Fibrinogen (Factor 1), Acute Phase Protein
Fibrinogen (Factor 1)
Acute-phase protein (Acute Phase Reactants)
- Acute-phase proteins are elevated in inflammatory conditions.
- Acute-phase proteins (positive) are plasma proteins whose concentrations increase during disease and, after the disease episode, decrease and may return to normal
- When there is an increase in a protein called a positive acute-phase protein.
- A decrease in an acute-phase protein is called a negative-phase protein..
Fibrinogen (Factor 1)
What sample is needed for Fibrinogen (Factor 1)?
- The patient’s blood is needed to prepare plasma.
- The sample is stable for 8 hours at room temperature.
- It can be stored for several months at -20 °C.
What are the indications for Fibrinogen (Factor 1)?
- For the evaluation of bleeding disorders.
- If there is excessive bruising.
- In case of bleeding from the gums and nose.
- In the case of bleeding in the GIT and blood in the stool.
- In the case of blood in the urine.
- If there is a rupture of the spleen.
What are the precautions for Fibrinogen (Factor 1)?
- Avoid clot formation.
- Avoid collecting blood from the heparinized blood vessel.
- Avoid contamination with tissue that contains tissue thromboplastin.
- Avoid contamination with heparin.
- Blood transfusion in the last month may affect the result.
- A diet rich in Omega-3 and Omega-6 fatty acids reduces the level of fibrinogen.
- Oral contraceptives and estrogen increase the level.
- Drugs like anabolic steroids, phenobarbital, streptokinase, valproic acid, and asparaginase.
How will you discuss the pathophysiology of Fibrinogen (Factor 1)?
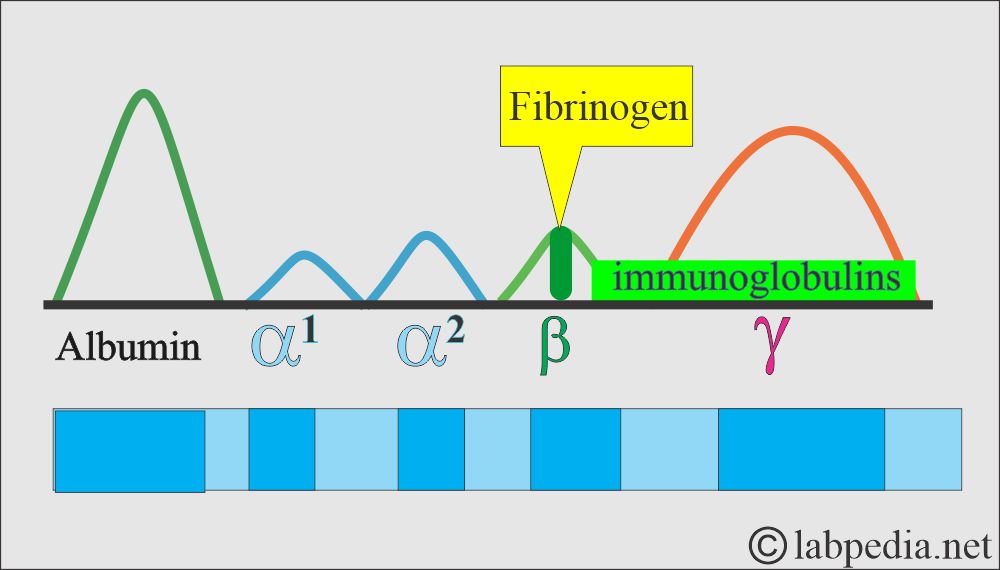
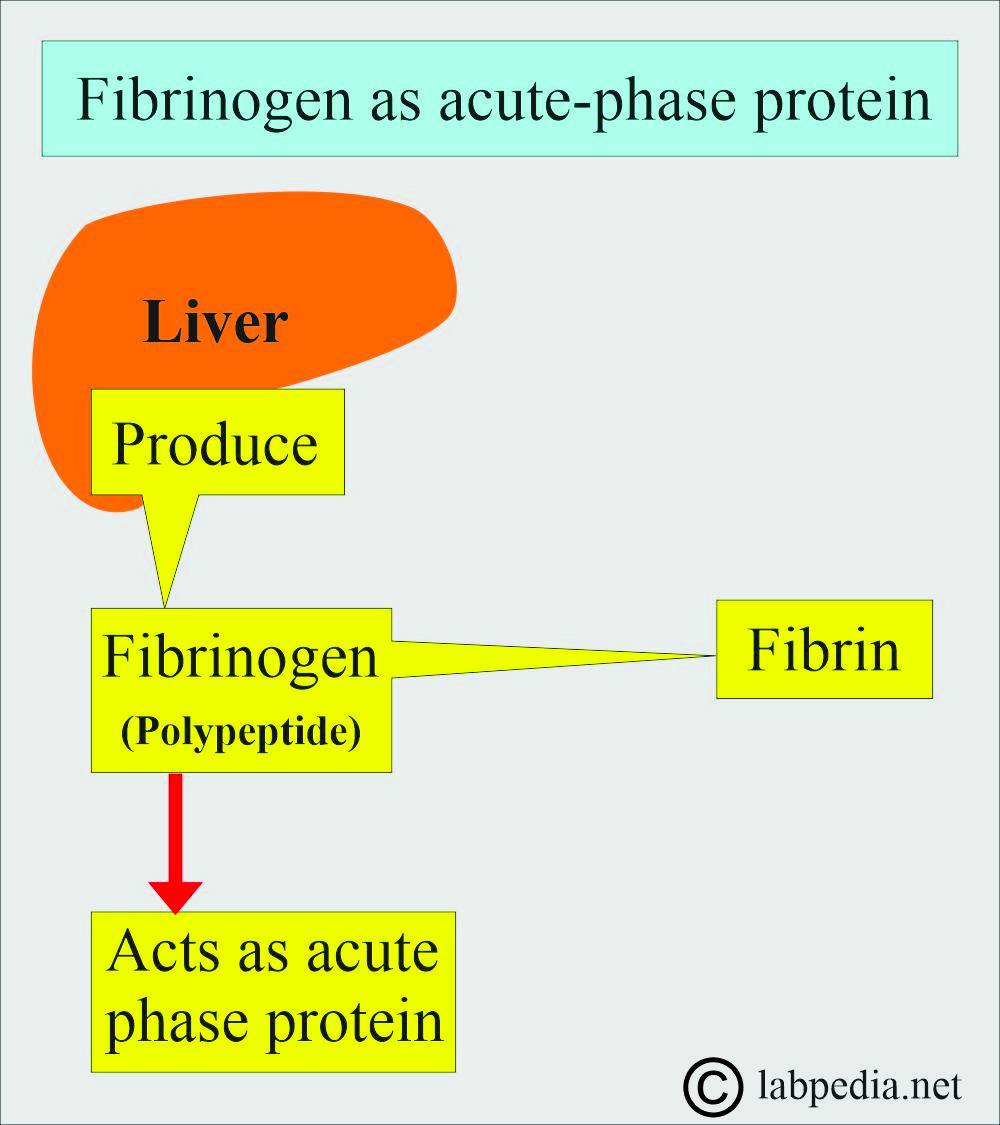
- Fibrinogen (factor 1) is an acute-phase protein.
- This is β-globulin and is usually absent from the serum.
- It is a fibrillary group of glycoproteins.
- This consists of three pairs of polypeptide chains.
- It is synthesized in the liver, the major source of coagulation factors.
- Fibrinogen may act as an acute-phase protein.
What will happen when fibrinogen is transfused?
- 50% disappear in 48 hours.
- 75% disappear in 6 days.
- Half-life is 3.5 to 4 days. (Another source says 100 to 150 hours).
