Enteric Fever:- part 4 – Paratyphoid Fever, Diagnosis and Treatment
Salmonella paratyphi
What samples are taken from Salmonella paratyphi patients?
- Samples are taken like typhoid fever.
- Blood complete examination.
- Stool for culture.
- Blood for culture.
- Urine for culture.
- Roughly 105 to 109 organisms are required for the culture, but this count may be low in infants and older adults.
- This count may be low in patients taking antacids and H2 receptor blockers.
How will you define Salmonella paratyphi?
- Salmonellae are flagellate, gram-negative bacteria that cause a self-limited disease.
- It is food-borne and water-borne.
- Salmonella paratyphi causes a less severe disease than Salmonella typhi.
- While S. Typhi may lead to gastroenteritis or may cause life-threatening systemic disease.
How will you divide Salmonella infections?
- Typhoidal infection caused by S. typhi and S. paratyphi.
- Salmonella paratyphi is also a type of Enteric fever.
- Non-typhoidal infection, most common in the USA, is caused by:
- S. Typhimurium.
- S. enteritidis.
- 95% of cases are food-borne, and the rest are nosocomial infections.
- Salmonella is relatively uncommon in the USA; 70% are acquired abroad.
- Humans are the only source of this infection; it spreads from person to person or through contaminated food or water.
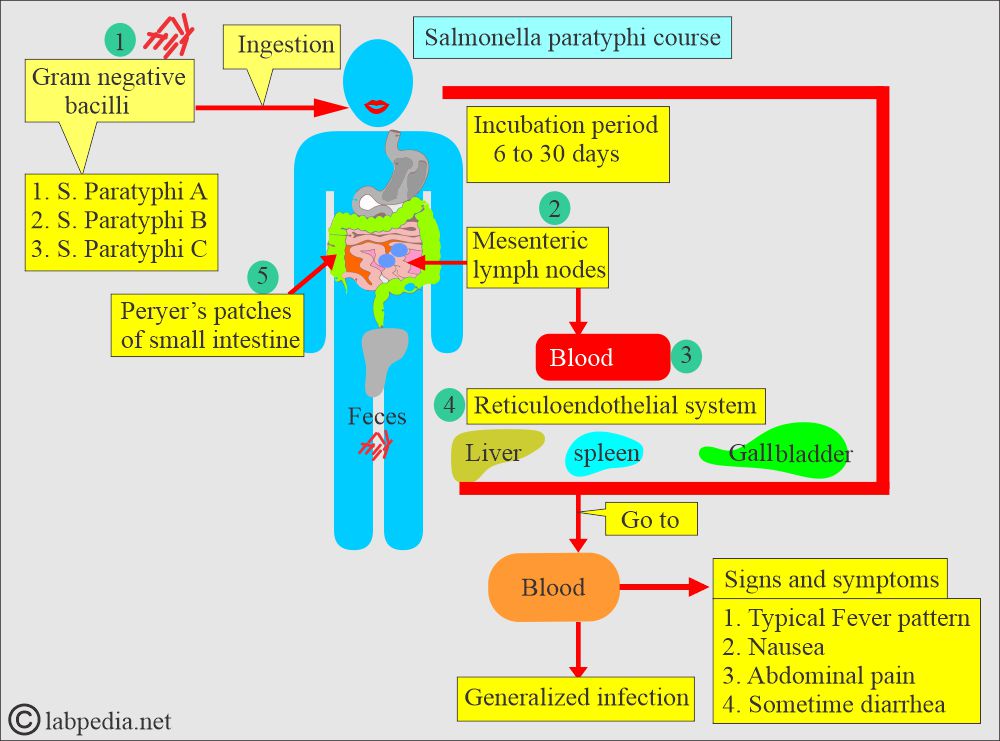
What are the types of S. Paratyphi?
- S. paratyphi A.
- S. paratyphi B.
- S. paratyphi C.
What is the incubation period of Salmonella paratyphi?
- It is 6 to 30 days.
- This is caused by Salmonella enterica, which has Paratyphi A, B, and C serotypes.
How will S. Paratyphi spread?
- It spreads through eating or drinking contaminated water or food contaminated with the patient’s feces or the carrier’s feces.
