Follicle-Stimulating Hormone (FSH), Follitropin
Follicle-stimulating hormone (FSH)
What sample is needed for follicle-stimulating hormone?
- It is done on the patient’s serum.
- Record the date of the last menstrual cycle in women.
- It is important to measure both FSH and LH levels.
- Plasma and urine are also acceptable.
- The sample was stable for 8 days at room temperature.
- 2 weeks at 4 °C.
- The urine sample should not contain preservatives.
- Storage at or below -20 °C is recommended.
- 3 hours of urine samples are preferred.
What are the Indications for Follicle-Stimulating Hormone (FSH)?
- FSH (along with LH) helps find whether the gonadal deficiency is of the primary origin or secondary due to insufficient pituitary hormone stimulation.
- FSH level helps to find the cause of hypothyroidism in women.
- FSH level helps to find the cause of endocrine dysfunction in men.
- FSH and LH are helpful in children with precocious puberty due to endocrine causes.
- In the case of the Anovulatory cycle (infertility problems), serial estimation to see the peak in mid-cycle will be missing.
- In primary ovarian or testicular failure, FSH helps find an increased level.
- FSH Helps to find the cause of infertility.
- FSH testing is commonly used to evaluate:
- Woman’s egg supply (ovarian reserve).
- Men’s low sperm count.
- To evaluate menstrual problems, such as irregular or absent menstrual periods (amenorrhea).
- FSH can help to determine whether the woman has gone through menopause.
- FSH level is done in menopause.
- FSH level is done in the case of abnormal vaginal or menstrual bleeding.
- In men where there are no testicles or underdeveloped.
- In children, the FSH level is done if there is delayed puberty.
- FSH determines early puberty (also called precocious puberty ) or delayed puberty.
- In children, the FSH level is who develops sexual features at a very young age.
- FSH diagnoses certain pituitary gland disorders, such as tumors.
What are the precautions for Follicle-stimulating hormone (FSH) estimation?
- Avoid hemolyzed, lipemic, or icteric samples.
- HCG and TSH may interfere with some immunoassays. So, patients with HCG-producing tumors and hypothyroidism will have a falsely high level.
- The recent administration of radioisotopes interferes with radioimmunoassay estimation of FSH.
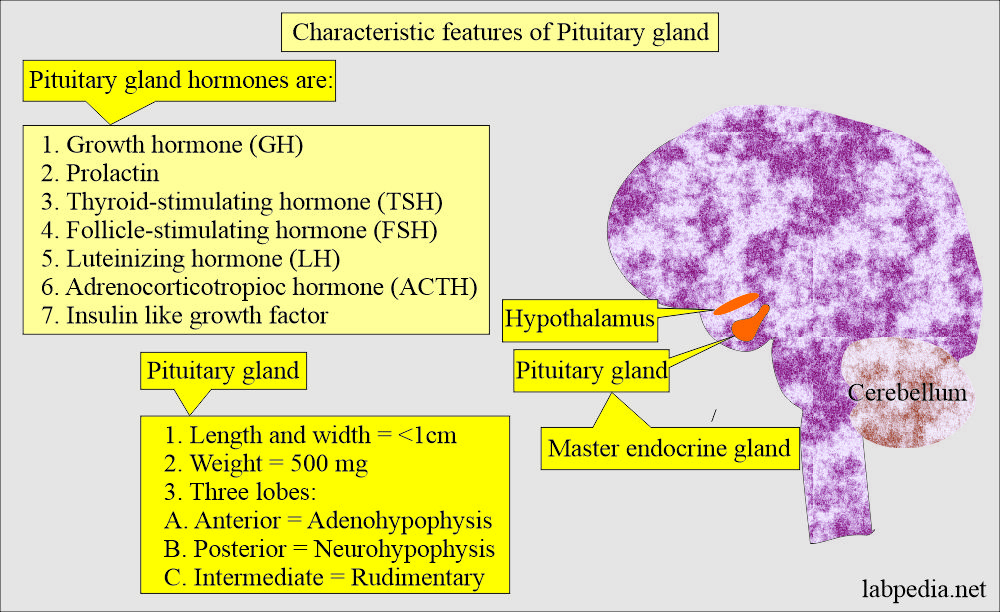
How will you describe the Characteristic features of the Pituitary gland?
