Fluid Analysis:- Part 8 – Synovial Fluid Analysis, Arthrocentesis
Synovial Fluid Analysis
What Sample is needed for Synovial fluid analysis?
- Synovial fluid is the aspirated fluid from the synovial spaces called Arthrocentesis.
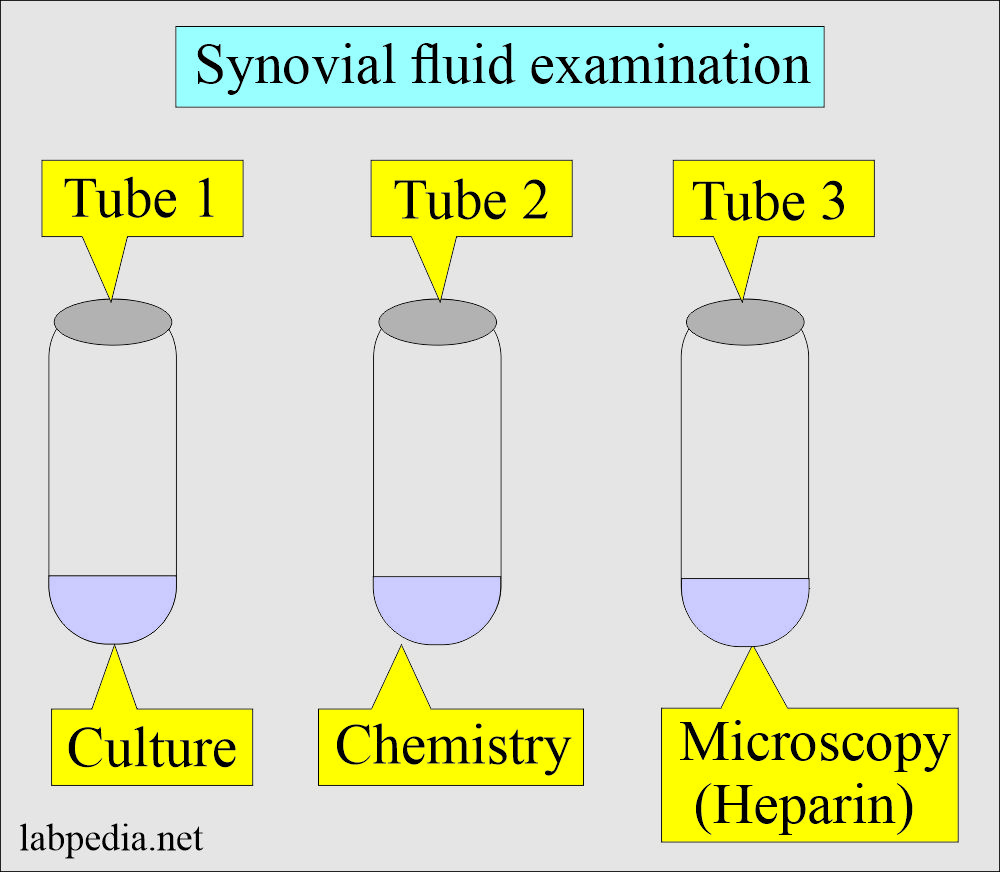
- Collect specimens in three tubes:
- Tube 1 for culture.
- Tube 2 for microscopy, add heparin, and do not use EDTA powder.
- You can use liquid EDTA.
- Tube 3 for chemistry.
- For glucose, the patient should have 6 hours of fasting.
