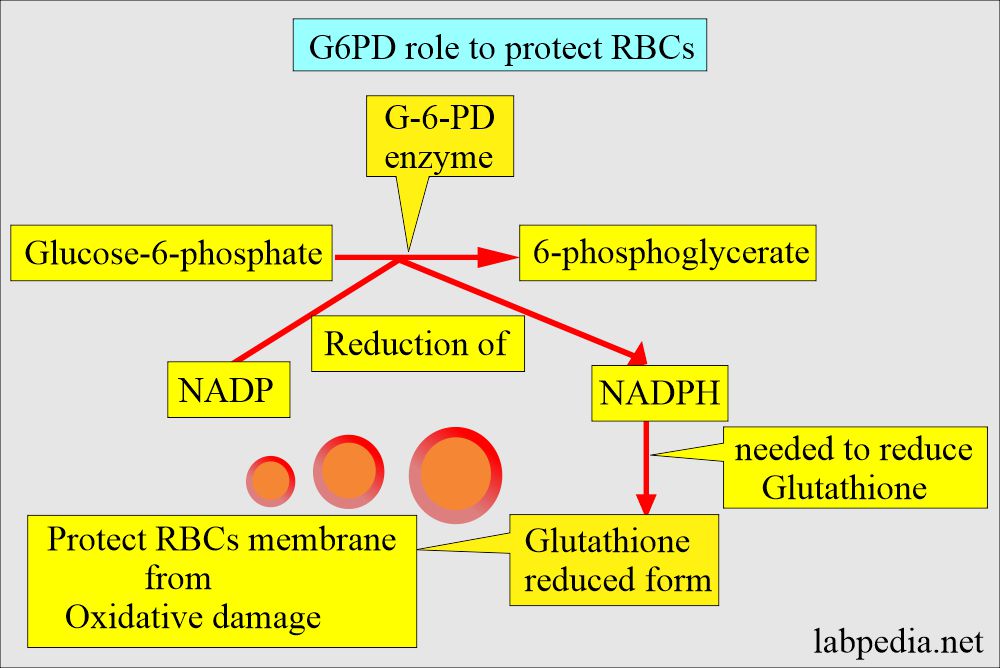
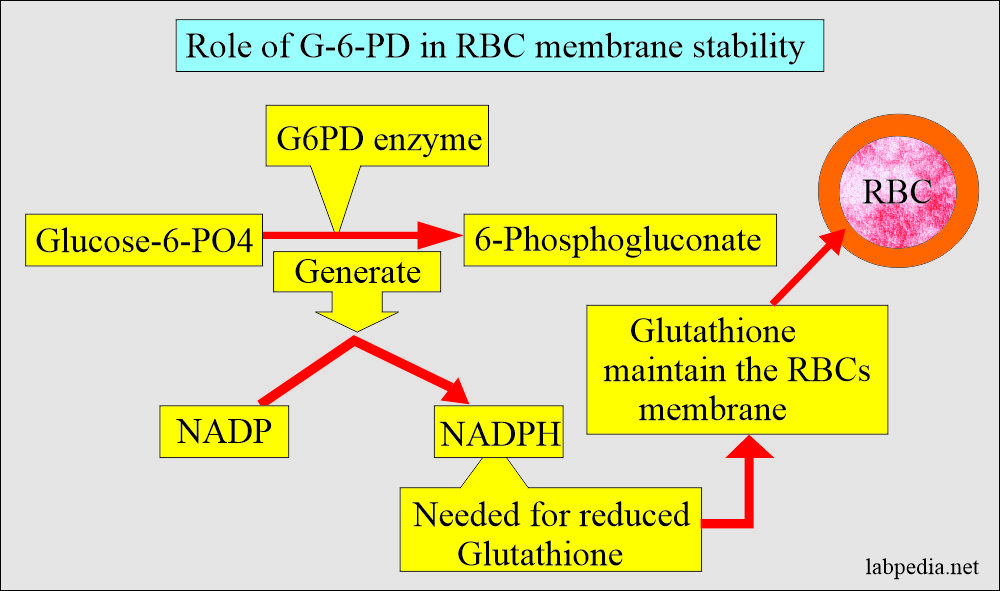
What is the role of the Glucose-6-phosphate Dehydrogenase (G6PD) enzyme?