- The pituitary gland is located at the base of the skull and in the bone cavity called sella turcica.
- The pituitary gland measures <1 cm in width and length, weighing around 500 mg.
- It is divided into:
- Anterior pituitary gland (adenohypophysis).
- Posterior pituitary gland (neurohypophysis).
- The intermediate lobe is rudimentary in human adults.
How will you discuss the Pathophysiology of Follicle-stimulating hormone (FSH)?
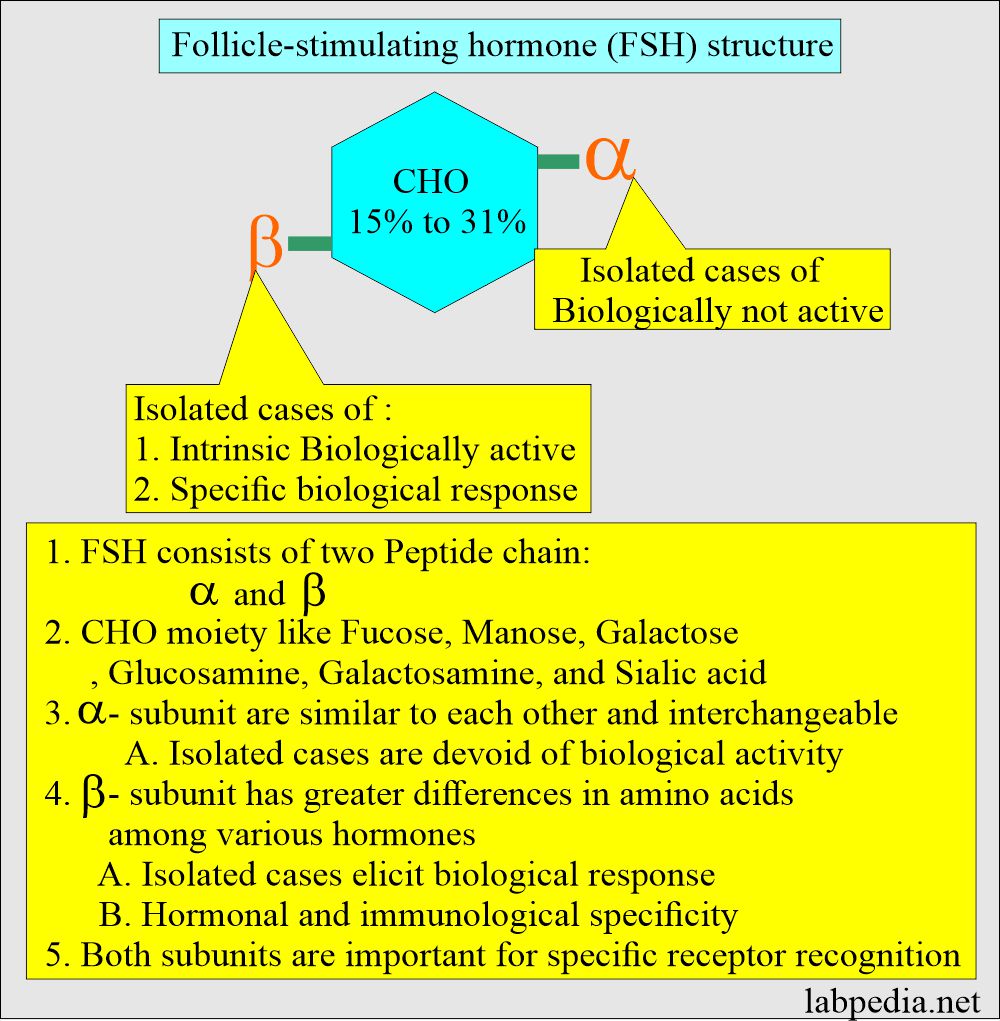
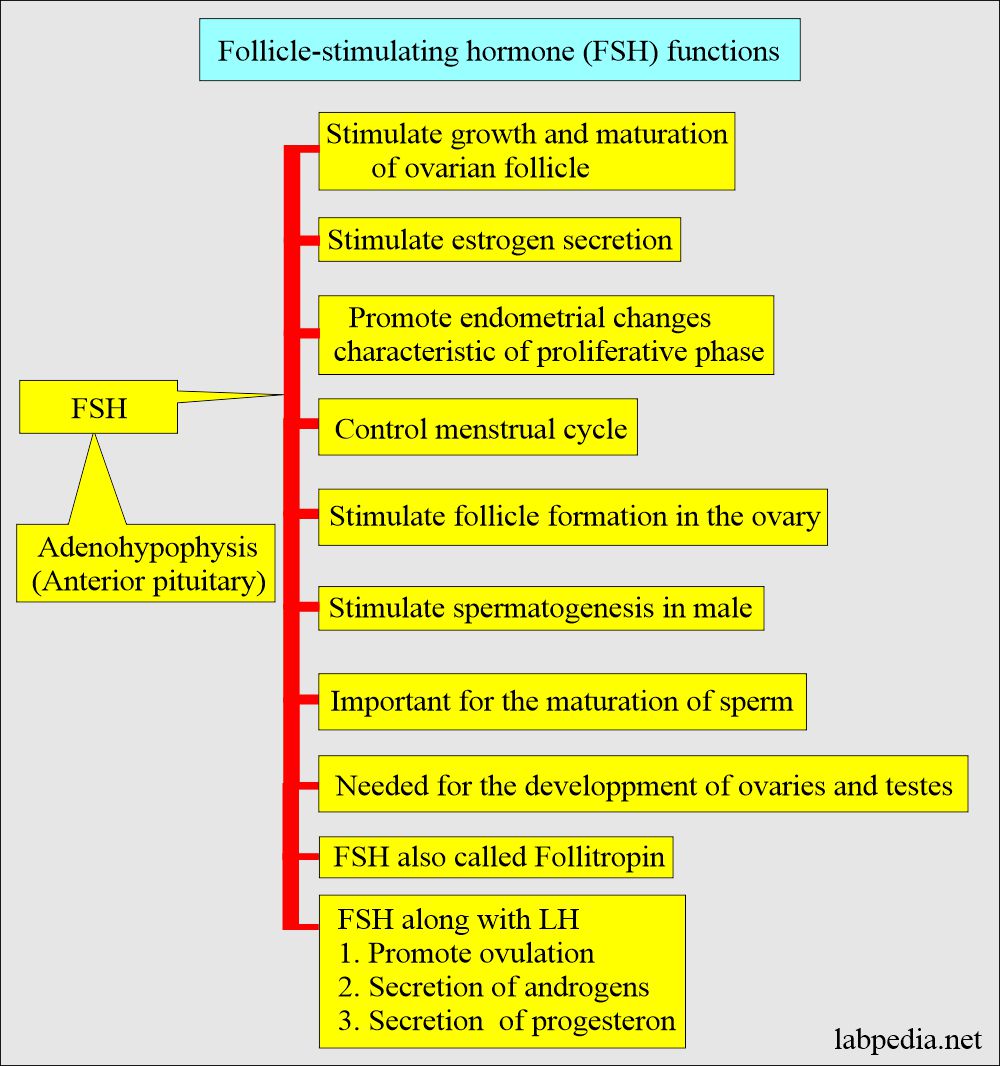
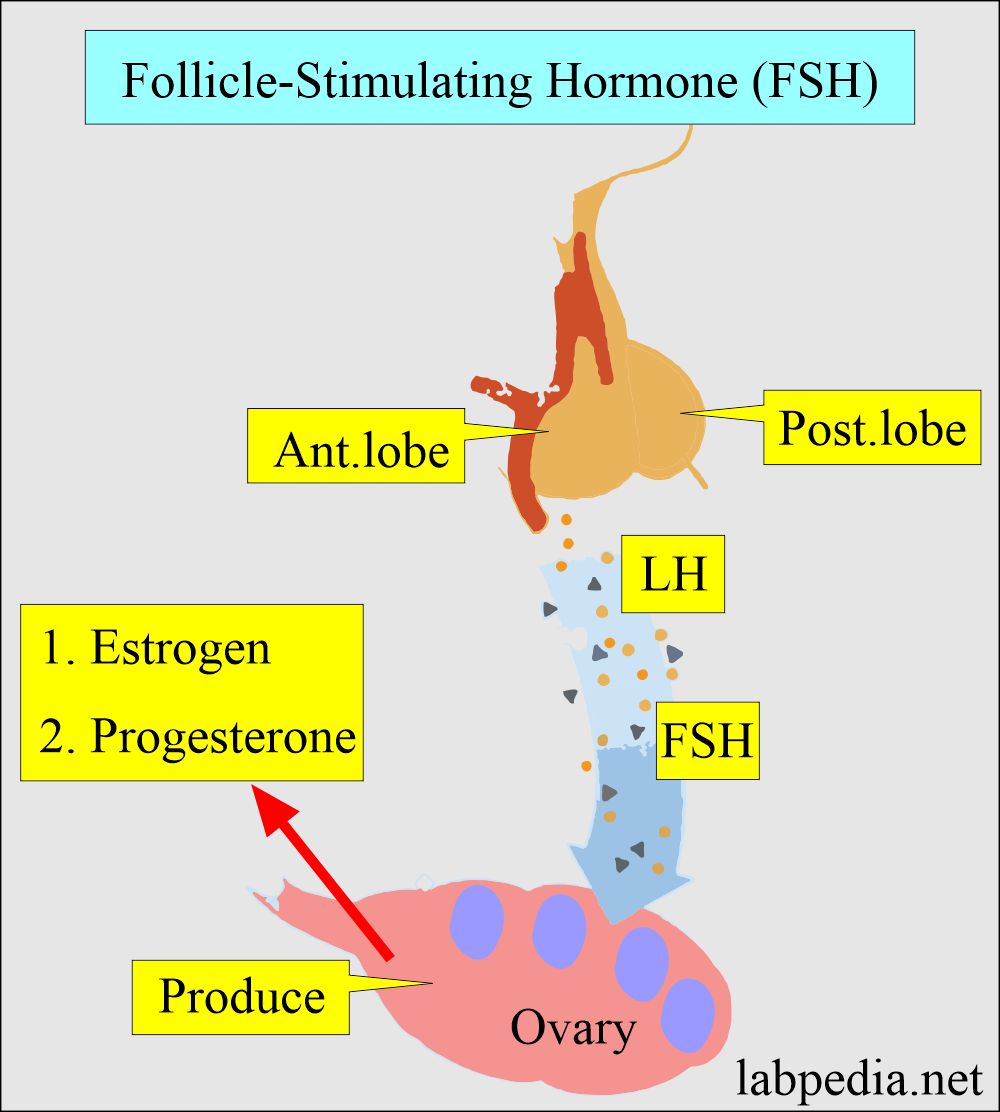
- FSH is synthesized in the adenohypophysis (anterior pituitary gland).
- FSH is a glycoprotein secreted by the anterior pituitary with a molecular weight of 32 kD.
- It consists of carbohydrates and two units of alpha and beta.
- FSH is produced and stored in the pituitary gland.
- When the α-unit combines with the β-unit, the biological activity increases for specific receptor recognition. Now, the β-subunit is responsible for specific biological responses.
What are the Functions of the follicle-stimulating hormone (FSH)?