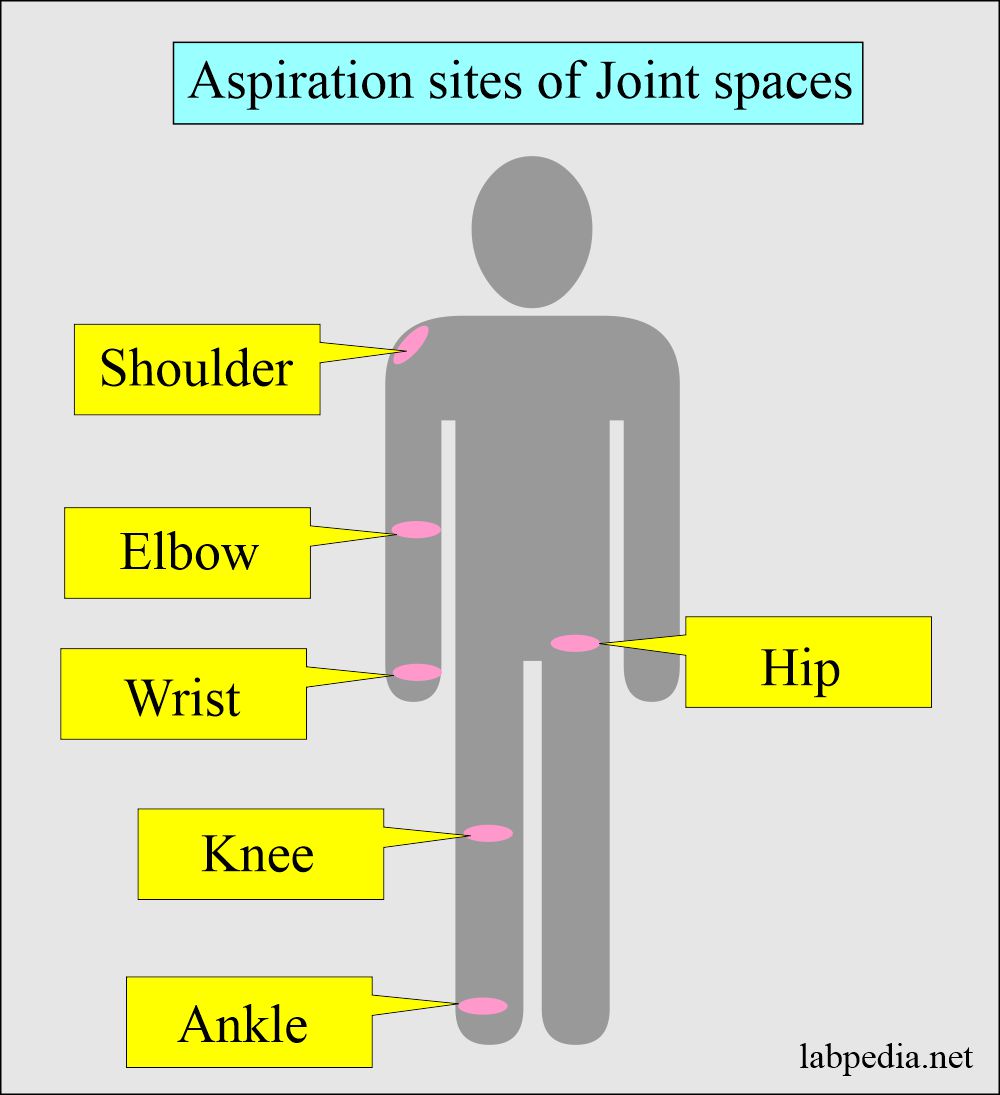
- Synovial fluid can be aspirated from joints of:
- Knee.
- Shoulder.
- Elbow.
- Wrist.
- Ankle.
- Hip.
What are the precautions for synovial fluid aspiration (Arthrocentesis)?
- Powered anticoagulants should not be used because this may interfere with crystal analysis.
- The non-anticoagulant test tube should be centrifuged to prevent the cellular elements from interfering with the chemical and serologic analysis.
- All testing should be done as soon as possible to prevent cellular and possible changes in the crystal.
What are the contraindications for arthrocentesis?
- Avoid in case of skin infection or wound in the area of aspiration.
What are the Indications for synovial fluid analysis (Arthrocentesis)?
- To diagnose the cause of synovial fluid formation.