- Humans are the only species infected. There is no known reservoir in the animals and the atmosphere.
- Occasionally, this may spread sexually.
- Most cases are due to Paratyphi A compared to Paratyphi B and C.
How will you describe the Epidemiology of S. Paratyphi?
- Paratyphi A is confined to tropical countries.
- Paratyphi B is more common in Europe.
- This will have S/S like typhoid fever.
- Diagnosis is performed by isolating the bacteria or by detecting antibodies (anti-BH) in the Widal test.
- Paratyphi C is a rare infection mostly seen in the Far East.
- It presents as septicemia with the formation of an abscess.
- Culture usually makes the diagnosis.
- S. Paratyphi A and C are primarily seen in tropical countries.
What is the Microbiology of S. Paratyphi?
- It is a gram-negative, flagellated bacterium.
- Its growth is seen on special media:
| Type of media | Appearance in the media |
|
|
|
|
|
|
|
|
|
|
- Special test:
- S. Paratyphi does not produce gas during the fermentation of sugars.
- Serological identification was performed with Salmonella polyvalent O and H antisera.
- A bacteriophage study can differentiate S. Paratyphi B.
How will you explain the Pathogenesis of S. Paratyphi?
- These bacteria are internalized by intestinal epithelial cells lining Peyer’s patches and are abundant in the ileum.
- These are transported to the peyer patches; these bacteria enter the blood circulation.
- S. paratyphi often settles in the liver and biliary tree.
What are the Signs and symptoms of paratyphoid fever?
- These are like typhoid fever.
- Symptoms of paratyphi usually begin 6 to 30 days after the infection.
- S/S are milder than typhoid fever (Salmonella typhi).
- There are signs of weakness and a loss of appetite.
- A headache is quite common.
- Some patients may develop rose-colored skin rashes.
- Only 20% to 40% of patients develop abdominal pain.
- The duration is shorter.
- There may be transient diarrhea and symptomless infection.
- Without treatment, S/S may persist for weeks or months.
- The carrier state is less common.
How will you diagnose Salmonella paratyphi?
- The laboratory diagnosis of S. paratyphi is similar to that of typhoid fever.
Complete blood count (CBC):
- Low TLC, leucopenia.
- 4000 to 6000/cmm during the first 2 weeks, and 3000 to 5000/cmm during the next 2 weeks.
- Count >10,000/cmm indicates perforation or suppuration.
- Initially, there is normocytic anemia; in the presence of bleeding as a complication, the anemia becomes hypochromic and microcytic.
Blood culture:
- This is the gold standard for the diagnosis.
- Positive in the first week of infection in 80% of the cases. But blood cultures may reach 90% of cases, decreasing to 50% by the third week.
- Blood culture is considered 100% specific.
- Buffy coats may decrease the time for isolation.
- This is subcultured on the MacConkey media.
Bone marrow culture:
- If taken, it will be positive and may yield up to 90% sensitivity.
Stool culture:
- It will be a positive but not reliable test. This will be positive within the first 7 days of infection.
- This is negative in 60% to 70% of the cases during the first week if the patient is untreated, then positive in these patients in the third week (another reference says after the 10th day), with increasing frequency up to the 4th or 5th week in <50% of the cases.
- After 4 months, stool culture indicates a carrier state, which may be seen in ∼3% of cases.
- The chronic carrier may have a stool culture positive even up to one year.
- Feces cultures on solid selective media:
- Desoxycholate citrate agar, where there are non-lactose fermenting colonies.
- McConkey’s medium shows non-fermenting colonies.
- There is no gas and no fermentation of sugar.