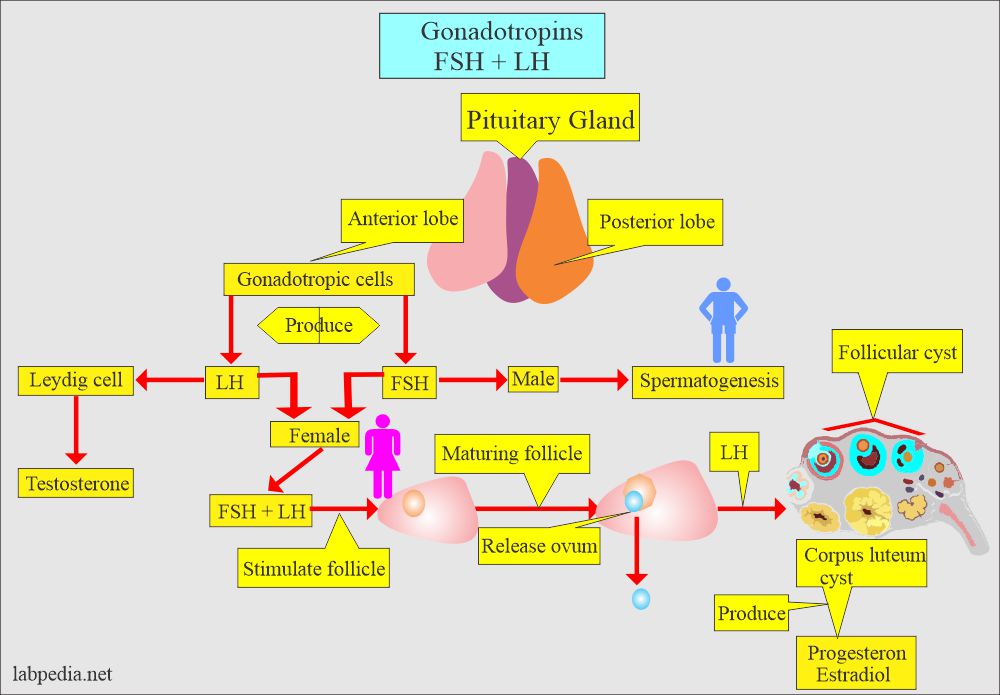
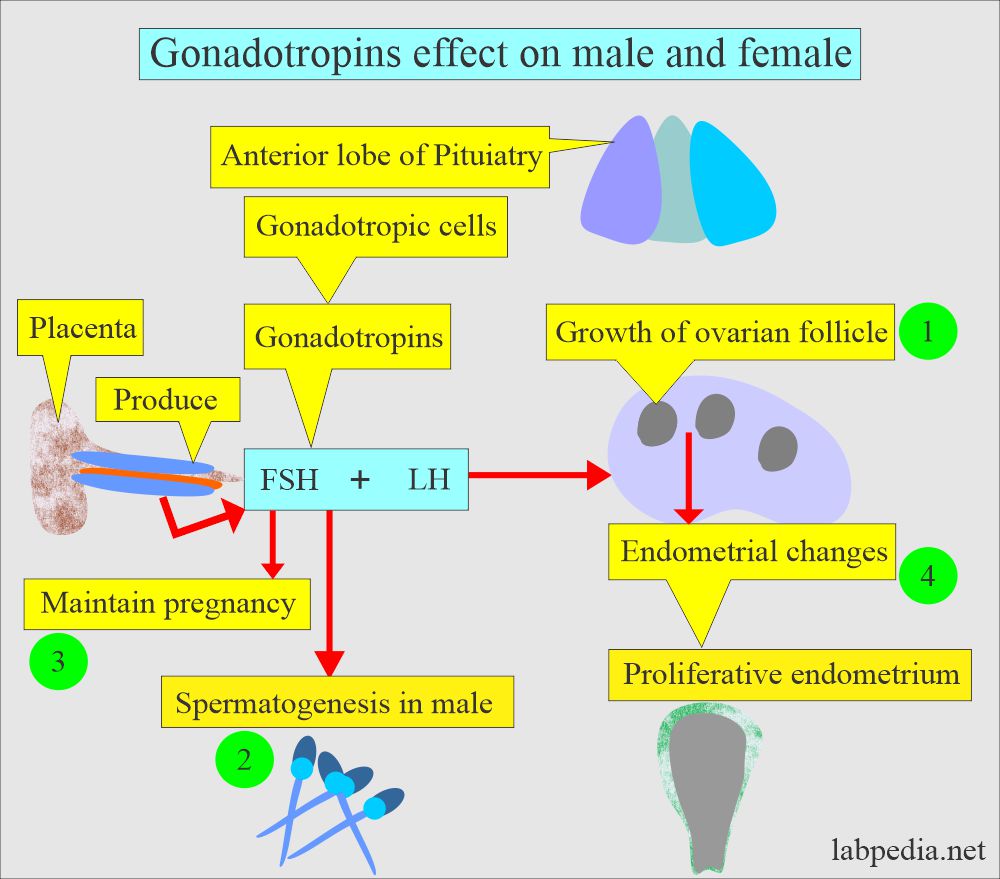
- The anterior pituitary gland secretes FSH and LH hormones, and these are given the name of gonadotropins.