- To differentiate inflammatory from non-inflammatory causes.
- Arthritis due to crystals like gout and pseudogout.
- Malignant tumor involving the joint.
- To inject anti-inflammatory medicines like corticosteroids.
- To monitor chronic arthritic diseases.
How will you define synovial fluid?
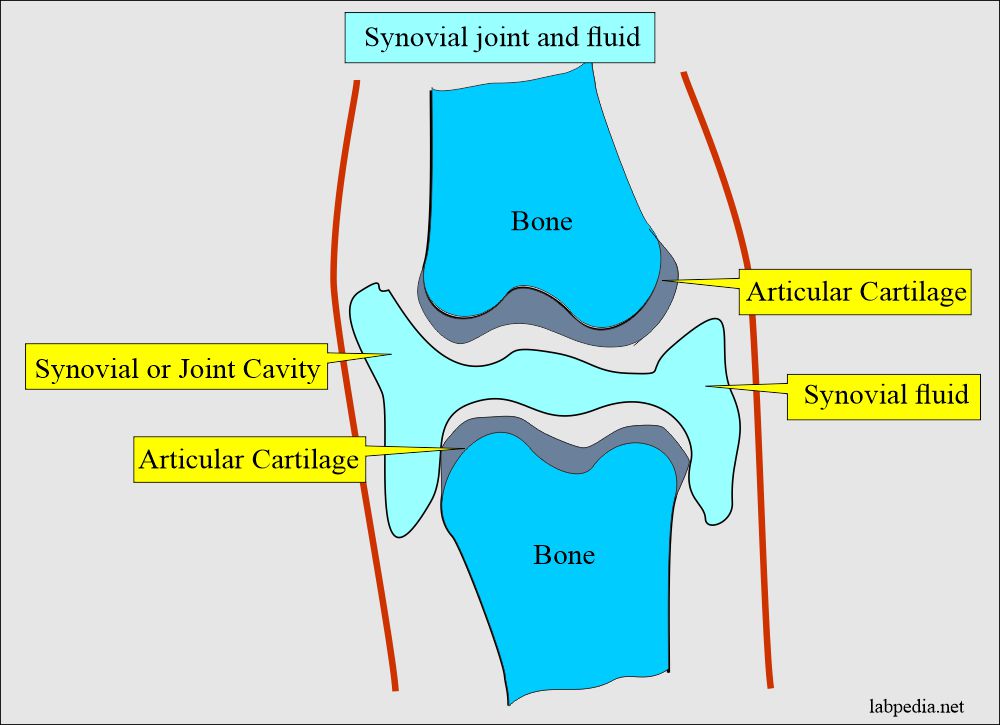
- This is often referred to as joint fluid, the viscous fluid found in the cavities of the moveable joints.
- It is clear and straw-colored with few WBCs, and no crystals are found.
- There is good mucin clot formation.
- Synovial fluid is transudate with <200 WBCs and <25% neutrophils.
What are the components of synovial fluid?
- Synovial fluid is formed as an ultrafiltrate of plasma across the synovial membrane.
- This filtration is nonselective except for the exclusion of high molecular weight proteins.
- The contents of the synovial fluid are similar to the plasma values.
- This synovial fluid does not typically clot. However, the inflammation due to increased fibrinogen may clot.
- The synovial cells lining the synovium secrete a mucopolysaccharide containing hyaluronic acid and a small amount of the protein.
- This hyaluronic acid causes noticeable viscosity of the synovial fluid.
- Synovial fluid is present normally in a very small amount. The amount in the large knee joint is less than 3.5 mL.
- This fluid collection can increase inflammation and may be around 25 mL.
