Epstein-Barr virus (EBV), Infectious Mononucleosis
Epstein-Barr virus (EBV)
What sample is needed for Epstein-Barr virus (EBV)?
- The patient’s serum is needed.
What is the Indication for Epstein-Barr virus (EBV)?
- This test is done to diagnose Infectious Mononucleosis (EBV).
How will you explain the epidemiology of the Epstein-Barr virus?
- EBV is a herpes virus belonging to the herpesvirus family and is found worldwide.
- It was first diagnosed in 1964 as the causative agent of infectious Mononucleosis.
- It is estimated that 95% of the world’s population is exposed to this virus.
- In the USA, 80% or more of the population is infected.
- Once an infection occurs, the virus becomes dormant and can later reactivate into clinical disease.
- Reactivation occurs in 15% to 20% of healthy people and up to 85% in immunocompromised patients.
- In the USA, it is seen in a higher socio-economic group in later life and considered by social contact, the so-called “kissing disease,” because it can spread through saliva.
How will the EBV spread?
- It is through the oropharyngeal secretion.
- EBV is transmitted through saliva.
- This is also reported via blood transfusion and the transplacental route.
- It can also spread through organ transplantation.
- The incubation period is 4 to 6 weeks (or 10 to 50 days).
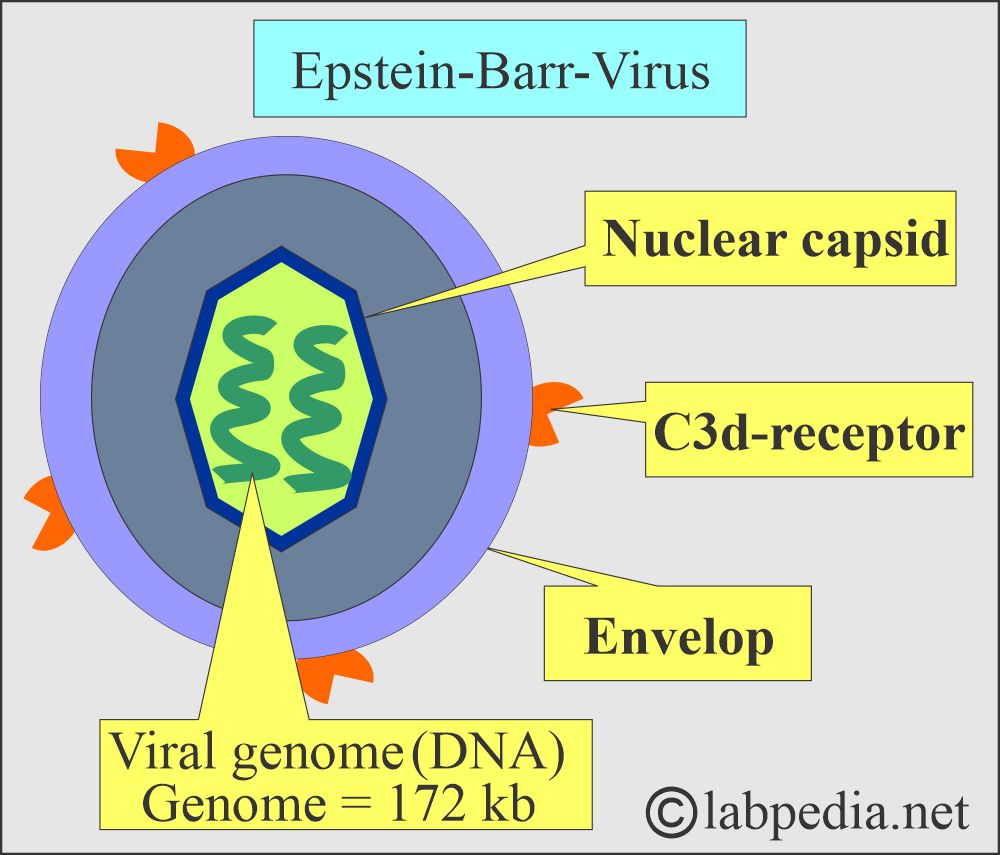
What is the morphology of the Epstein-Barr virus?
