Fluid Analysis:- Part 4 – Ascitic fluid Abdominal Paracentesis Procedure
Abdominal Paracentesis Procedure
How will you get a sample of Ascitic fluid?
- The ascitic fluid is aspirated from the peritoneal cavity.
How will you define ascitic fluid?
- The collection of fluid in the peritoneal cavity is called ascites and ascitic fluid.
What are the indications for Ascitic fluid?
- An abdominal tap is done on the patient who has unexplained ascites.
- An abdominal tap is done to relieve the intraabdominal pressure.
- To diagnose whether ascites are benign or due to malignancy.
- An abdominal tap is helpful to differentiate between the medical and surgical abdomen.
- Abdominal fluid differentiates between Transudate and Exudate.
- The abdominal fluid is removed for diagnostic and therapeutic purposes.
What are the precautions for abdominal paracentesis?
- Do not perform in case of DIC.
- Avoid in case of pregnancy.
- Do not perform in the organomegaly.
- Avoid in case of intestinal obstruction.
- Do not perform in case of a distended urinary bladder.
- Avoid when there is a need for surgery on an acute abdomen.
- Avoid when the platelets are below 20,000/cmm, or INR is >2.
How will you discuss the pathophysiology of ascitic fluid?
- The peritoneal cavity is the space between the visceral and parietal peritoneum.
- The peritoneal membrane constantly produces the fluid and is reabsorbed by the same membrane, containing a network of capillary and lymphatics.
- If the secretion is increased or reabsorption is decreased, that will lead to peritoneal fluid collection (Ascites).
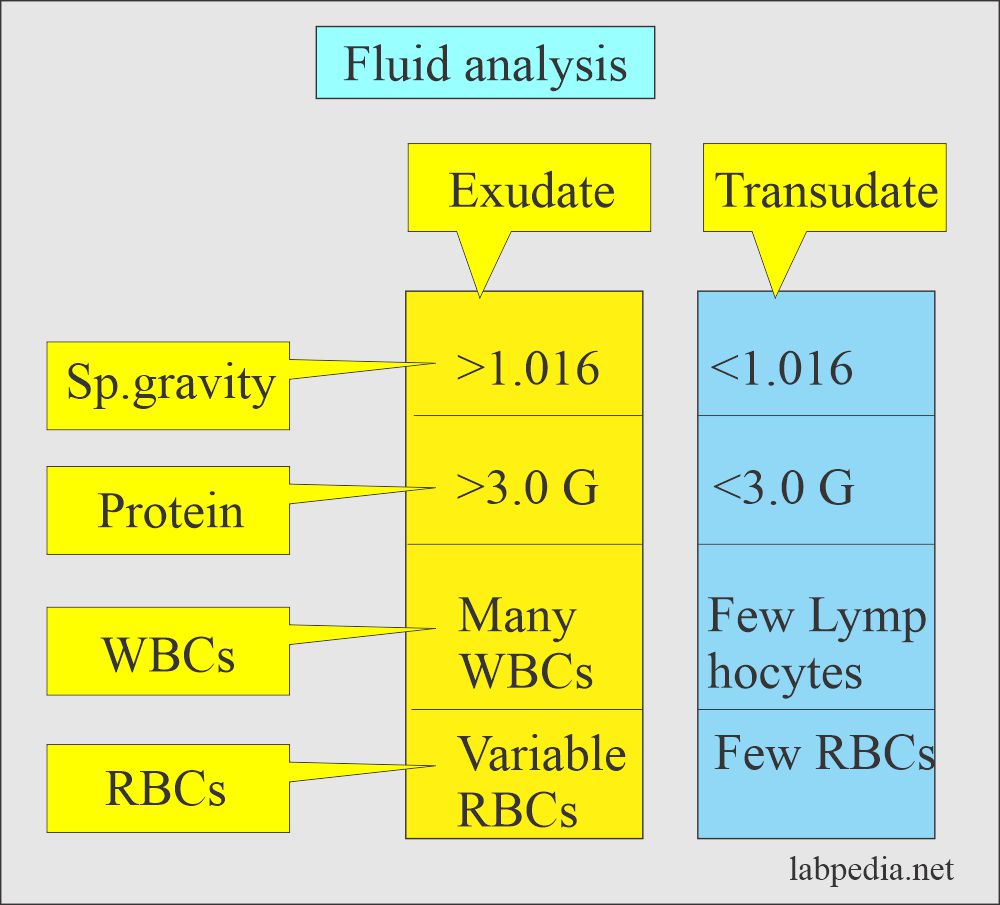
- The abdominal fluid is classified as Transudate when the protein is less than 3 G /dl or Exudate when the protein is more than 3 g/dl.