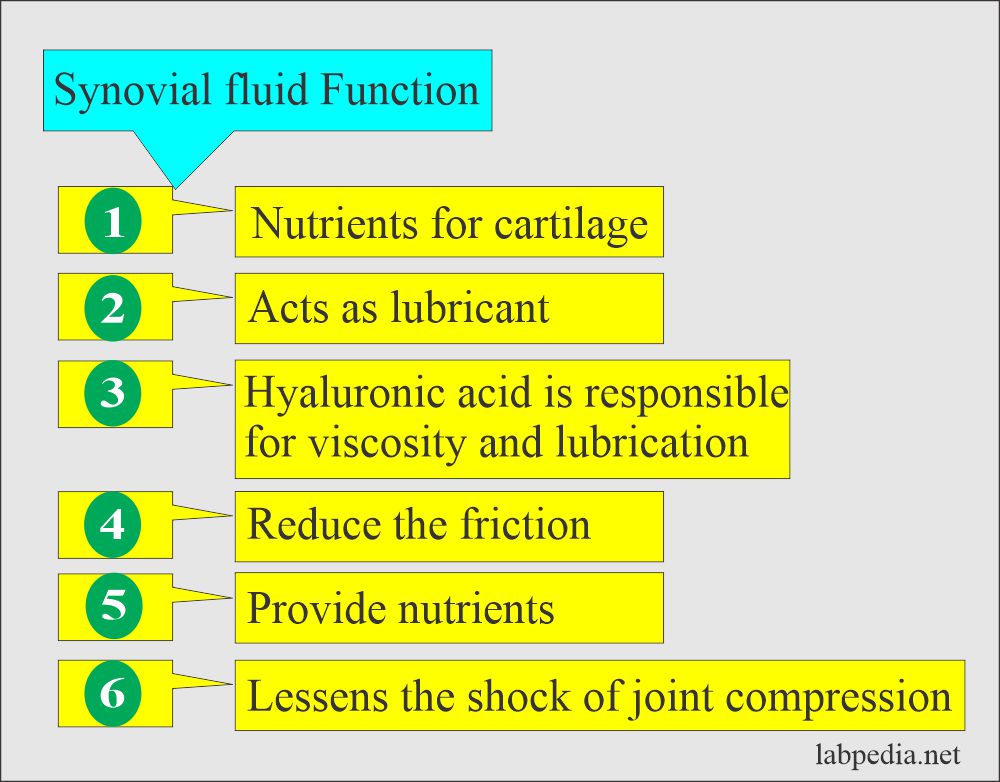
- Synovial fluid contains mucopolysaccharides called hyaluronic acid, which are responsible for the viscosity of the synovial fluid and lubricate the joints.
- An increase in a synovial fluid enough to aspirate is due to some disease.
What are the functions of the synovial fluid?
- The smooth articular cartilage and synovial fluid reduce friction between the bone during joint movements.
- Synovial fluid supplies nutrients to the cartilage and acts as a lubricant to the joint, bursa, and tendons sheaths.
What are the types of arthritis?
- Damage to the articular membrane produces pain and stiffness in the joints, referred to as arthritis.
- There are the following types of arthritis:
- Noninflammatory:
- This arthritis is seen in osteoarthritis, trauma, neuropathic osteoarthroscopy, pigmented villonodular synovitis, and osteoarthritis dissecans.
- Inflammatory:
- Inflammatory or crystal-induced arthritis is due to rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and pseudogout (chondrocalcinosis).
- In inflammatory or crystal-induced arthritis, there are predominantly polys.
- Septic arthritis:
- It may be due to bacteria, tuberculosis, viral, and fungi.
- Hemorrhagic arthritis:
- It is due to trauma, synovioma, and pigmented villonodular synovitis.