- There are two genomic types of EBV:
- EBV1. This one is more predominant in the West.
- EBV2. Meanwhile, EBV1 and EBV2 are distributed worldwide.
- It is 100 nm, double-stranded DNA, icosahedral, enveloped.
- EBV is an enveloped icosahedral virus containing a double-stranded DNAgenome of 172 Kb.
What is the mode of spread?
- It infects the B-lymphocytes.
- These B-lymphocytes, after the infection, look like T-lymphocytes.
- The habitat for the EBV is B-lymphocytes and epithelial cells of the oropharynx.
- EBV is a lymphotropic virus.
- EBV is a member of the herpes virus family.
- This virus usually affects young adults.
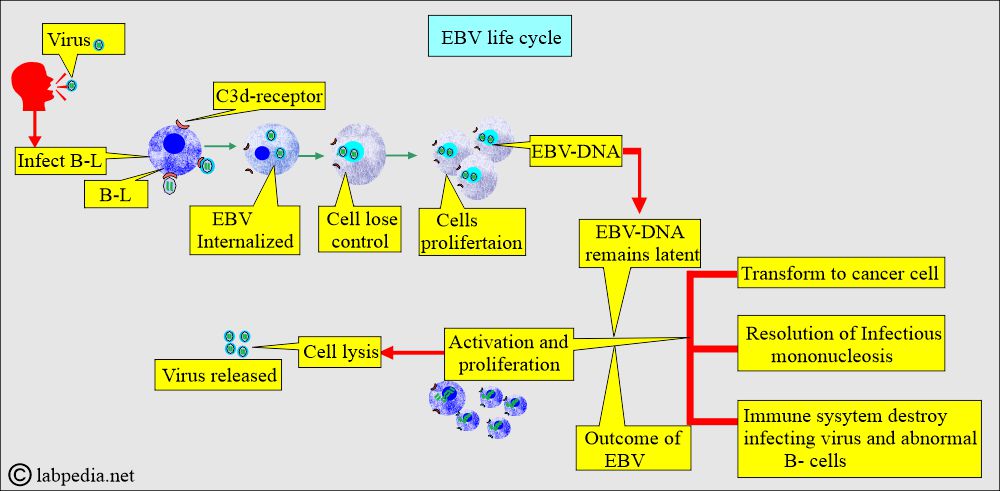
How will you explain the Epstein-Barr virus (EBV) life cycle?
- EBV virus enters through the pharyngeal mucosa and then infects the B-lymphocytes.
- The EBV enters the B-lymphocytes through the presence of C3d receptors.
- Once it is internalized, the cell loses control.
- There is cellular proliferation.
- EBV becomes part of the DNA and remains latent as EBV-DNA.
- Later, the EBV-DNA cell is activated and begins proliferating.
What is the outcome of the EBV infection?
- Now, there are possibilities:
- Cells transform into cancer cells.
- There may be a resolution of the infectious Mononucleosis.
- The immune system destroys the infecting virus and abnormal B-lymphocytes.
- Or there is cell lysis, and the viruses are released.
- The patient develops IgM antibodies against the EBV viral capsid, usually after 2 weeks of the disease.
- These antibodies readily bind to and agglutinate horse RBCs.
What is the Normal Epstein-Barr virus (EBV) profile?
Source 6
- EBV titer = ≤1:10 is nondiagnostic.
- An EBV titer of 1:10 to 1:60 indicates infection at some undetermined time.
- An EBV titer of ≥1:320 suggests active infection.
- A fourfold increase in titer in paired sera drawn 10 to 14 days apart usually indicates an acute infection.
- Heterophil (sheep RBC) antibody titer: <1:112 (in a normal person).
Infectious Mononucleosis
How will you describe the clinical presentation of Infectious Mononucleosis?
- Primary infection with EBV in older children, adolescents, or young adults produces Infectious Mononucleosis syndrome in around 50% of cases.
- The patients with Infectious Mononucleosis are mostly adolescents and young adults. But this may be seen in older children, middle-aged adults, and older adults.
- In the case of primary infection in infectious mononucleosis, the incubation period is:
- 3 to 7 weeks.
