Gastrin, Zollinger-Ellison Syndrome
Gastrin Level
What sample is needed for Gastrin Level?
- Collect the venous blood to prepare the serum.
- A fasting sample is taken (at least for 12 hours of fasting).
- If the patient is not fasting, then the values will be different.
- The lowest values are between 3.00 a.m. and 7.00 a.m.
- Freeze the sample if the test is not done immediately.
What are the Indications for Gastrin Level?
- Gastrin level done in hyperacidity conditions.
- It is done to diagnose Zollinger-Ellison syndrome.
- This test also diagnoses G-cell hyperplasia.
- It is done to diagnose gastrinoma.
What precautions are needed for Gastrin Level?
- A high protein diet can increase gastrin levels 2 to 5 times the normal level.
- Diabetic patients on insulin may give a false raised level of gastrin.
- Patients with stomach surgery will have alkaline pH, a strong stimulant to gastrin.
- Drugs like antacids, H2-blockers (cimetidine, ranitidine), and hydrogen pump inhibitors (Omeprazole) will increase the gastrin level.
- Anticholinergic and tricyclic antidepressant drugs decrease the gastrin level.
- Avoid alcohol for at least 24 hours.
How will you define Gastrin?
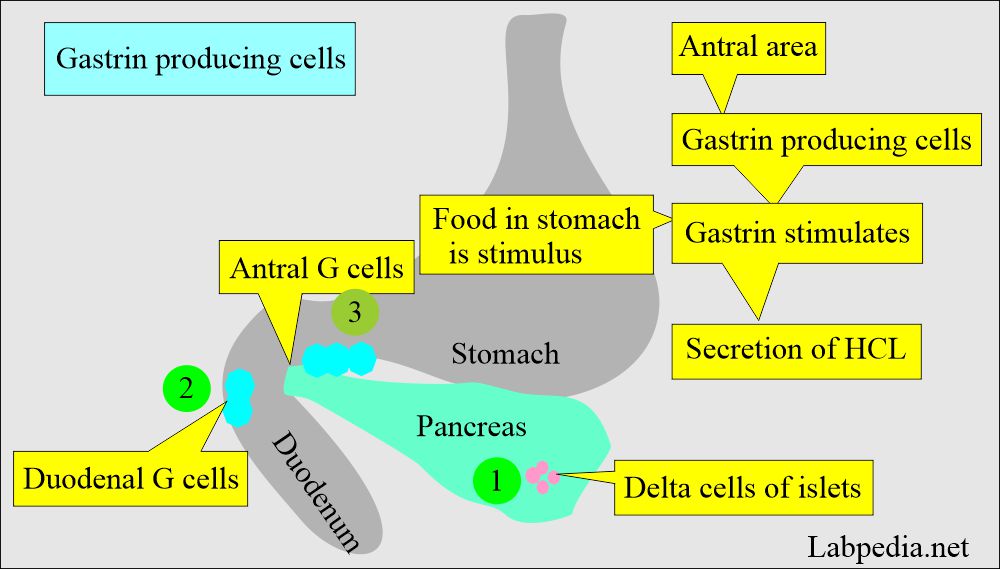
- Gastrins are a group of peptide hormones secreted by the antrum of the stomach, and these are powerful inducers of the gastric secretion of HCL.
- Food in the stomach produces Gastrin secretion in response to mechanical stress or high pH.
- Gastrin stimulates parietal cells to produce HCL.
How will you describe normal gastrin physiology?
