Fluid Analysis:- Part 5 – Amniotic fluid Examination (Amniocentesis)
Amniotic fluid Examination (Amniocentesis)
What sample is needed for Amniotic fluid Examination (Amniocentesis)?
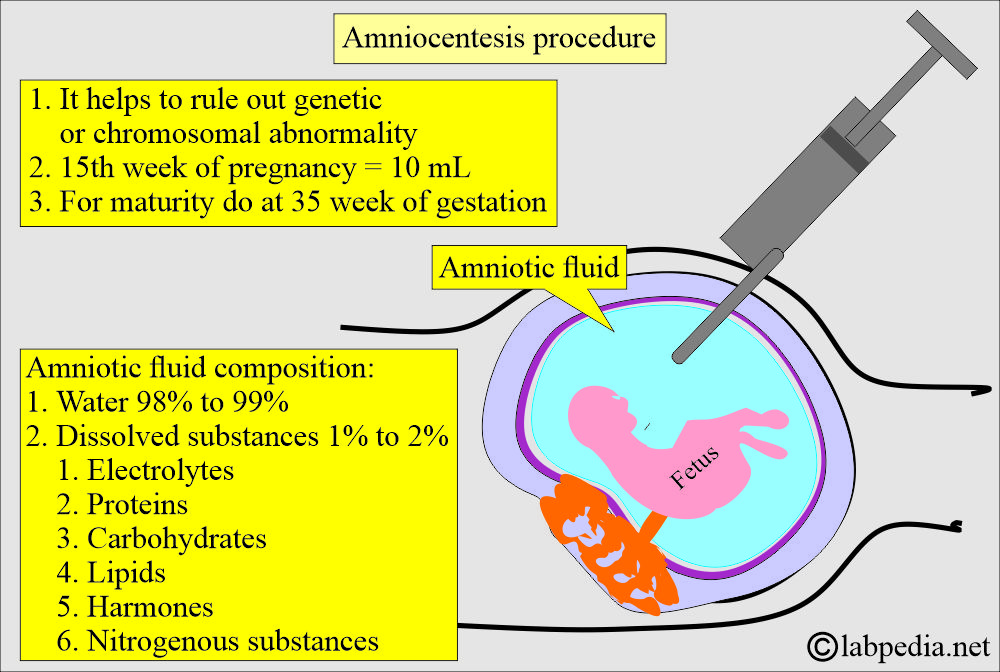
- Amniotic fluid is collected by amniocentesis.
- Amniotic fluid needs to be refrigerated.
- Avoid amniotic fluid from light for the estimation of bilirubin.
- Amniocentesis is done during the 14th, 16th, and 18th weeks of gestation.
- Chorionic villus sampling is better than amniotic fluid for karyotyping and genetic analysis.
What are the Indications for Amniotic fluid Examination (Amniocentesis)?
- To diagnose the genetic disorder (cytogenetics analysis).
- To diagnose chromosomal abnormalities.
- To diagnose inherited metabolic disorders like cystic fibrosis.
- To diagnose neural tube defects like myelomeningocele, anencephaly, and spina bifida,
- Measure bilirubin in Rh sensitization for erythroblastosis fetalis.
- To diagnose chorioamnionitis.
- To assess fetal lung maturity, a sample was taken after 32 weeks. The lecithin/sphingomyelin ratio is a measure of fetal lung maturity. Phospholipids are measured in amniotic fluids.
- To assess postmature pregnancy >40 weeks.
- To find intrauterine retardation.
- To find congenital infections like:
- Toxoplasmosis.
- Cytomegalovirus (CMV).
- It can do a culture for bacterial infections.
- Amniocentesis helps with an elective abortion in a defective fetus.
- To diagnose respiratory distress syndrome (RDS). This is a complication in premature newborns.