- The acute phase of this disease in symptomatic patients lasts 2 to 3 weeks.
- The convalescent stage reaches in 4 to 8 weeks.
- The majority have no signs or symptoms.
- Infectious Mononucleosis may be seen as:
- Acute.
- Chronic.
- This is a benign disease.
- This is a self-limiting disease.
- In children under 5 years of age, the disease is very mild.
- This is also seen in adolescents and young adults.
- After 10 to 50 days of incubation, the disease lasts 1 to 4 weeks.
- The most common signs and symptoms are:
- Pharyngitis and sore throat.
- Soft palate petechiae are seen in 10% to 30% of cases.
- Fever.
- Fatigue, malaise.
- Exudative tonsillitis is often the presenting feature of the generalized viral infection due to Epstein-Barr virus, the so-called anginose form of infectious Mononucleosis.
- Enlargement of the cervical lymph nodes is seen. Lymph node involvement may be seen in 80% to 90% of cases.
- Splenomegaly is seen in 50% of the cases.
- Jaundice is less common. This is usually mild and seen in 5% to 10% of cases.
- This also causes oral hairy leukoplakia.
- The most common complication is hepatitis.
- What are the complications?
- A few patients may show hepatomegaly. This may be seen in only 10% of the cases.
- This is associated with Burkitt’s lymphoma and nasopharyngeal carcinoma.
- There may be B-cell lymphoma in the immunocompromised patient.
- Most patients recover uneventfully and attend regular activities within 4 to 6 weeks.
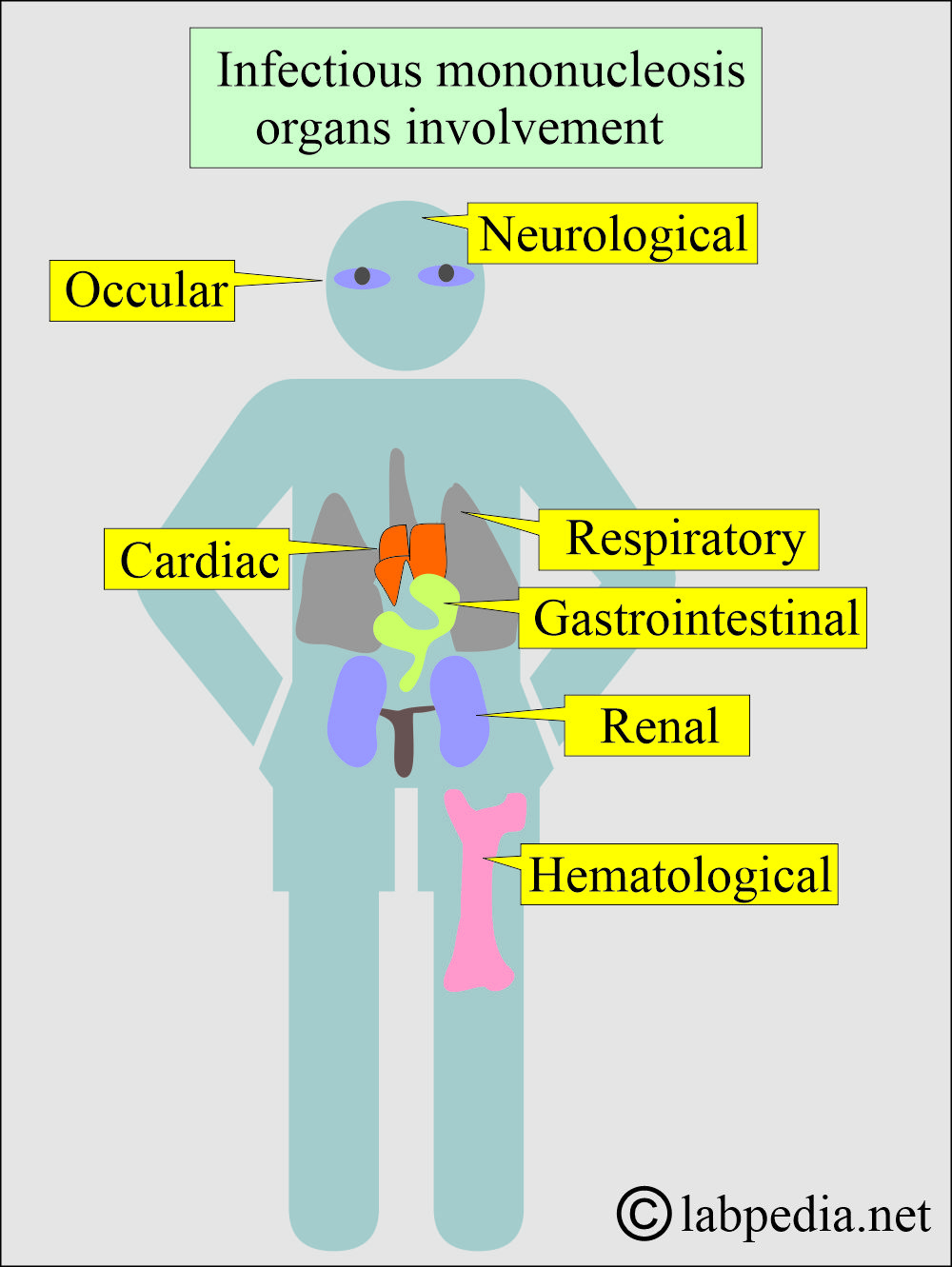
What are the complications of infectious Mononucleosis?