- FSH is present in the plasma of males and females of all ages.
- Needed for the development of mature ova.
- It is also needed for the development of spermatozoa in males.
- FSH is needed for the pubertal development and function of the ovary and testes:
- Stimulate the growth and maturation of the ovarian follicles in the female.
- FSH stimulates estrogen secretion.
- FSH promotes endometrial changes in the proliferative phase of the menstrual cycle.
- FSH binds the Sertoli cells and promotes the synthesis of androgen-binding protein; this protein binds testosterone.
- FSH stimulates spermatogenesis.
- The FSH level can help determine whether male or female sex organs (testicles or ovaries) function properly.
What are the Follicle-stimulating hormone (FSH) effects in males and females?
- FSH is under the control of:
- Hypothalamic-gonadotropin hormone (G N R H).
- Ovarian estrogen and progesterone are in females, while testosterone is low in males.
- FSH acts on the ovary’s granulosa cells and the testes’ Sertoli cells.
- FSH level increases at the time of puberty in both sexes.
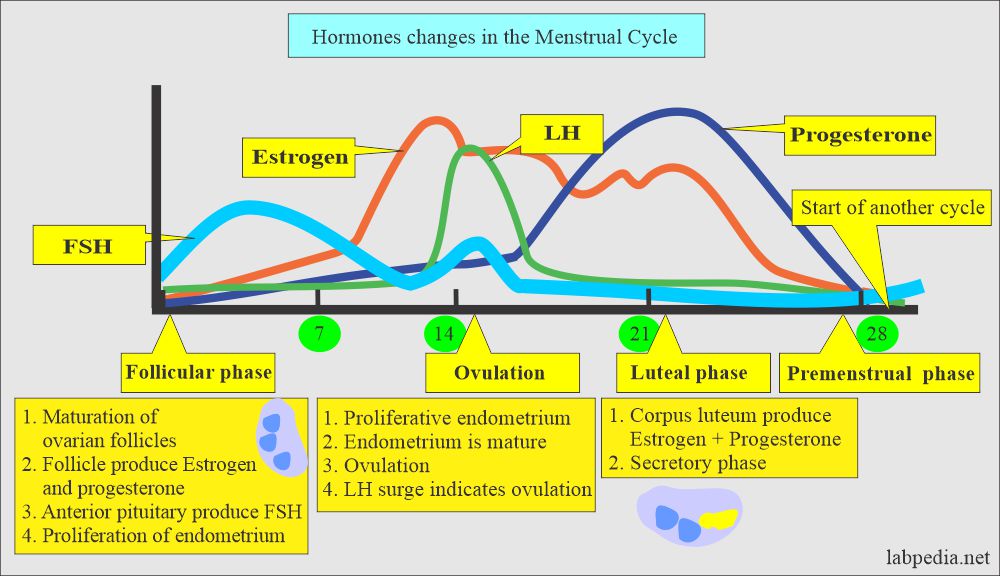
- The amount of FSH varies throughout a woman’s menstrual cycle and is highest just before ovulation.
- FSH and LH sharply rise from the basal level just before ovulation in ovulating females.
- FSH stimulates the formation of the follicle in the early stage of menstruation.
- The amount of FSH varies throughout a woman’s menstrual cycle and is highest just before ovulation.
- The great increase in FSH and LH occurs in women after menopause and remains elevated for the rest of life.
- In males, FSH and LH are necessary for the maturation of spermatozoa.
- A surge of LH leads to ovulation from the primed or active follicle in the mid-cycle.
- It is one of the female hormones In women. FSH helps control the menstrual cycle and ovulation by the ovaries.
- In men, FSH helps control the production of sperm. The amount of FSH in men normally remains constant.
What are the normal levels of Follicle-Stimulating Hormone (FSH)?