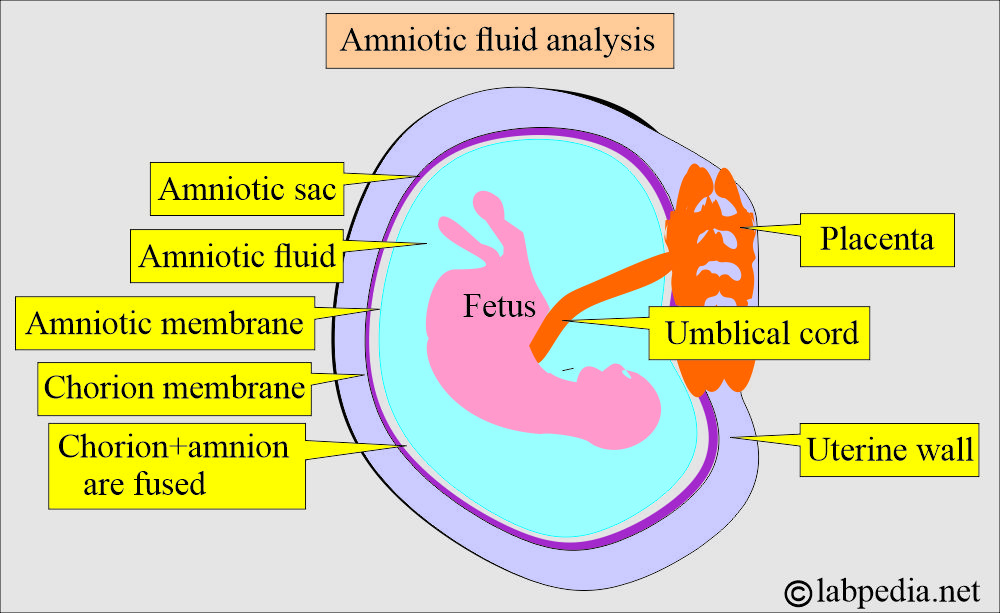
How will you define amniotic fluid?
- Amniotic fluid is the fluid in the amniotic sac that surrounds the fetus.
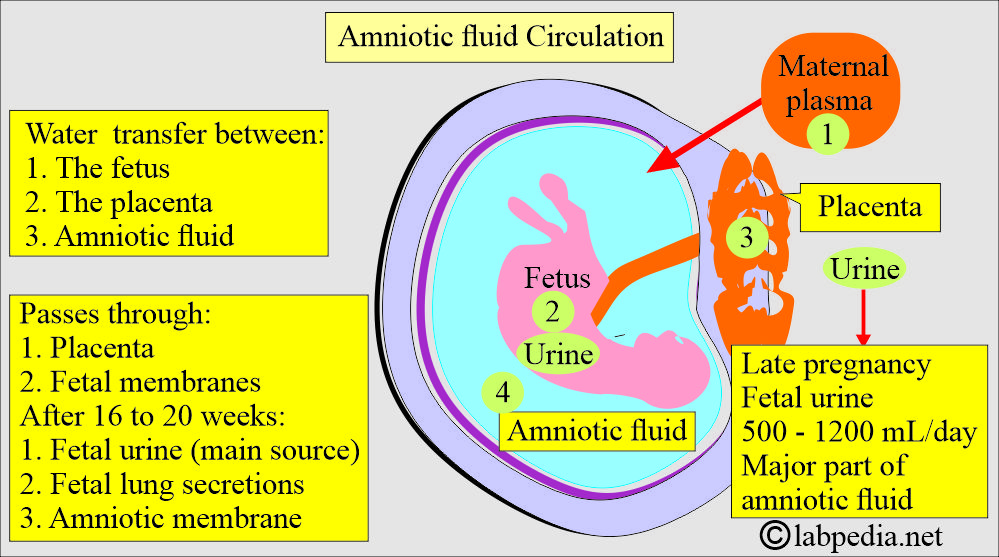
- A portion of the amniotic fluid arises from the fetal respiratory system, urine, the amniotic membrane, and the umbilical cord.
- Amniotic fluid at term is 500 to 1100 mL.
How will you discuss the pathophysiology of Amniotic fluid?
- Amniotic fluid is present in the amniotic sac, a membranous sac surrounding the fetus.
- Formation of amniotic fluid:
- Amniotic fluid arises from:
- Fetal respiratory tract.
- Urine.
- From the amniotic membrane.
- From the umbilical cord.