- Cardiac.
- Ocular.
- Hematological.
- Renal.
- Gastrointestinal.
- Neurological. This may lead to Bell’s palsy, meningoencephalitis, Guillain-Barré syndrome, cranial nerve neuritis, myelitis, and psychotic disorders.
- Respiratory.
What are Chronic EBV signs and symptoms?
- In some cases, there may be nonspecific symptoms.
- There may be severe fatigue (chronic fatigue syndrome).
- Pharyngitis.
- Myalgia.
- Arthralgia.
- Low-grade fever.
- Headache.
- Paresthesia.
- There is a loss of skilled thinking.
What is the association of Infectious Mononucleosis with malignancies?
- In Africa, Burkitt’s lymphoma.
- In China, with nasopharyngeal carcinoma.
- Nasal T/NK-type lymphoma.
- Some subtypes of Hodgkin’s lymphoma.
How will you diagnose Epstein-Barr virus (EBV) and Infectious Mononucleosis?
- Hemoglobin is mostly normal.
- Mild thrombocytopenia may be reported in 25% to 50% of patients.
- There is mild leucocytosis. In the first week, maybe leucopenia.
- Liver function tests are abnormal and return to normal in nearly 90 days. However, GGT may remain elevated for 3 to 12 months.
- LDH may also be raised.
- Molecular biology can detect EBV-DNA.
- The peripheral blood smear shows atypical lymphocytes.
- >50% are lymphocytes. This lymphocytosis is seen in 80% to 90% of the patients. Peak occurs during the second and third weeks and lasts 2 to 6 weeks.
- 5% to 30% are atypical lymphocytes.
- These atypical lymphocytes persist for 1 to 2 months,
- These atypical lymphocytes may last for 4 to 6 months in some cases.