- This enzyme is needed for the integrity of the Red blood cell membrane.
- 30% or less of the deficiency of the G6PD enzyme leads to hemolysis when exposed to some drugs, like antimalarial (primaquine) medicines.
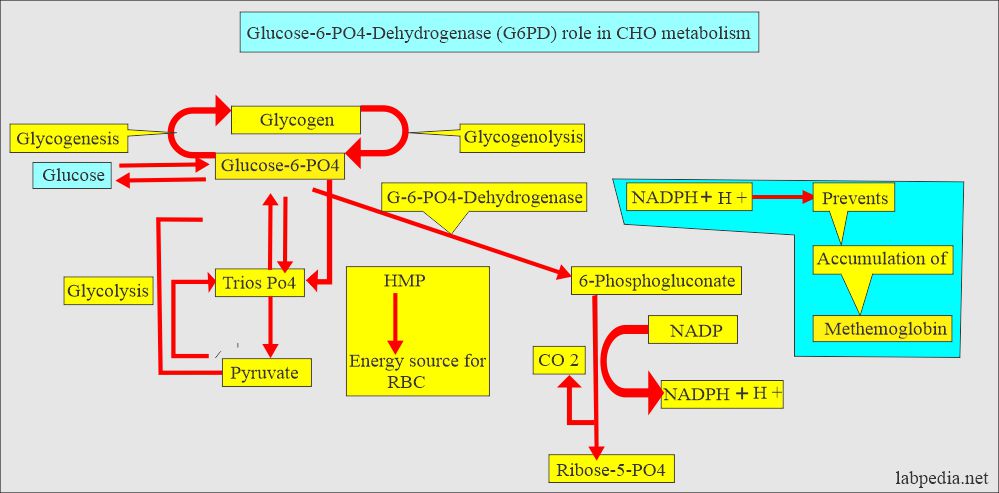
- G6PD is an enzyme used in glucose metabolism.
- The generated NADPH is a necessary ingredient for the enzyme system in the red blood cells to prevent methemoglobin formation.
How will you Classify Glucose-6-phosphate Dehydrogenase deficiency (G6PD)?
- African Americans, where 10% to 15 % of this population, are affected.
- The Mediterranean is more common in Iraqis, Kurds, Sephardic Jews, and Lebanese. This is less common in Greeks, Turks, and North Africans.
- The MAHIDOL variant is common in southeast Asia, where 22% of the population are males.
Another classification of Glucose-6-phosphate Dehydrogenase (G6PD):
- It divides G6PD deficiency into 5 classes. Classes 2 and 3 represent 90% of the cases.
- Class 1: <5% of the normal RBC enzyme activity.
- It is rare, chronic, congenital nonspherocytic hemolytic anemia initiated by oxidant medications.
- The fever may initiate it.
- There is no improvement by splenectomy.
- Class 2: <10% of normal RBC enzyme activity.
- It is seen in 90% of the cases.
- There are acute episodic hemolytic crises induced by oxidant drugs like sulfonamide, primaquine, and acetanilid.
- This reaction may take place by acidosis.
- There is no improvement by splenectomy.
- Class 3: 10% to 60% of normal RBC enzyme activity,
- It is seen in 90% of the cases.
- The hemolytic episode in people without the known hematological disease.
- Oxidant drugs or infection (hepatitis or pneumonia) induce acute self-limiting hemolysis episodes lasting 2 to 3 days.
- It is also seen in hepatic coma, myocardial infarction, hyperthyroidism, chronic blood loss, and megaloblastic anemia.
- It induces hemolytic crises, which are self-limiting episodes.
- Class 4 and 5: These do not show any clinical findings.
- Class 1: <5% of the normal RBC enzyme activity.
What are the variants of Glucose-6-phosphate Dehydrogenase (G6PD) deficiency?
- These are based on electrophoretic patterns and kinetic criteria:
- G6PD-A is common in blacks.
- G6PD – Mediterranean is common in Kurds, Iraqis, Lebanese, and Sephardic Jews and less common in Greeks, Turks, Italians, Portuguese, Ashkenazi Jews, North Africans, and Spaniards.
- G6PD- Mahidol is common in Southeast Asians.
What is the clinical presentation of Glucose-6-phosphate Dehydrogenase (G6PD) Deficiency?