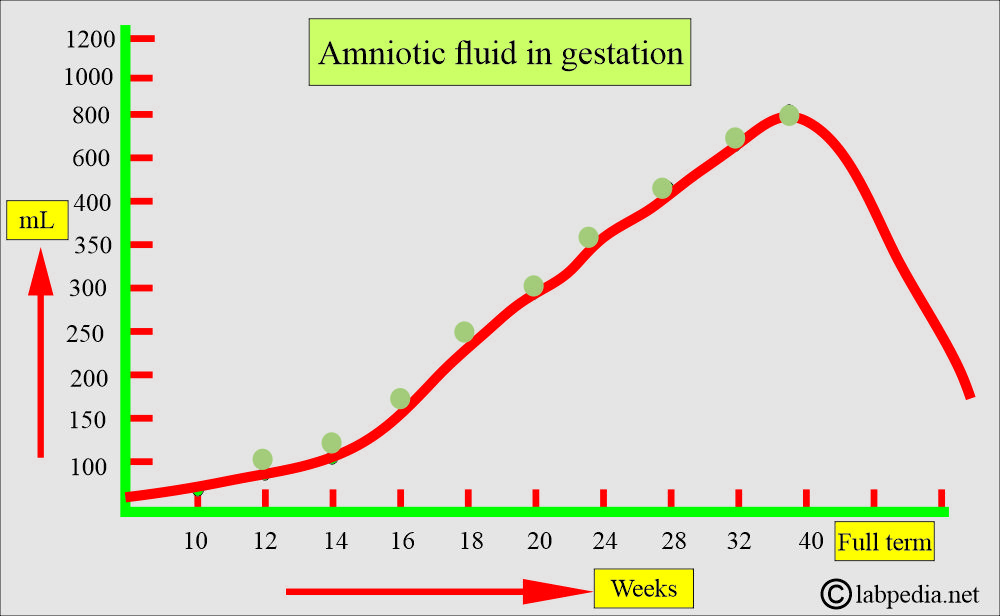
- Amniotic fluid keeps increasing throughout the pregnancy and reaches a peak of around one liter (1 L) during the third trimester.
- It gradually decreases before delivery.
- Around 30 mL of the amniotic fluid is derived from the maternal circulation during the first trimester. Its composition is similar to that of the mother’s plasma, with the addition of fetal cells. These cells may provide the basis for cytogenetic analysis.
- After the first trimester, fetal urine is the major contributor to the amniotic fluid volume.
- Now, fetal swallowing of amniotic fluid begins, and it regulates the increase in the fluid from the fetal urine.
- How will you describe Hydramnios?
- If there is a failure to swallow amniotic fluid, it will cause amniotic fluid to accumulate around the fetus, called Hydramnios.
- This will lead to fetal distress, which is usually seen in neural tube defects.
- It will occur in 1% of pregnancies.
- This may occur in diabetic mothers.
- How will you describe Oligohydramnios?
- It is decreased amniotic fluid seen with increased fluid swallowing, urinary tract abnormalities, and membrane leakage.
- This may occur due to abnormalities in the maternal, fetal, or placental compartments.
How will you describe the amniotic fluid composition?
- In early pregnancy, amniotic fluid is produced by the amniotic membrane covering the placenta and umbilical cord.
- It changes when urine formation starts.
- With the advance of pregnancy, amniotic fluid is a by-product of fetal pulmonary secretion, urine, and metabolic products from the intestinal tract.
- Initially, amniotic fluid is produced by the amniotic membrane and later by the maternal blood.
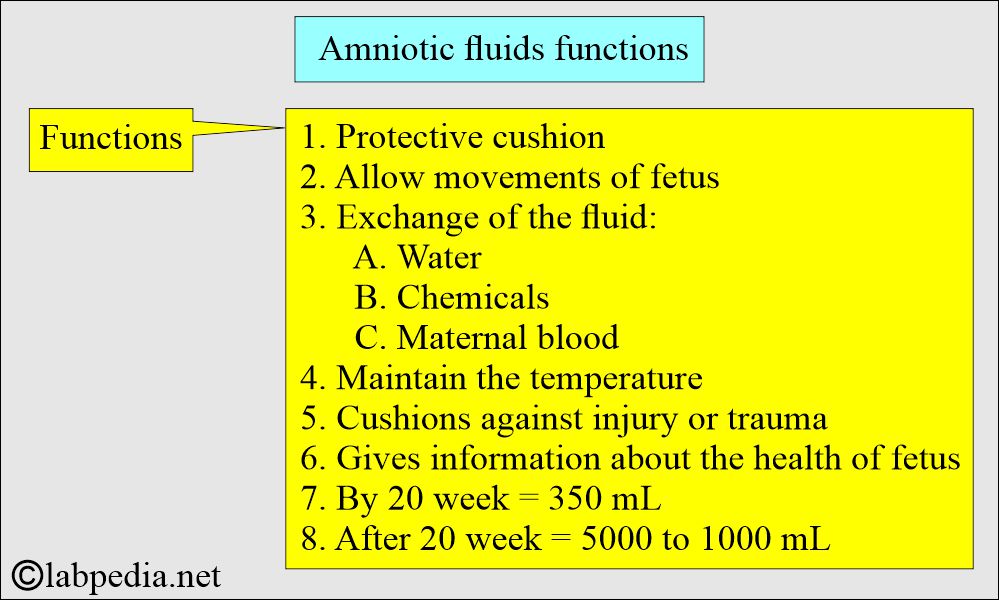
- Initially, the volume from 30 mL increases to 350 mL by the 20th week of gestation.