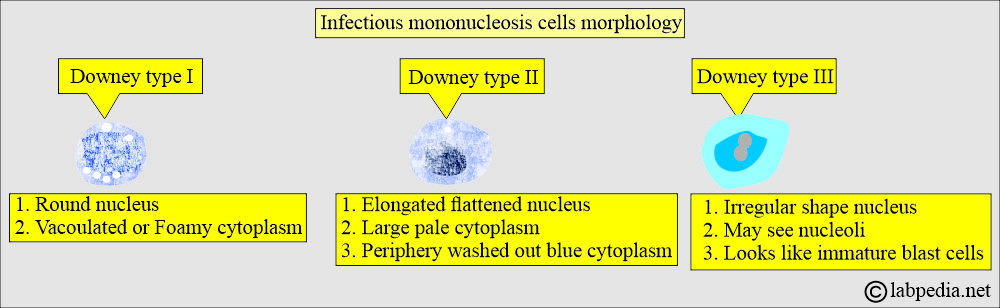
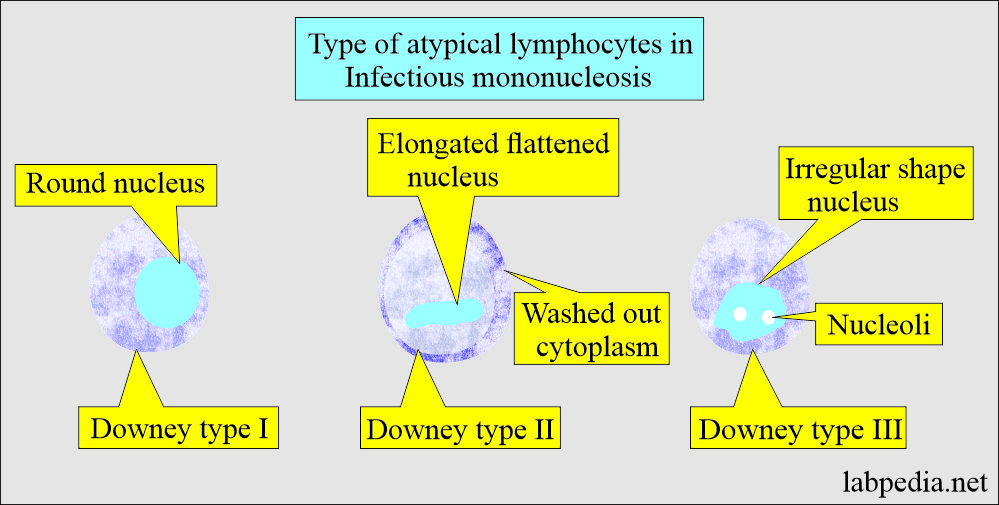
- Atypical lymphocytes are mainly Downey-type cells. These are divided into three main types.
- Downey type I has a round nucleus and vacuolated or foamy cytoplasm.
- Downey type II has an elongated, flattened nucleus and large, pale cytoplasm. At the periphery, there is washed-out blue cytoplasm.
- Downey III has an irregularly shaped nucleus. This may have nucleoli and suggest immature blast cells.
- All these atypical lymphocytes are larger than normal lymphocytes. The majority are activated CD8+ T lymphocytes (cytotoxic/suppressor).
- Few are activated B-lymphocytes, and these are Downey type III. These are EBV-transformed B-lymphocytes.
- These atypical lymphocytes are also seen in various diseases, such as CMV infection and acute viral hepatitis.
- These atypical lymphocytes may be confused with acute leukemia or lymphoma.
What are the serological markers for infectious mononucleosis?
There are following antibodies:
- Heterophil antibodies.
- Specific anti-EBV antibodies.
- Heterophil antibodies test:
- Monospot test (Heterophil antibody test):
- This test is done on the slide.
- Principle of heterophil antibodies:
- These heterophil antibodies against EBV react with and agglutinate sheep/horse RBCs.
- This test can be used as a screening test.
- The patient’s serum is added to slides and has horse or sheep RBCs.
- It is negative in 30% of patients with infectious mononucleosis.
- Monospot test (Heterophil antibody test):
- Paul-Bunnel screening test (Heterophil antibody test):
- This test is done in the tube, also called the tube method.
- The Paul-Bunnel antibody is an IgM antibody of unknown origin, as it is also found in other diseases.