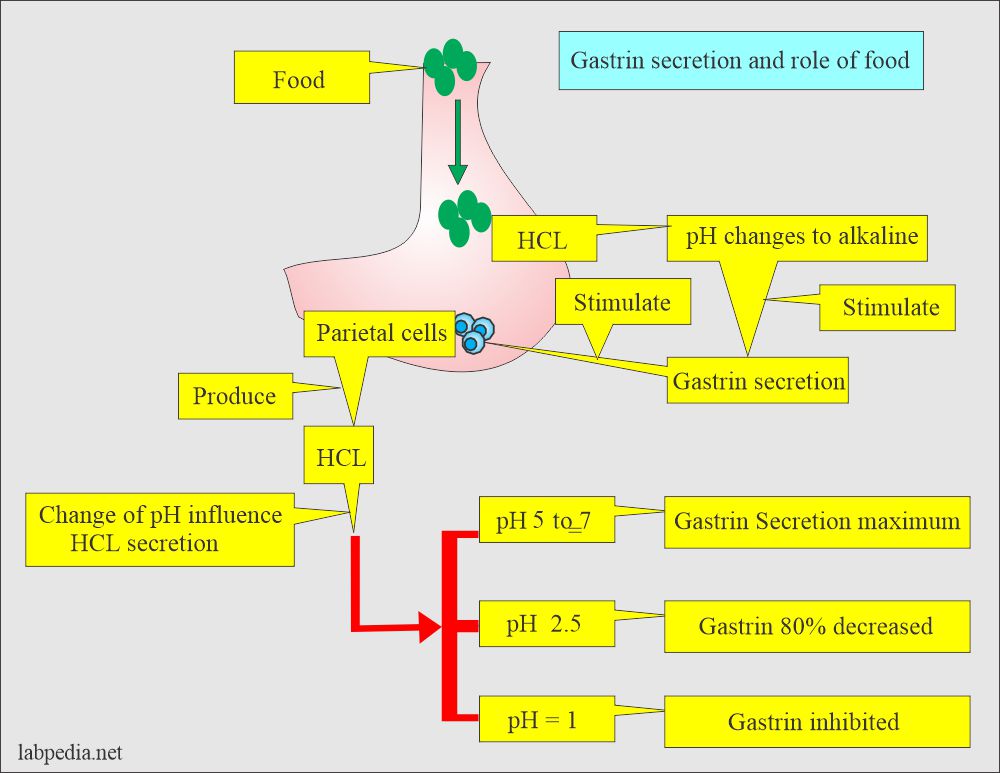
- When food enters the stomach, it changes pH to alkaline.
- This alkaline pH stimulates gastrin secretion to produce acid from parietal cells.
- Now, low pH stops further production of Gastrin.
- Secretion of gastrin:
- Maximal at Antral pH of 5 to 7.
- Reduced by 80% at a pH of 2 to 5.
- Inhibited at pH of 1.
- Secretion of gastrin:
- Zollinger Ellison syndrome is a gastrin-producing tumor of pancreatic origin with a high serum level of gastrin.
- Zollinger-Elison syndrome is due to non-beta cell tumors of the pancreas, which produce a large amount of gastrin.
- G-cell hyperplasia leads to high serum gastrin levels.
- Both conditions lead to an aggressive peptic ulcer.
- Gastrin level will be normal in the routine peptic ulcer.
- The Patient with antacid therapy or atrophic gastritis has a high gastrin level.
- A gastrin stimulation test is done by giving calcium or secretin.
What are the stimuli of the Gastrin secretion?
- Partially digested food.
- Alcohol and caffeine.
- Insulin-induced hypoglycemia.
- The smell of food, swallowing, and chewing.
- Calcium.
- Amino acids like glycine, tryptophan, and phenylalanine.
- Pancreatic islet tumors (non-β cells) produce large amounts of gastrin.
- Gastrin values follow a circadian rhythm and fluctuate physiologically to meals.
How will you discuss the pathophysiology of Gastrin?
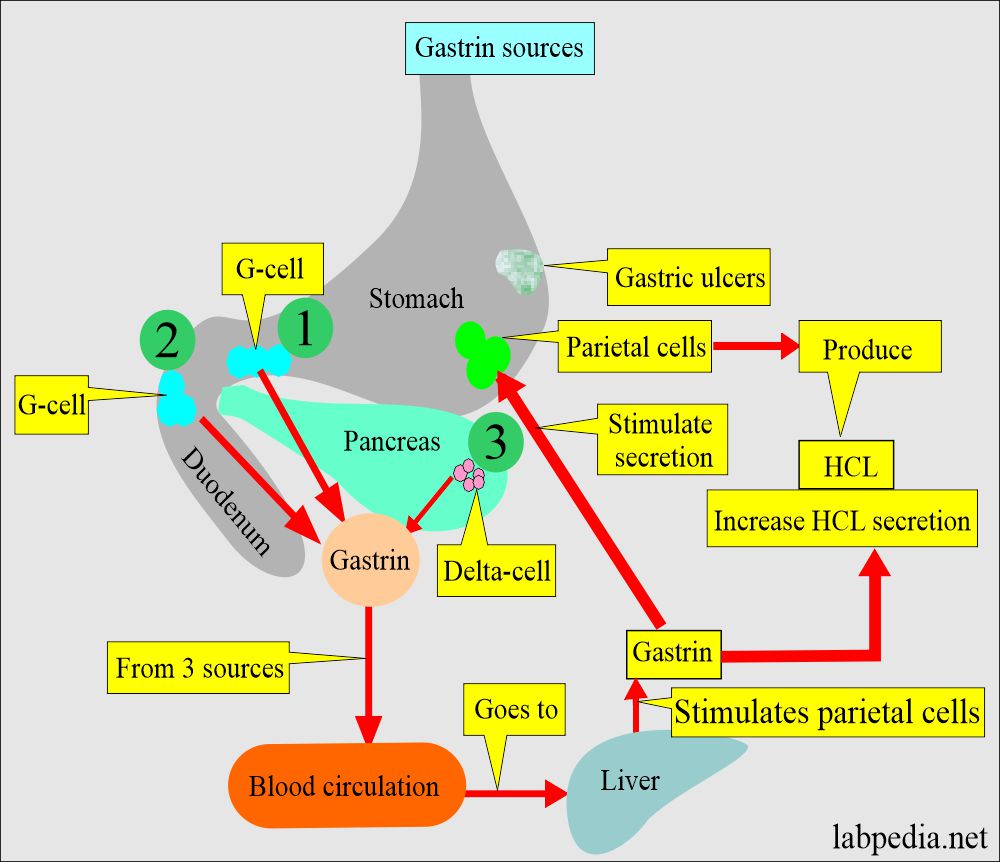
- Gastrin is a hormone produced by:
- Pancreatic delta cells.