- After 20 weeks, the amniotic fluid volume varies from 500 mL to 1000 mL.
- Creatinine, urea, and uric acid concentrations increase while glucose and protein concentrations decrease.
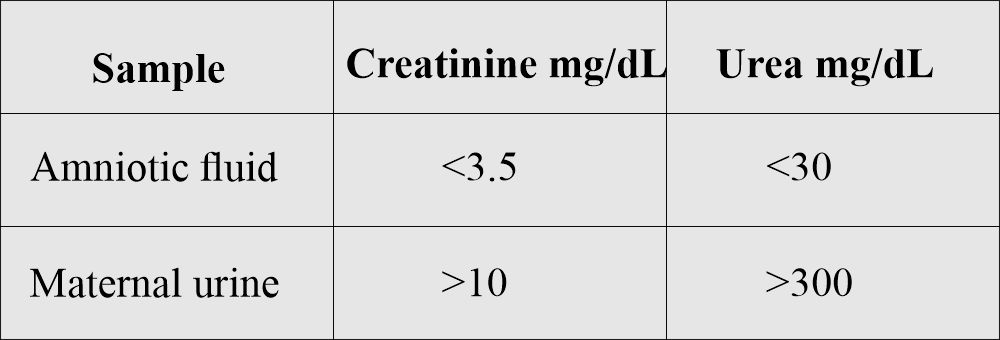
- The concentration of urea and creatinine is much lower in the amniotic fluid than in the maternal urine.
- Amniotic fluid contains albumin, urea, uric acid, creatinine, lecithin, sphingomyelin, bilirubin, fats, fructose, epithelial cells, leucocytic enzymes, and lanugo hairs.
How will you differentiate between amniotic fluid and maternal urine?
What are the functions of amniotic fluid?
- Amniotic fluid surrounds, protects, and nourishes the fetus during gestation.
- A part of the amniotic fluid is derived from:
- The fetal respiratory system.
- Amniotic membrane.
- Urine.
- Umbilical cord.
- A fetus can move freely in the amniotic fluid of the uterus.
- Amniotic fluid provides cushioning to the fetus from trauma and injury.
- This will prevent the compression of the umbilical cord.
- Amniotic fluid also maintains the temperature.
- Amniotic fluid provides information about the health and maturity of the fetus.