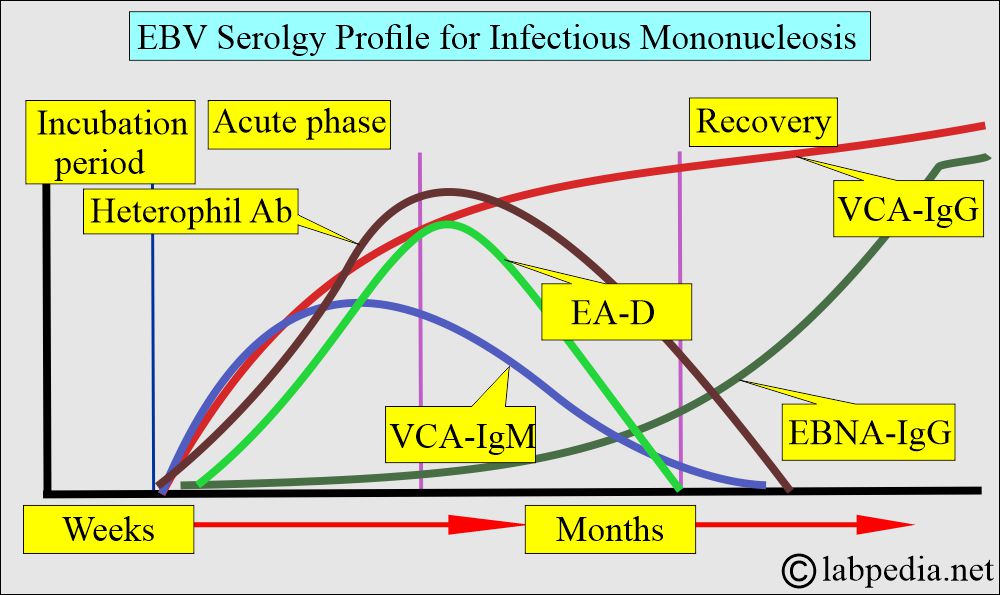
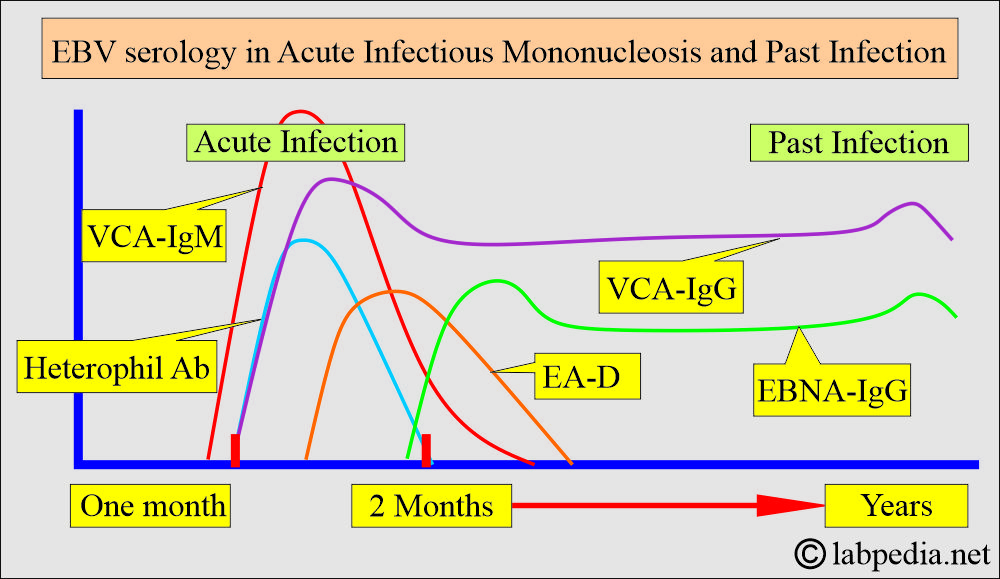
- Paul-Bunnel antibodies begin to appear in the first week of the Infectious Mononucleosis and peak in the second or third week. Then it starts declining in the fourth or fifth week. It may be undetectable by 8 to 12 weeks after the start of infectious mononucleosis.
- In a few cases, these antibodies may be seen for as long as 1 to 2 years after the infection.
- A Heterophil antibody test can not be used to monitor the disease.
- Davidsohn Differential test is based on the presence of heterophilic antibodies.
- This test is specific for the diagnosis of Infectious mononucleosis.