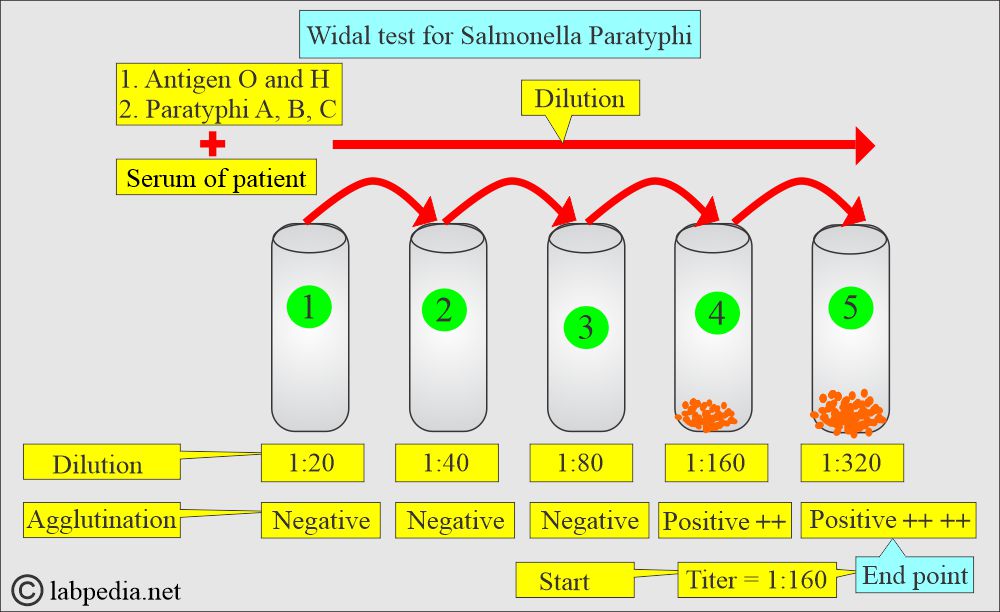
The widal test
- What is the Widal test principle?
- The widal test measures agglutinating antibody levels against O (somatic) and H (flagellar) antibodies.
- O-antibody (agglutinin) can usually be detected 6 to 8 days after the onset of fever.
- H- antibody (agglutinin) after 10 to 12 days.
- The classical Widal test is difficult to interpret when patients have already been vaccinated.
- An agglutination test is done for flagellar H and somatic O antigen with antisera (Salmonella paratyphi A and B).
What Salmonella paratyphi antigens are used in the widal test?
| Salmonella paratyphi type | Antigen suspension |
|
|
|
|
|
|
Why is the Widal test not used in routine practice?
- The widal test is positive in vaccinated cases.
- It is positive in the previous history of infection.