- This is an essential protein for blood clot formation (30% activity for normal coagulation is required).
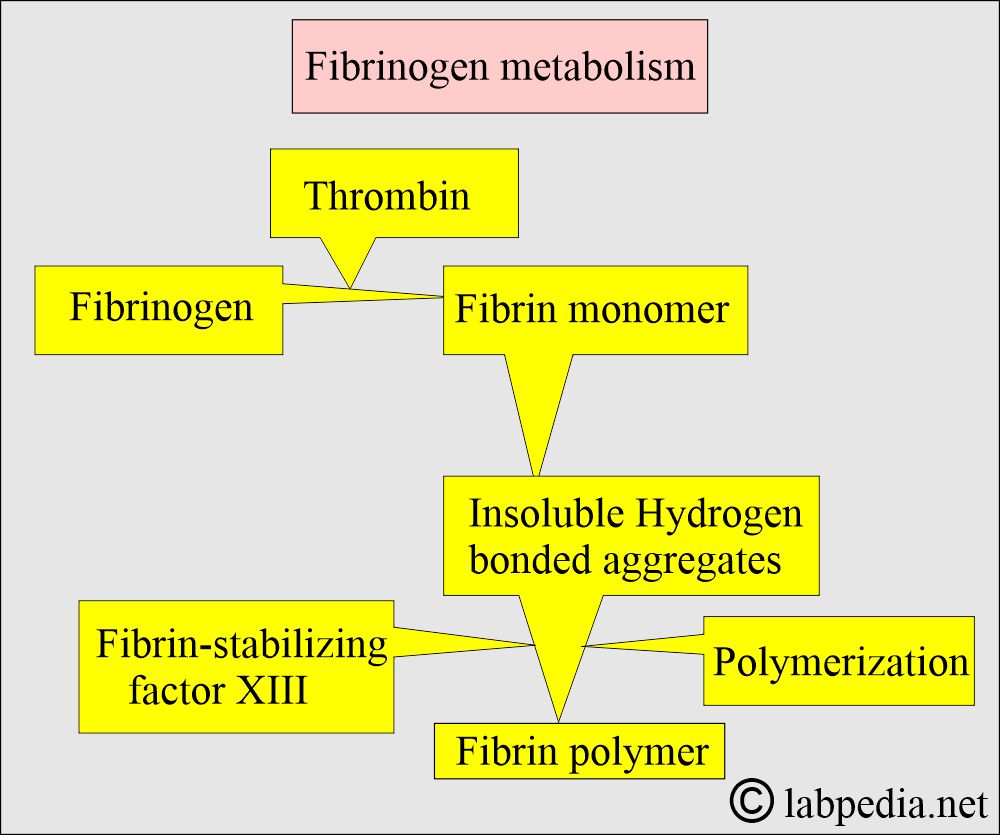
- It is a complex protein with enzymatic action that is converted into fibrin.
- In the clotting process, all the fibrinogen in the plasma is converted to fibrin.