- Serologic tests are based on the following:
- These are the antibodies formed against the various antigens of the Epstein-Barr virus (EBV):
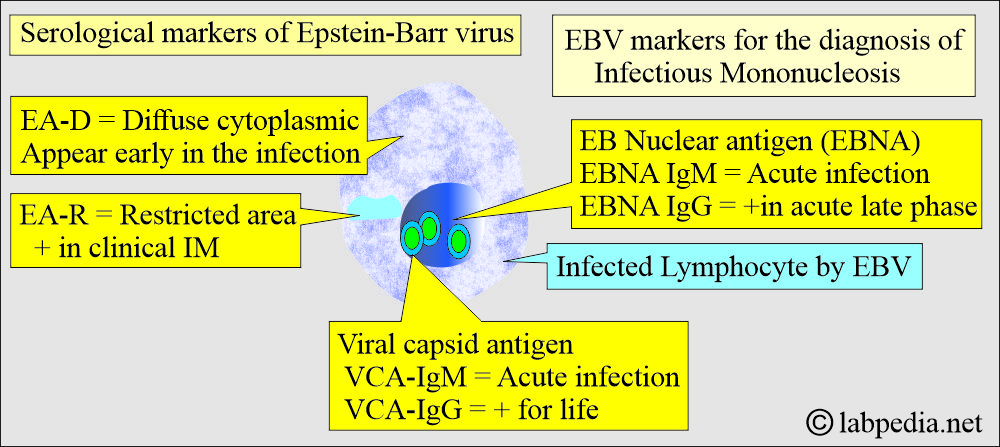
What are the EBV antigens?
- Viral capsid antigen = VCA
- Antibodies are VCA-IgM and VCA-IgG.
- This is detected in the early phase and disappears in 2 to 4 months.
- VCA-IgM presence suggests acute infection or convalescent stage.
- VCA-IgG is usually positive after the VCA-IgM. It remains elevated for life after an early peak.
- So, VCA-IgG presence indicates early acute, convalescent, or past infection.
- Early antigen = EBV early antigen EA.
- These are present in the cytoplasm of the infected lymphocytes.
- This is a complex of:
- EA-D.
- EA-R.
- EA-D: Early antigen-diffuse = EA-D.
- One antigen present throughout the cytoplasm is called a diffuse antigen.
- The antibody begins to rise in the first week of infection.
- There is an increase after the appearance of heterophil antibodies.
- After the peak, these antibodies disappear in the convalescent stage.
- Around 85% of patients produce the EA-D antibody.
- Its presence suggests an acute or convalescent stage of the disease.
- EA-D is found in EBV-associated nasopharyngeal carcinoma.
- An anti-EA-D IgG antibody is highly indicative of acute infection.
- It is absent in 10-20% of patients.
- It disappears in about 3 months.
- It is present in the nucleus and cytoplasm.
- EA-R: Early-antigen-restricted = EA-R.
- The second antigen is present in a restricted area of the cytoplasm and is called EA-R (early antigen-restricted).
- EA-R is found in about 5% to 15% of patients with infectious mononucleosis.
- It is more frequent, 10% to 20%, in children under 2 years.
- EA-R is also found elevated in EBV-Burkitt’s lymphoma.
- Usually not found in young patients.
- It appears transiently in the recovery stage.
- EBV can be confirmed in liver biopsy by in situ hybridization or PCR>
What are the serological markers for the diagnosis of Infectious Mononucleosis?
| Type of antibodies | When detected first | Peak level | When disappearing from the blood |
| EA-D | 5 days after S/S appear | 14 to 21 days after the S/S | 9 weeks after the appearance |
| VCA-IgM | At the start of S/S | During the first week of S/S | 2 to 3 months after S/S onset |
| VCA-IgG | 3 days after the onset of S/S | 2nd week after onset of S/S | Decline and then persists for life |
| EBNA-IgM | At the start of S/S | During the first week of S/S | 2 to 3 months after S/S onset |
| EBNA-IgG | 3rd week after onset of S/S | 8 months after the appearance | Persists lifelong |
| Heterophil Ab | 3 to 5 days after the onset of S/S | During the 2nd week of the onset of S/S | 2 to 3 months after the onset of S/S |
How will you summarize serological markers of Infectious Mononucleosis?
| Stage of the disease | Serological markers |
|
|
|
|
|
|
|
|
|
|
How will you treat Infectious Mononucleosis?
- This is mainly supportive.
- Corticosteroids may be helpful in some cases.
- Antiviral drugs are not recommended in most EBV cases.