- Duodenal G-cells.
- Stomach mucosa’s antral cells (G-cells).
- There are different forms of gastrin as biologically active forms that differ only in the length of the chain of the N-terminal end like:
- Small gastrin has 17 amino acids polypeptide (little gastrin G17).
- Big gastrin comprises 34 amino acid polypeptides (Big gastrin G34).
- Mini gastrin has 14 amino acids (G14).
- Little and big gastrin are found in the gastric antrum and duodenum.
- Gastrin stimulates gastric acid secretion, pepsinogen, intrinsic factor, and secretin, stimulates intestinal mucosal growth, and increases gastric and intestinal motility.
- Gastrin is produced from pregastrin, which has 101 amino acids and cleaves into gastrin.
- Gastrin from the three sources goes into circulation and then to the liver.
- The liver stimulates parietal cells to produce hydrochloric acid (HCl).
How will you interpret gastrin action?
- Gastrin is in the normal range for peptic ulcers without Zollinger-Ellison syndrome.
| Clinical presentation | Intragastric administration of 0.1 N HCL | Serum gastrin level |
| Peptic ulcer without Zollinger-Ellison syndrome | Normal | |
| Zollinger- Ellison syndrome | No change | Highly raised |
| Pernicious anemia | Marked decrease | Raised may reach Zollinger-Ellison syndrome level |
How will you describe the Gastrin functions:
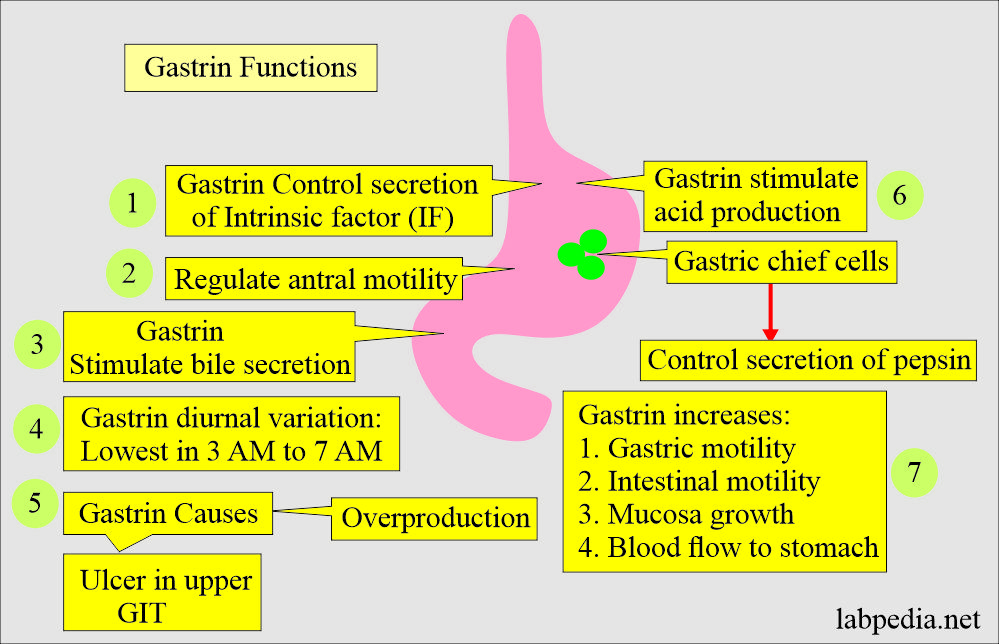
- Stimulates gastric acid production (potent stimulator).