Source 1
| Age | mIU/mL Male | mIU/mL Female |
| Prepuberty child | ||
| 2 to 11 month | 0.19 to 11.3 | 0.10 to 11.3 |
| 1 to 10 years | 0.3 to 4.6 | 0.68 to 6.7 |
| Puberty Tanner stage | ||
| 1 -2 | 0.30 to 4.6 | 0.68 to 6.7 |
| 3 to 4 | 1.24 to 15.4 | 1.0 to 7.4 |
| 5 | 1.53 to 6.8 | 1.0 to 9.2 |
| Adult | 1.42 to 15.4 | |
| Follicular phase | 1.37 to 9.9 | |
| Ovulatory phase | 6.17 to 17.2 | |
| Luteal phase | 1.09 to 9.2 | |
| Postmenopausal | 19.3 to 100.6 |
-
- To convert into SI units x 1.0 = IU/L
Another source
Women before puberty = 0 to 4 mIU/L
- Menstruating women
- Follicular = 5 to 20 IU/L.
- Ovulatory phase = 30 to 50 IU/L.
- Luteal phase = 1.09 to 9.2 IU/L.
- Women post menopause = 19.5 to 100.6. IU/L.
- Men before puberty = 0 to 5 mIU/L
- Men during puberty = 1.42 to 15.4. IU/L
- Men adult = 1.5 to 12.5 IU/L.
- Children:
- Male = 0.3 to 4.6 IU/L.
- Female = 0.68 to 6.7 IU/L.
Source 2
| Sex | LH IU/ L | FSH IU/ L |
|---|---|---|
| Adult | ||
| Male | 1.24 to 7.8 | 1.4 to 15.4 |
| Female | ||
| Follicular phase | 1.68 to 15 | 1.37 to 9.9 |
| Ovulatory phase | 21.9 to 56.6 | 6.17 to 17.2 |
| luteal phase | 0.61 to 16.3 | 1.09 to 9.2 |
| Postmenopausal | 14.2 to 52.3 | 19.3 to 100.6 |
| Child | ||
| 1 to 10 years: male | 0.04 to 3.6 | 0.3 to 4.6 |
| 1 to 10 years: female | 0.03 to 3.9 | 0.68 to 6.7 |
(Values vary from lab to lab. above data is from two sources)
Hormone cycles in the menstrual period:
| Phase of Cycle | LH | FSH | Progesterone | Estradiol |
| Follicular phase | low | High | low | low |
| Late follicular phase | High | low | lower limit | high |
| Mid-cycle | Peak | raised | increasing | low |
| Luteal phase | raised | raised | high | high |
| Start of Next cycle | low | rising | rising | rising |
What are the causes of High Hormones in the menstrual cycle?
- Loss of ovarian function before age 40 (ovarian failure).
- Polycystic ovary syndrome (PCOS).
- Menopause has occurred.
- Pituitary adenoma.
- Precocious puberty.
- Ovarian dysgenesis (Turner syndrome ).
What will be the menopause picture?
- Menopause occurs due to the aging of the ovary and deletion of the ovarian follicles.
- Urinary estrogen is decreased.
- Androstenedione and testosterone are decreased.
- DHEA and dehydroepiandrosterone (DHEA-S) are decreased.
- Progesterone is <0.5 ng/mL.
- Serum estradiol is <5 ng/dL.
- FSH is increased by >40 mIU/mL., confirming the primary ovarian failure.
- Plasma and urine gonadotropins are increased.
- The vaginal smear shows typical menopausal changes.
What causes High Follicle follicle-stimulating hormone (FSH) values in a man?
- Klinefelter syndrome ( Testicular dysgenesis ).
- Testicles are absent or not functioning properly.
- Alcohol dependence or treatments like X-rays or chemotherapy have damaged testicles.
- High values in children may mean that puberty is about to start.
- Complete testicular feminization syndrome.
What are the causes of decreased follicle-stimulating hormone (FSH)?
- Pituitary failure.
- Hypothalamic failure.
- Stress.
- Anorexia nervosa.
- Malnutrition.
What is the significance of low Follicle follicle-stimulating hormone (FSH) values?
- A woman not producing eggs (prevents ovulation) leads to infertility.
- A man is not producing sperm.
- The hypothalamus or pituitary gland is not functioning properly.
- A tumor is present that interferes with the brain’s ability to control FSH production.
- Stress.
- Starvation or being very underweight.
Questions and answers:
Question 1: What is the value of FSH in menopause?
Question 2: What is the site of formation of FSH?