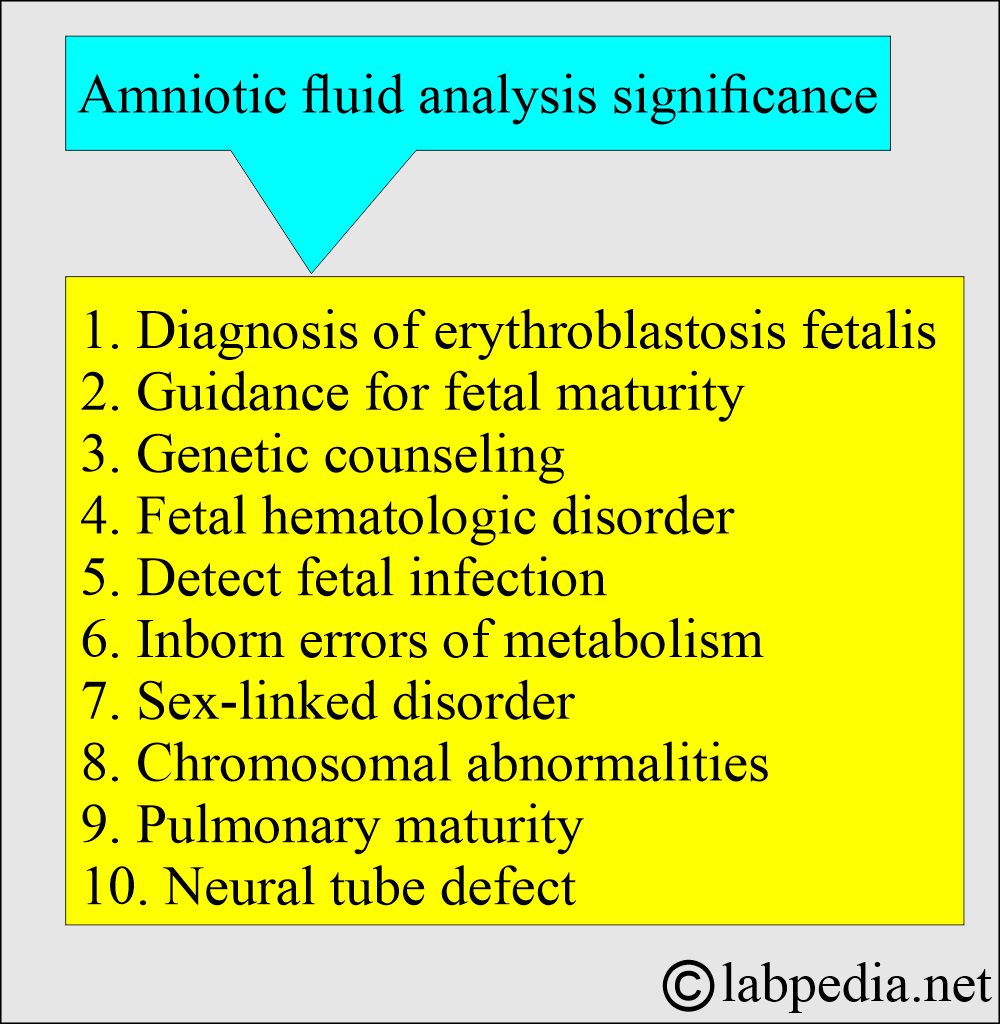
What is the significance of Amniotic fluid analysis?
- It can diagnose erythroblastosis fetalis, fetal maturity, and genetic counseling.
- It also diagnoses so many other abnormalities.
What are the important facts about Amniotic fluid?
- Amniotic fluid contains protein, hormones, nutrients, and antibodies.
- There is water transfer between intrauterine compartments:
- The placenta.
- The fetus.
- Amniotic fluid.
- As pregnancy (gestation) advances, there are changes as follows:
- After 25 weeks, there is an increase in amylase, alkaline phosphatase, urea, uric acid, creatinine, and phospholipids.
- There is a decrease in chloride, bilirubin, protein, glucose, and sodium.
- An elevated AFP level suggests neural tube defects, while a decreased AFP level is associated with an increased risk of trisomy 21.
- Amniocentesis helps with an elective abortion in a defective fetus.
What is the volume of amniotic fluid during pregnancy?
| Age of pregnancy | Volume of amniotic fluid |
|
50 mL |
|
400 mL |
|
800 mL |
|
1000 mL maximum |
|
800 mL |
What is the importance of the lecithin/sphingomyelin (L/S) ratio in amniotic fluid?
- It measures fetal lung maturity.
- Lecithin is the major surfactant required for alveolar ventilation. In the case of a deficiency of surfactant, alveoli collapse during expiration and lead to respiratory distress syndrome(RDS).
- There is an increased concentration of lecithin between 32 weeks and full-term babies, and there is a slight decrease in the sphingomyelin during the same period.
- Sphingomyelin is not a surfactant and has no role in lung maturity.
- This may be a major cause of death in immature babies. As the L/S ratio decreases, the risk of RDS increases.
- This test is very cumbersome.
- An L/S ratio value of 2.0 indicates lung maturity.
- L/S ratio of <2.0, newborns may not develop RDS.
How will you summarize the L/S ratio?
| L/S ratio | L/S ratio by various labs | Maturity of the lung |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What is the importance of Phosphatidylglycerol (PG) in amniotic fluid?
- This is the minor lung surfactant of about 10%. This is entirely synthesized by mature alveolar cells in the lung, which is a good indicator of lung maturity.