- Gastrin overproduction causes ulcers in the upper gastrointestinal tract.
- Regulate antral motility.
- Control secretion of pepsin.
- Control secretion of intrinsic factors.
- Secretion from the intestinal mucosa.
- Stimulate hepatic bile secretion.
- Secretion of pancreatic HCO3- and enzymes.
- Gastrin increases:
- Gastric Motility.
- Intestinal motility.
- Mucosa growth.
- Blood flow to the stomach.
- Gastrin secretion has diurnal variation.
- Its lowest value is 3 a.m. to 7 a.m.
What is the normal Gastrin Level?
Source 1
| Age | pg/mL |
| Cord blood | 20 to 290 |
| 0 to 4 days | 120 to 183 |
| Child | <10 to 125 |
| !6 to 60 years | 25 to 90 |
| >90 years | <100 |
Source 2
- Adult = 0 to 180 pg/mL or 0 to 180 ng/L.
Source 6
- Adult = 0 to 180 pg/mL (0 to 180 ng/L).
- Child = 0 to 125 pg/mL.
- Levels are higher in elderly patients.
Source 4
- Adult = <25 to 100 pg/mL (<12 to 48 pmol/L)
- Children = 10 to 125 pg/mL (5 to 60 pmol/L)
- Postprandial = 95 to 140 pg/mL (46 to 67 pmol/L)
Another source
- Children = 10 to 125 pg/mL.
- Postprandial = 95 to 140 pg/mL.
- Levels are higher in elderly patients.
Another source
- Child = <10 to 125 pg/mL
- Adult 16 to 60 years = 25 to 90 pg/mL.
- Over 60 years = <100 pg/mL.
Gastrin Level and its relation to diseases:
| Gastrin level | Causes (Interpretations) |
|
|
|
|
|
|
|
|
What are the conditions where gastrin level is Increased?
- Zollinger-Ellison syndrome.
- G-cell hyperplasia.
- Atrophic gastritis.
- The retained antral portion after gastric surgery.
- Gastric carcinoma.
- Pyloric obstruction (gastric outlet obstruction)
- Gastric and duodenal ulcer.
- Chronic renal failure.
- Pernicious anemia.
- Vagotomy without gastric resection.
- Hyperparathyroidism.
What are the conditions where gastrin level is decreased?
- Hypothyroidism.
- Anterectomy with a vagotomy.
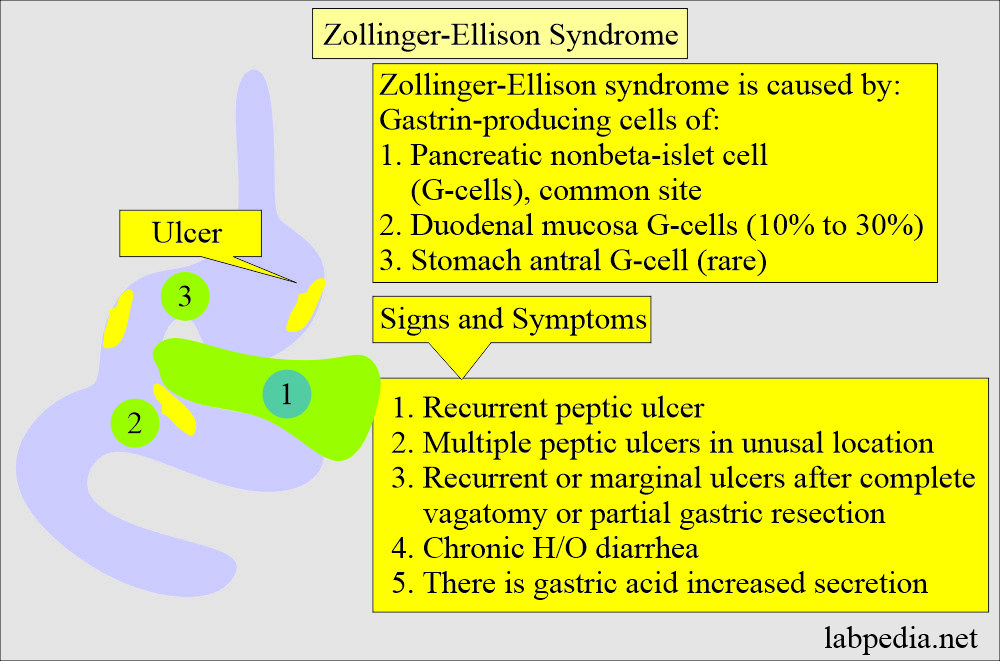
Zollinger-Ellison syndrome
How will you define Zollinger-Ellison syndrome?