How will you classify arthritis?
| Etiological classification | Cause of the arthritis |
| Non-inflammatory | Degenerative joint disease (Osteoarthritis) seen in old age |
| Inflammatory | An immunologic disorder like Rheumatoid arthritis and SLE |
| Septic | Due to microbial infection |
| Hemorrhagic | Coagulation factor deficiency and traumatic injury |
| Due to crystals | Uric acid in gout |
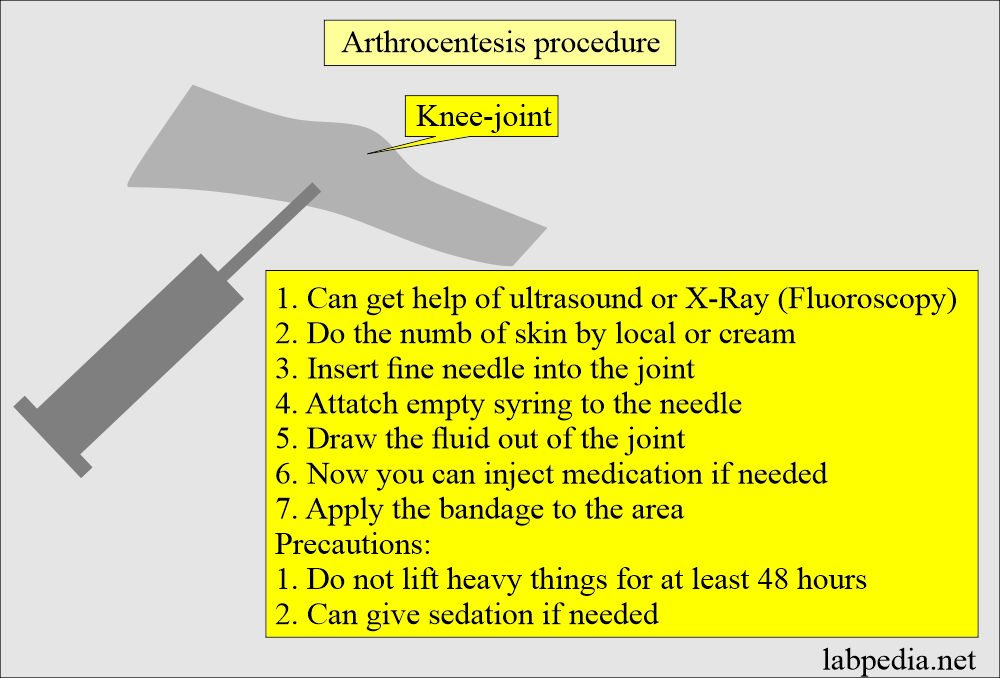
How will you perform arthrocentesis to get synovial fluid?
- Sterile the area with an antiseptic solution.
- Can give local anesthesia to decrease the pain.
- Lie the patient on their back with the joint fully exposed.
- The joint may be wrapped with an elastic bandage to compress free fluid within a particular area to get maximum fluid during aspiration.
- Insert a sterile needle into the joint space and get the synovial fluid for analysis.
- If corticoid steroids need to be injected, in that case, connect the already-filled syringe to the aspiration needle.
- Keep one mL in a sterile tube for culture.
- Another one mL in a heparinized tube for cell count.
- Also, collect the blood for the comparison of the chemicals.
- Aftercare:
- Note the severity of the pain.
- Apply ice packs to decrease the pain and swelling.
- Keep the pressure dressing to decrease the collection of fluid or hematoma formation.
- Avoid strenuous exercise for the next several days.
- Contraindication:
- Avoid if there is skin or wound infection in the aspiration site because of the risk of sepsis.
- Complication:
- There is a risk of joint infection and hemorrhage in the joint area.
- There may be a hemorrhage in the joint.
What are the normal values of synovial fluid?
Source 1
| Features | Findings |
| Physical features | |
|
|
|
|
|
|
|
|
|
|
|
|
| Microscopic examination | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Chemicals | |
|
|
|
|
|
|
|
|
|
|
What are the findings in different types of arthritis?
| Test | Noninflammatory | Inflammatory (acute) | Septic | Hemorrhagic |
|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Synovial fluid laboratory tests:
What are the parameters in the synovial fluid analysis?
WBC count.
- Generally, WBCs <200/cmm and RBCs <2000/µL.