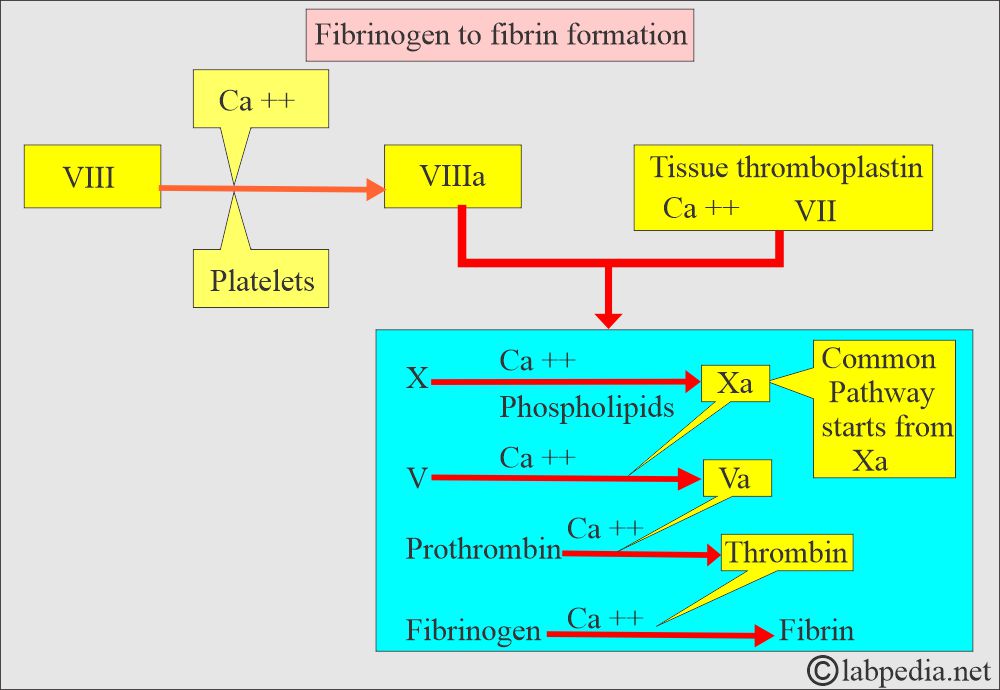
- Conversion of fibrinogen into fibrin is the final step in coagulation, and it takes place under the influence of thrombin.
- This is part of the common pathway in coagulation.
- The serum is lacking fibrinogen.
What are the facts about Fibrinogen (Factor 1)?
- The fibrinogen significantly affects RBC sedimentation rates by coating the cells.
- This allows the cells to settle (sediment) faster.
- So, increased fibrinogen indicates raised ESR.
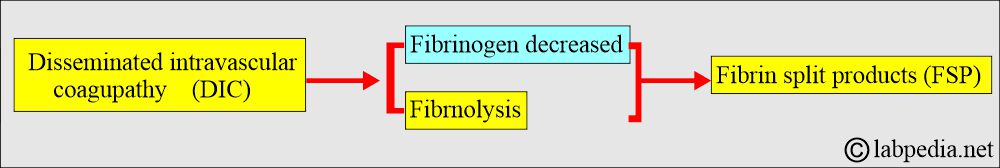
- Disseminated intravascular coagulopathy (DIC): In this case, fibrinogen is decreased.
- Fibrinogen is converted into fibrin under the influence of thrombin and is the final step in coagulation.
- This is raised by inflammation or tissue injury. Fibrinogen plays an important role in the body’s acute reaction in response to trauma or various severe diseases.
- It is a risk factor for coronary heart disease and stroke.
- Fibrinogen is decreased in DIC.
- Fibrinogen level increases with cigarette smoking.
- There is an influence of genetics.
- Snake venom leads to the depletion of fibrinogen.
What is the normal level of Fibrinogen (Factor 1)?
- Source 2
- Newborn = 125 to 300 mg/dL
- Adult = 200 to 400 mg/dL (2 to 4 g/L)
- Source 4
- 200 to 400 mg/dL (2 to 4 g/L)
- Another source
- 175 to 400 mg/dL.
What is the critical value of Fibrinogen (Factor 1)?
Critical value = <100 mg/dL.
- Another source: Critical value is <60 mg/dL.
What causes an increased level of Fibrinogen (Factor 1)?
- Acute infections.
- Myocardial infarction and Sudden cardiac death.
- Patients with malignancies.
- Inflammatory conditions like Rheumatoid arthritis and Glomerulonephritis.
- In the case of traumatic injury.
- Patient with a stroke.
- In pregnancy.
- People who are cigarette smokers.
- Patients with peripheral artery disease.
- This is raised in acute and chronic inflammation.
- Older age.
- Diabetes mellitus.
What is the association of increased fibrinogen levels?
- Coronary heart disease.
- Myocardial infarction.
- Stroke.