- These patients may be asymptomatic.
- Acute hemolytic anemia due to some drugs, foods, and infection.
- The anemia may be self-limiting as there is replacement by the new RBC formation.
- There may be hemoglobinuria.
- There may be neonatal jaundice.
- Deficiency may cause hemolytic disease in newborns in Asia and the Mediterranean.
- In the newborn G6PD deficiency:
- Newborn develops neonatal jaundice after the first 24 hours in contrast to the erythroblastosis fetalis.
- Raised serum bilirubin levels peak on the 3rd to 5th day.
- Serum bilirubin level may reach >20 mg/dL.
- In Asian and Mediterranean newborns, neonatal jaundice and kernicterus are more common.
What is the normal value of Glucose-6-phosphate Dehydrogenase (G6PD)?
- G6PD screening test = G6PD detected.
- In the deficiency of G6PD screening test is negative
- Adult = 8.6 to 18.6 U/g Hb.
- Children = 6.4 to15.6 U/g Hb.
- Conversion of U/g Hb to U/mL of RBC:
- U/g Hb X0.34 = U/mL of RBCs.
How will you diagnose Glucose-6-phosphate dehydrogenase (G-6-PD)?
- G6PD deficiency can be diagnosed by :
- Screening test by direct enzyme assay on red blood cells.
- During crises, peripheral blood smear shows fragmented RBCs like bite and blister cells.
- Heinz bodies may be seen in the reticulocytes in the case of splenectomy.
- Heinz bodies are oxidized denatured hemoglobin.
- Heinz’s body can be seen by the supravital stain (new methylene blue) in the early stage of hemolysis.
- Quantitative spectrophotometry.
- The rapid fluorescent spot test detects the generation of NADPH from NADP. It is read under ultraviolet light.
- Recently DNA analysis has been introduced to diagnose variation in G6PD.
- After a single dose of primaquine in adults, Intravascular hemolysis takes place and shows the following lab findings:
- Hct is decreased. It starts in 2 to 4 days, and the peak is 8 to 12 days.
- Heinz’s body is seen on the peripheral blood smear.
- Increased serum bilirubin level was seen in the first few days of hemolysis.
- Reticulocytosis starts at about the 5th day of hemolysis, and the maximum level is at 10 to 20 days.
- Hemolysis will subside spontaneously even if primaquine tablets are continued.
- Diagnosis is confirmed by the RBC assay of G6PD (by fluorescence technique).
What conditions lead to Glucose 6-phosphate dehydrogenase (G6PD) enzyme deficiency?
- G6PD deficiency.
- Congenital nonspherocytic anemia.
- Non-immunologic hemolytic anemia of the newborn.
- African-American males around 13%.
- African females are 3%, and the carrier rate is around 20%.
- It is also seen in Greek, Sardinians, and Sephardic Jews.
- All persons with favism.
What conditions show increased Glucose 6-phosphate dehydrogenase (G6PD) enzyme?
- Megaloblastic anemia (untreated).
- Thrombocytopenic purpura (ITP = Werlhof disease). These patients become normal after splenectomy.
- Hyperthyroidism.
- Viral hepatitis.
- Myocardial infarction.
What drugs will initiate hemolysis due to Glucose 6-phosphate dehydrogenase enzyme (G6PD) deficiency?
- Antimalarial.
- Ascorbic acid.
- Aspirin.
- Dapsone.
- Nalidixic acid.
- Phenacetin.
- Quinidine.
- Sulphonamides.
- Thiazide diuretics.
- Tolbutamide.
- Vit. K.
- Primaquine.
- Nitrofurantoin.
- Dapsone.
- Acetanilide.
- Antipyretics.
- Sulfa drugs and sulphonamides.
How will you treat Glucose-6-phosphate Dehydrogenase (G6PD) deficiency?
- Avoid offending drugs.
- Treat the underlying infections.
- Keep a high urine output.
- Give blood transfusion in case of anemia.
- Newborn babies with G6PD deficiency are prone to neonatal jaundice.
- In such cases, phototherapy and exchange blood transfusion may be needed.
Questions and answers:
Question 1: What agents will lead to hemolysis in G6PD deficiency?
Question 2: What is the role of G6PD enzyme?