- Transudate is caused by congestive heart failure, cirrhosis, nephrotic syndrome, myxedema, hypoproteinemia, peritoneal dialysis, and acute glomerulonephritis.
- Exudate is found more commonly in inflammation and malignancy. While some other conditions of drug hypersensitivity, pulmonary infarction, GIT diseases, and collagen diseases may form exudate.
How will you do the Procedure for ascitic fluid tap (Paracentesis)?
- This is an invasive procedure.
- Ensure that the patient’s urinary bladder is empty.
- The position is semi-prone and lateral.
- Raise the bedhead side so that fluid accumulates in the lower abdomen.
- First, sterilize the area. Clean the area with 70% isopropanol and allow it to dry the area.
- If needed, can give local anesthesia. Raise the area with local anesthetic and make the small bleb from where the needle can be inserted.
- Locate the area with percussion where there is dullness, indicating fluid.
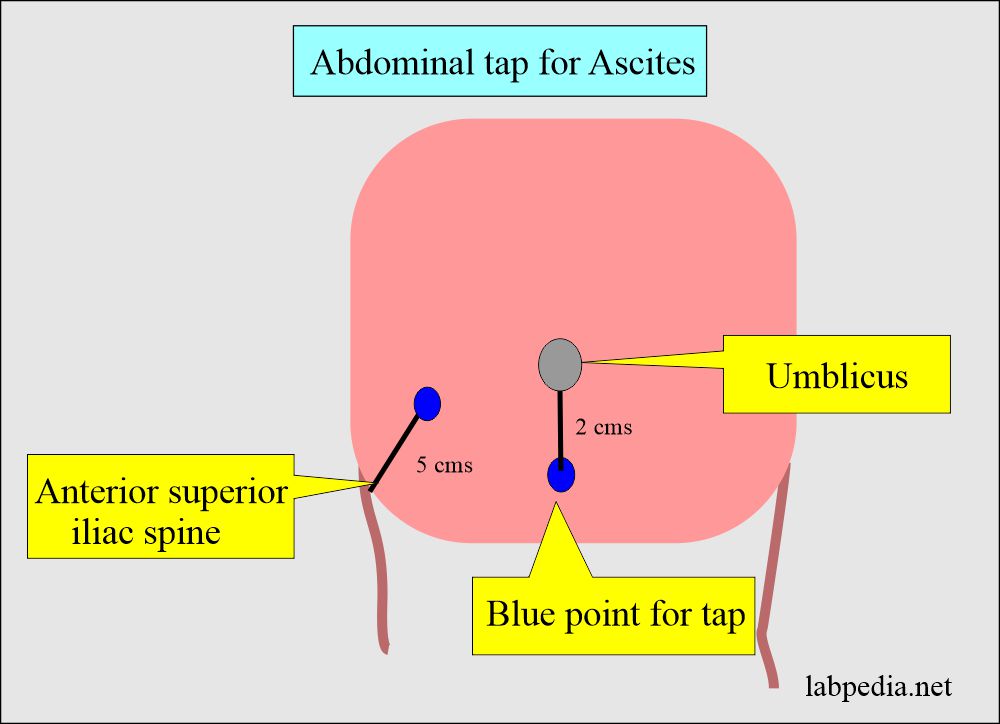
- Insert needle 5 cm superior and medial to the anterior superior iliac spine.
- Or 2 cm below the umbilicus.
- A needle 20 or 18 gauge is inserted into the abdominal cavity lateral to the umbilicus with constant negative pressure in the syringe till you see the fluid.
What are the complications of ascitic fluid tap (Paracentesis)?
- Hypovolemia and hypotension may occur if a large volume of the ascitic fluid is aspirated.
- There is a risk of peritonitis.
- Do not perform in case of DIC.
- Do not perform in case of acute abdomen.
- Leakage at the site needle insertion.
- Abdominal wall hematoma or bleeding.
- There may be spontaneous hemoperitoneum.
- Subcutaneous effusion due to ascitic fluid leakage.
What are the normal features of ascitic fluid?
| Characteristics | Findings |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What are Ascites (peritoneal fluid) findings in various diseases?