- There is an overlap between infectious and noninfectious arthritis.
- In bacterial arthritis, neutrophils >75%.
- Neutrophils >90% are diagnostic of bacterial arthritis.
Protein and lactate level:
- Estimate synovial fluid protein, uric acid, and lactate.
- Increased uric acid level indicates gout.
- Increased protein and lactate levels suggest a bacterial infection.
Mucin clot (Ropes test):
- A few drops of the synovial fluid, add 10 to 20 mL of 5% acetic acid in a test tube.
- After one minute, shake the test tube.
- Interpretations:
- Normal findings = Firm clot with a surrounding fluid having a clear appearance.
- Well-formed clot = In non-inflammatory arthritis (good clot).
- Clot good to poor = Non-infectious arthritis.
- The clot is poor = Bacterial arthritis.
- Clinical significance of mucin clot:
- It helps to diagnose inflammatory joint diseases.
- However, this test lake specificity is 49% and has a low % predictive value of 52%.
- This is not the test to diagnose joint diseases.
Viscosity:
- Allow the drip of the fluid from the needle.
- Note the string formation.
- Normal and non-inflammatory synovial fluid = String is 3 cms long.
- Acute inflammatory conditions = Fluids drips and very little string or no string formation.
Synovial glucose level:
- It is 10 mg/dL less than normal blood glucose and is always within the 20 mg/dL range.
- It is better to get blood glucose and the synovial fluid sample simultaneously for comparison.
- The patient should have fasted for 6 to 8 hours.
- In degenerative arthritis, synovial fluid glucose is normal.
- Synovial fluid glucose level falls with increasing severity of the inflammatory process.
- This is the lowest in septic arthritis. This may be 50% less than serum glucose levels (<40 mg/dL). It is seen in only 50% of the cases.
- Glucose is also low in rheumatoid arthritis, SLE, and gout. It is a mild to moderate decrease and is usually 40 mg/dL below the serum level.
- In bacterial arthritis, there is an increased level of protein and lactate.
- Rheumatoid arthritis shows more lymphocytes (lymphocytosis).
Gram stain:
- It is done for the diagnosis of infection/noninfectious causes:
- It is positive in 40% to 75% of the cases.
- It can diagnose Gonorrhea.
AFB stain:
- It is done to rule out tubercle bacilli.
Complement:
- The complement level is done, which is low in the:
- Systemic lupus erythematosus.
- Rheumatoid arthritis.
- Other immunologic arthritis.
- Total complement may be increased in Reiter’s syndrome.
Rheumatoid arthritis (RA) factor:
- This may be positive before the blood test for Rheumatoid arthritis on the synovial fluid.
- LE cell phenomenon may be positive on synovial fluid.
Cholesterol crystals:
- Cholesterol crystals are found in rheumatoid arthritis.
Culture and sensitivity:
- This is the best tool for diagnostic purposes.
- This is advised for bacteria and fungi.
- If the patient has taken antibiotics, then it will decrease the positivity.
Polarized microscopy:
- It is done in the presence of crystals.
- The calcium pyrophosphate dihydrate crystals are birefringent in pseudogout (blue on red background).
- Cholesterol crystals are seen in rheumatoid arthritis.
What is the summary of the lab findings of synovial fluid analysis?
- Noninflammatory disease:
- Clear and straw color.
- WBCs count = <2000 WBCs, and Neutrophils are 25%.
- Inflammatory diseases:
- The fluid is turbid yellow.
- <75000 WBCs, and Neutrophils >50%.
- Septic arthritis:
- Fluid is opaque (Turbid yellow).
- >7500 WBCs, and Neutrophils >75%.
- Culture positive (Gonorrheal disease, TB, or other organisms).