- Peripheral arterial disease.
What are the causes of decreased fibrinogen levels?
- Patients with severe liver disease.
- Consumptive coagulopathy like DIC.
- Malnourished patients.
- In case of a large volume of blood transfusion.
Afibrinogenemia:
How will you define Afibrinogenemia?
- This is rare and usually inherited as an autosomal recessive trait (congenital absence).
- If the parents do not show the disease, they can still pass it to their children.
- When 2 carriers of autosomal recessive positive parents have children, each child has:
- 25% chance to be affected.
- 50% chance to be an unaffected carrier.
- 25% chance to be unaffected and not a carrier.
- There is a severe lack of fibrinogen, and blood will not clot.
- What are the signs and symptoms of Afibrinogenemia?
- In the case of afibrinogenemia, if the fibrinogen level is <0.1 g/L, it will have bleeding abnormalities from mild to severe.
- This disease is present from birth.
- The first symptom is bleeding from the umbilical cord, which will not stop and is difficult to stop.
- There may be gastrointestinal bleeding.
- There may be nose bleeding (epistaxis) or bleeding from the oral mucosa.
- There may be bleeding episodes, bruises, and poor wound healing.
- Females may have excessive menstruation.
- There may be a spontaneous abortion.
- There may be a CNS hemorrhage.
- Evidence of bleeding in the joints.
- How will you diagnose Afibrinogenemia?
- The following tests are advised:
- Prothrombin time (PT). It is abnormal.
- Activated partial thromboplastin time (APTT) is abnormal.
- Bleeding time (BT) is prolonged in 1/3 of the cases.
- Fibrinogen level in the blood. Plasma fibrinogen is absent.
- Reptilase time.
- Thrombin time.
- Prolonged bleeding time and fibrinogen level <0.1 g/L, indicating afibrinogenemia.
Congenital hypofibrinogenemia:
- It is an inherited autosomal dominant abnormality.
- Plasma fibrinogen is mildly decreased and is usually <80 mg/dL.
- Bleeding time (BT) and coagulation time (CT) are normal.
- Blood clots are small.
Dysfibrinogenemia:
How will you define Dysfibrinogenemia?
- It is rarely inherited (autosomal dominant) or acquired, heterogeneous groups of diseases.
- There is abnormal fibrinogen due to a structural abnormality, which results in abnormal function.
- What are the types of Dysfibrinogenemia?
- This may be:
- Congenital or inherited, there is an increased risk of bleeding, thrombosis, or both in the same patient or family.
- Some of the patients are asymptomatic.
- The prognosis is good. The event of thrombosis and bleeding is mild.
- Acquired fibrinogen is dysfunctional due to autoimmune diseases, liver diseases, plasma cell dyscrasia, or cancers.
- There is more bleeding than thrombosis.
- The prognosis is worse because of liver disease.
- Congenital or inherited, there is an increased risk of bleeding, thrombosis, or both in the same patient or family.
What are the signs and symptoms of dysfibrinogenemia?
- This leads to a relatively mild hemorrhage if there is a congenital cause.
- >50% of the cases have no bleeding disorders.
- 20% to 25% of cases have mild to moderate bleeding, thrombosis, or both.
- Few of these may tend to thrombosis in case of an acquired cause.
- How will you diagnose dysfibrinogenemia?
- Prothrombin time (PT) is prolonged.
- Activated partial thromboplastin (APTT) is also prolonged.
- Thrombin time (TT) is the most sensitive test for dysfibrinogenemia in the case of bleeding tendency and may not be prolonged in the case of a tendency for thrombosis.
- Reptilase time is prolonged.
What is the value for the layman?
- This is advised when there is a history of bleeding or bruises.
- If the patient has epistaxis.
Questions and answers:
Question 1: What will happen to fibrinogen in case of snake bite?
Question 2: What is the critical value of the fibrinogen?

Excellent article about Fibrinogen!
Thanks for the comments.