What is the importance of the bilirubin level in amniotic fluid?
- Analysis of the amniotic fluid for bilirubin level (or absorbance at 450), in the Rh-negative mothers in later weeks of gestation gives the severity of anemia due to Rh-incompatibility.
- Lilly plotted the graph to show the severity of hemolytic anemia.
How will you perform the amniotic fluid collection (amniocentesis) procedure?
- The needle from the amniotic sac, which aspirates amniotic fluid, is called amniocentesis.
- This is a transabdominal procedure (amniocentesis).
- Another route is transvaginal amniocentesis. This method carries a great risk of infection.
- The first 2 to 3 ml collected is discarded because it may be contaminated with maternal blood, tissue fluid, and cells.
- 30 mL of amniotic fluid is collected in sterile syringes.
- This procedure is safe if performed after the 14th week of gestation.
What is the best time when you will collect amniotic fluid?
- Fluid for chromosomal analysis is collected after the 16th week of gestation.
- In case of fetal distress and maturity is collected in the 3rd trimester.
- In the case of hemolytic disease of the newborn, the sample should be kept away from light. The sample should be kept in an amber-colored bottle or test tube.
- The fetal lung maturity sample should be placed on ice for transport to the laboratory and kept in the fridge.
- The cytogenetics sample may be stored at room temperature (37 °C) prior to analysis.
- The sample for biochemical testing should be separated immediately from cellular elements and debris to avoid the effects of cellular metabolism.
What are the Complications of the amniocentesis procedure?
- There may be a miscarriage.
- There are chances for injury to the fetus.
- There may be a leak of amniotic fluid.
- There are chances for abortion.
- There are chances for premature labor.
- There are chances of infections.
- There may be an amniotic fluid embolism.
- There is a risk of maternal Rh isoimmunization.
- There may be damage to the urinary bladder or intestine.
What are the precautions and contraindications of amniocentesis?
- Fetal blood contamination can cause a falsely elevated AFP level.
- Do not perform this test in case of:
- Placenta previa.
- Patients with placenta abruptio.
- Patients with an incompetent cervix.
- Patient with a history of premature labor.
What are the normal values of the amniotic fluid?
The mean volume of amniotic fluid during gestation:
| Weeks of gestation | Quantity of fluid |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Source 2
- 15 weeks of gestation = 450 mL of amniotic fluid
- 25 weeks of gestation = 750 mL of amniotic fluid
- 30 to 35 weeks of gestation= 1500 mL of amniotic fluid
- Full-term = <1500 mL of amniotic fluid
How will you summarize the normal Amniotic Fluid findings?
| General test | Result |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are the abnormal amniotic fluid findings?
| Lab findings | Findings | Clinical significance |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you interpret the amniotic fluid analysis?
- Hemolytic anemia shows increased bilirubin.
- Rh immunization also shows increased bilirubin.
- An elevated AFP indicates a neural tube defect. Acetylcholinesterase can confirm the diagnosis.
- AFP may also be raised in Sacrococcygeal teratoma.
- Fetal distress: The presence of meconium gives a greenish color to amniotic fluid, indicating fetal distress.
- Can diagnose an immature fetal lung.
- Can diagnose Hereditary metabolic disorders like cystic fibrosis, Tay-Sachs disease, and galactosemia.
- Can diagnose Sex-linked disorders like hemophilia.
- Genetic abnormalities like sickle cell anemia, thalassemia, and Down syndrome are diagnosed.
- Polyhydramnios (>2000mL) seen in diabetic patients increases the chances of congenital abnormalities.
- Oligohydramnios when the amniotic fluid is less than 300 mL at 25 weeks of gestation. This is associated with fetal renal disease.
- A genetic disorder is identified by the amniotic fluid analysis.
What are the Chromosomal anomalies diagnosis?
|
|
|
|
|
|
|
|
|
|
What are the critical values of amniotic fluid analysis?
Bilirubin level = It is increasedin hemolytic diseases of the newborn.
Lecithin/sphyngomylein ratio (L/S) = <2.0
Chromosomal abnormalities = Can diagnose various congenital (genetic) abnormalities.
Abnormal metabolites = Diagnose various diseases
Questions and answers:
Question 1: What is the main function of amniocentesis?
Question 2: What is the amount of amniotic fluid at 28 weeks of gestation?