- This is a disorder of autonomous gastric acid hypersecretion caused by the gastrin-secreting tumor.
- This gastrin production may be from non-β-cells tumors often present in the pancreas.
- Tumors are malignant in 50% of the cases, and 34% have metastatic disease.
- Hyperplasia only occurs in 10% of the cases.
How will you discuss the pathophysiology of Zollinger-Ellison syndrome?
- This is a gastrin-producing pancreatic tumor.
- Non-beta cell tumors of the pancreas produce excessive gastrin.
- The G cell’s hyperplasia of the stomach can also give a picture of Zollinger-Ellison syndrome.
- The patient has aggressive peptic ulcer disease.
- These patients have recurrence and complications.
How will you describe the signs and symptoms of Zollinger-Ellison syndrome?
- These patients have multiple ulcers in the antrum, the duodenum, and the jejunum.
- The ulcers are multiple.
- There is abdominal pain.
- There is burning and discomfort in the upper abdomen.
- There are acid reflux and heartburn.
- The patient may have diarrhea.
- The patient may have nausea and vomiting.
- The patient may have bleeding in the GI tract.
- The patient may have weight loss and decreased appetite.
- The gastrin level is normal in routine peptic ulcers.
- The gastrin level is normal in routine peptic ulcer disease, while it is high in Zollinger Ellison syndrome and G-cell hyperplasia.
- The patients on antacid or peptic ulcer disease medicines, atrophic gastritis, and patients with peptic ulcer surgery have slightly raised gastrin levels.
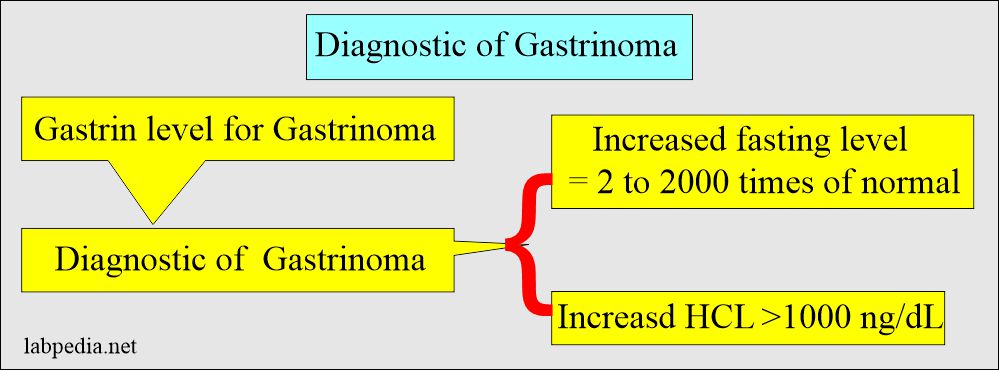
How will you diagnose Zollinger-Ellison syndrome?
- Gastrin assay is the method of choice.
- Most patients have fasting gastrin levels>500 pg/mL or >500 ng/L (fasting level is elevated in more than 95% of the cases).
- The gastrin level may reach 400,000 pg/mL.
- Gastrin level may be >5 times the normal value (1,000 pg/mL or 1,000 ng/L). This value is diagnostic.
- Advise Gastrin stimulation test using calcium or secretin.
- It is advised when the fasting level is <1,000pg/mL (1,000 ng/L) to assist the differentiation from other conditions.
- 90% of the Zollinger-Ellison syndrome patients have borderline gastrin fasting levels of 100 to 500 pg/mL.
- In response to the secretin stimulation test, these patients will increase 100 pg/mL above the baseline.
- When a calcium infusion test is given, gastrinoma patients have similar results.
- Gastrin stimulation test to diagnose Zollinger-Ellison syndrome:
- Secretin stimulation test:
- Give 2 units/Kg body weight (IV bolus).
- Estimate Gastrin level at baseline, 2, 5, 10, 15 minutes.
- Get >200 pg/mL (200 ng/L)over the baseline.
- Positive results were seen in 87% to 100% of Zollinger-Ellison syndrome.
- Calcium infusion test:
- Give calcium gluconate 10% as 5 mg/Kg/hour for 3 hours.
- Check gastrin as baseline, post-dose 120, 150, and 180 minutes.
- An increase >395 pg/mL (395 ng/L) occurs in 95% of Zollinger-Ellison syndrome.
- An increase of >3 times the baseline is seen in 85% of the cases.
- Response to the Calcium infusion test is less specific than a response to the secretin test.
Questions and answers:
Question 1: What are the functions of gastrin?
Question 2: What is the source of Gastrin?

Good lecture
Thanks.