What are the findings in synovial fluids in different types of arthritis?
| Diseases | Viscosity | Mucin clot | Glucose | Total cell count | Neutrophils | Special tests |
| Normal synovial fluid | Normal or increased | Good clot | After fasting, the same level | 0 to 200/cmm | 0 to 25% | |
| Gout | Low |
|
Normal to 30 mg/dL, below blood level | 2000 to 50,000/cmm | 40% to 90% | Urates crystals |
| Pseudogout | Low |
|
Normal | 2000 to 50,000/cmm | 35% to 85% | calcium pyrophosphate crystals |
| Rheumatoid arthritis | Low |
|
Normal to 30 mg/dL, below blood level | 2000 to 50,000/cmm | 70% to 80% | RA factor is positive |
| Systemic lupus erythematosus (SLE) | Normal or low | Good to fair | Normal to 20 mg below blood level | 2000 to 5000/cmm | 10% to 30% | LE cell preparation |
| Osteoarthritis | Normal | Good | 500/cmm | 25% | Cartilage fragments | |
| Trauma with hemorrhage | Normal | Good | >5000/cmm | 25 to 50% | many RBCs | |
| Acute bacterial arthritis | Low | Poor | >40 mg below the blood level | >50,000/cmm | 75% to 95% |
|
| Acute rheumatic fever | Low | Good to poor | Small decrease | 2,000 to 15,000/cmm | 50% to 60% | Negative |
What is Gout (Gouty arthritis)?
- Gout is a purine metabolism disorder characterized by monosodium urate crystals in the synovial fluid.
- These crystals are present in the soft tissues and the synovial fluid.
- There are attacks of acute inflammatory arthritis and hyperuricemia.
- Urine acid is mostly synthesized in the liver and intestinal mucosa.
- The kidneys excrete 2/3 and 1/3 by the intestine in feces.
- Increased serum uric acid.
- The synovial fluid will show characteristic crystals.
- There is increased fluid uric acid.
- There are monosodium urate crystals.
- There are increased monocytes.
- Calcium pyrophosphate is present in chondrocalcinosis (pseudogout).
- Cholesterol is common in chronic arthritis. These are birefringent, square plate-like crystals with notched corners.
What is pseudogout?
- It is also known as chondrocalcinosis. and Crystalline arthropathy.
- It may involve one or multiple joints.
- It is an inflammatory reaction due to calcium pyrophosphate dehydrate crystals deposition in the joints.
- These typical crystals are seen in the synovial fluid inside and outside the WBCs.
- Blood and urine findings are normal.
Questions and answers:
Question 1: What is the glucose level of synovial fluid in gout,
Question 2: What is the normal volume of the synovial fluid.

You did not have any info if the synovial fluid color is pale pink, or if the body fluid appearance is hazy, red cell count is 1810 or lower, 2/cumm, and what happens if a person shows lymps that are seen in smear survey
Please, I have added what you want.
SIR WHAT ABOUT GENEXPERT CAN BE DONE OR NOT AND CRITERIA TO RULLOUT MALIGENCY.
Genexpert can be done on the urine. To rule out malignancy; better to do cytospin preparation of the morning urine sample.
Hello. I am a lay person researching what may cause the increase in synovial fluid viscosity. I’ve search this page, and I may have overlooked what may be the cause. My hunch is the it may be related to hyperglycemia, if so, can you please point me to an article or research paper that may have that information. Thank you very much.
These are the references you can find on google.
1. It’s another reason to eat leafy greens, bright-colored fruits and vegetables, nuts, seeds, and foods high in omega-3 fatty acids; they nourish your joints and keep your synovial fluid healthy. Add foods high in allicin like onions and garlic, and fermented foods like yogurt and kefir, and your joints will thank you.02-Aug-2021.
2. Hyaluronic acid provides the high viscosity of the synovial fluid and, with water, its lubricating properties.
3. Consuming healthy fats can increase joint health and lubrication. Foods high in healthy fats include salmon, trout, mackerel, avocados, olive oil, almonds, walnuts, and chia seeds. The omega-3 fatty acids in these foods will assist in joint lubrication.