- Gross or physical appearance:
- Grossly peritoneal fluid is clear and light yellow with <50 ml volume.
- No RBCs are seen.
- White blood cells are <300 /cmm
- Transudate fluid will be clear and straw in color.
- Chylous color fluid: This is seen in blocked lymphatic vessels, and the color is milky.
- This may be seen in lymphoma, carcinoma, and tuberculosis.
- In such fluids, triglyceride value is > 110 mg/dl.
- The inflammatory condition gives rise to a turbid or opaque color. This may be seen in peritonitis, pancreatitis, and appendicitis.
- The hemorrhagic color is due to trauma or intraabdominal bleeding, tumor infiltrates, or hemorrhagic pancreatitis.
- Greenish color or bile-stained fluid is seen in the ruptured gallbladder, acute pancreatitis, or in intestinal perforation.
- Bloody fluid may be due to the following:
- Traumatic tap.
- Hemorrhagic pancreatitis.
- Tumors.
- 10,000 RBCs/ µL will give a pink color.
- 20,000 RBCs/ µL will give the bloody appearance.
- Grossly peritoneal fluid is clear and light yellow with <50 ml volume.
- Specific gravity:
- Exudate has a specific gravity of more than 1.015, and less than 1.015 in transudate.
- Proteins:
- Transudate has less than 3 g/dl, and exudate has more than 3 g/dl of protein.
- The ratio of serum protein and ascitic fluid protein is more significant in differentiating exudate from transudate (Fluid protein/serum protein).
- A ratio of more than 0.5 is diagnostic of exudate.
- The albumin gradient between serum albumin and the ascitic fluid is also important to differentiate between exudate and transudate.
- Ascitic fluid albumin -(minus) serum albumin.
- A value 1.1 g/dL or more indicates transudate.
- Value <1.1 g/dL indicates exudate.
- Total Cell Count:
- This depends upon the cause of ascites.
- The count will be high in inflammatory conditions, and predominantly Polys are seen.
- In hemorrhagic conditions, the RBC count will be high.
- Differential count:
- The inflammatory conditions show more polys and reactive mesothelial cells, while transudate may show more lymphocytes. Malignant ascites also show more lymphocytes.
- RBC presence indicates malignancies, tuberculosis, or intra-abdominal bleeding.
- WBCs presence indicates peritonitis, tuberculosis, or cirrhosis.
- Cytology:
- This can be done better on cytospin preparation, can differentiate the cells, and can find the malignant cells.
- Sometimes, reactive mesothelial cells and malignant cell differentiation are difficult.
- Malignant cells have variable morphology of the cells and nuclei. There is chromatin clumping, which changes the nuclear/cytoplasmic ratio. May see prominent nucleoli.
- Glucose:
- Glucose level may be done, usually equal to blood glucose level.
- However, in tuberculous and bacterial ascites, it is low.
- It is low in peritoneal carcinomatosis.
- Amylase:
- This will be raised in:
- Pancreatic trauma.
- Acute pancreatitis.
- Intestinal necrosis.
- Intestinal Perforation or strangulation.
- Pancreatic pseudocyst.
- Lactate dehydrogenase (LDH):
- It is diagnostic for exudate if the ascites LDH/serum LDH ratio is greater than 0.6.
- The alkaline phosphatase:
- Its level is greatly increased in infarction or the strangulation of the intestine.
- Ammonia:
- Its raised level is seen in the following:
- Ruptured or strangulated intestine.
- Ruptured appendix.
- Its raised level is seen in the following:
- Gram stain:
- This may be performed, but culture and sensitivity are usually advised.
- Fungal infection:
- Fungal infection is usually seen with histoplasmosis, candidiasis, or coccidioidomycosis.
- Carcinoembryonic antigen (CEA):
- CEA is seen in the case of GIT malignancies.
How will you interpret abnormal ascitic fluid?
| Physical appearance | Significance |
|
|
|
|
|
|
|
|
|
|
| Biochemical findings | |
|
|
|
|
|
|
|
|
|
|
|
|
| Microscopic findings | |
|
|
|
|
|
|
|
|
- Note: Please see more details in Fluid Analysis Part 2.

Perfect presentation and very informative knowledge
Thanks for the encouraging remarks.
Yes, I love this place
Thanks.
Very interesting and simple to understand presentation.
Thanks,
Thanks.
Sir, Great effort!
Thanks.