- Non-specific diseases may cause an increase in titer.
- Autoimmune disease may see false-positive results.
- Early treatment of typhoid fever may give negative or low widal titers.
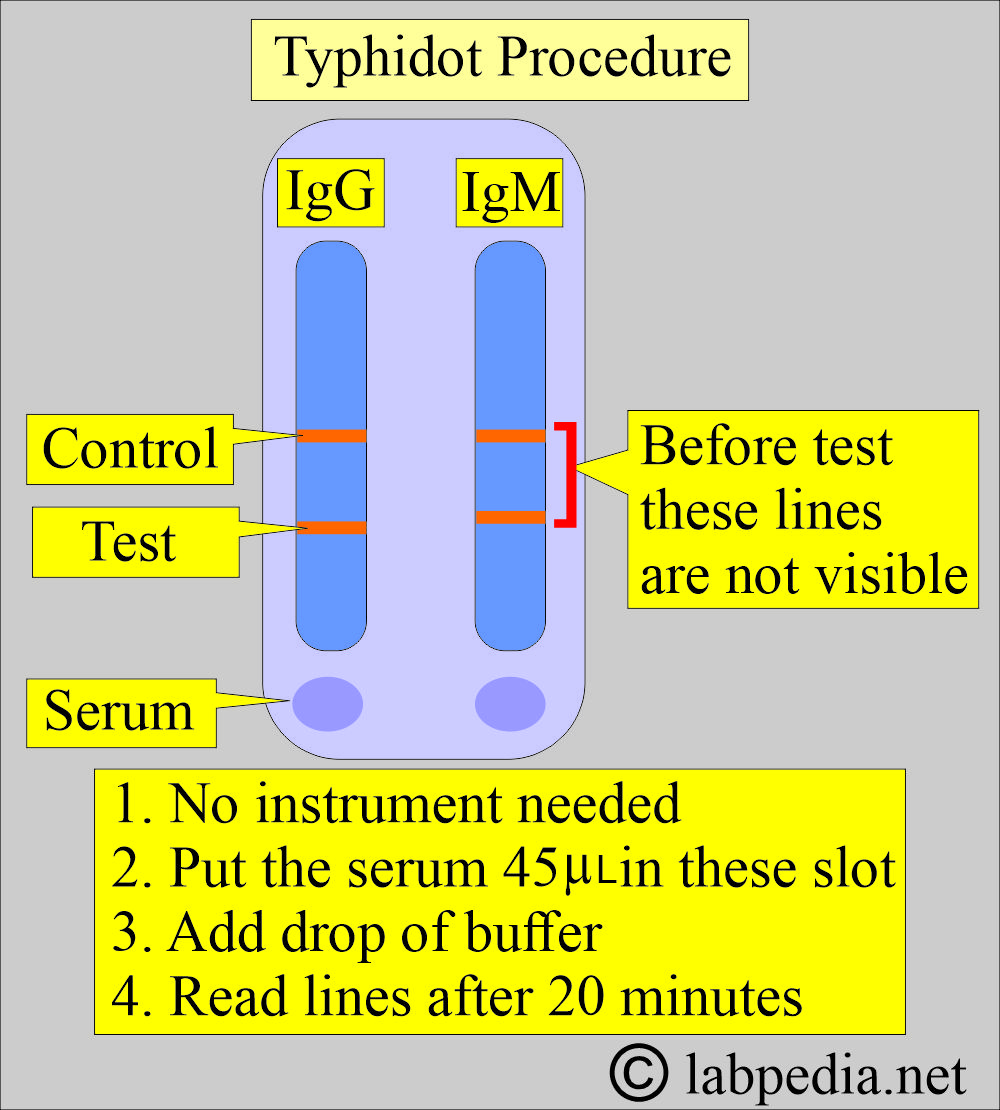
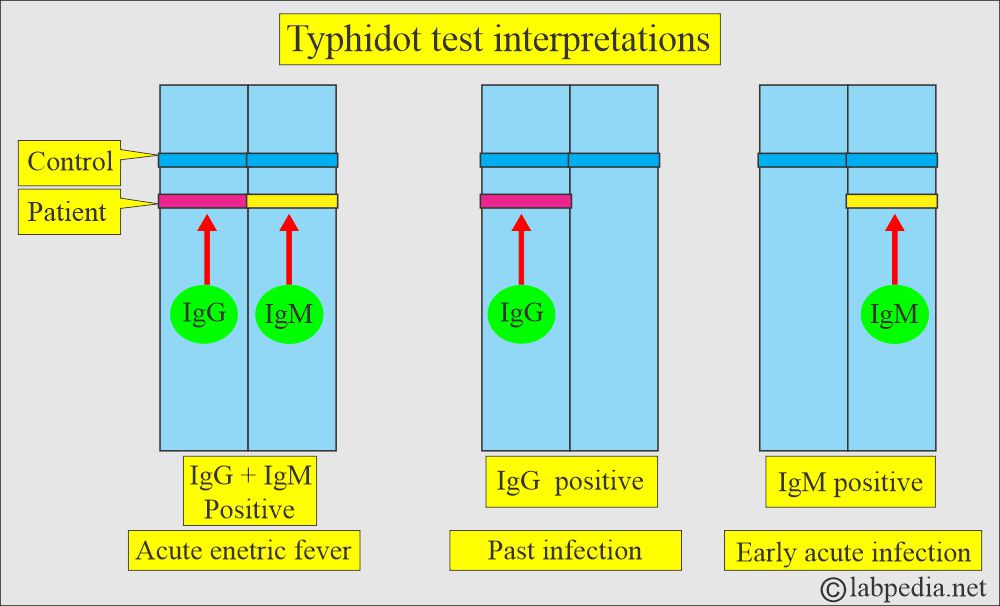
Typhidot test
- The manufacturing companies claim it will be positive after 2 to 3 days.
- This will detect IgM antibody, which is more sensitive and specific than the widal test.
- IgG antibodies can also be detected.
The urine culture:
- It may be done and is positive in the case of enteric fever, but it is less sensitive.
- This is done on the MacConkey media.
- Urine culture is positive during the 2nd to 3rd week in 25% of the patients, even if blood culture is negative.
Bacteriophage typing:
- It is done to identify the different strains of S. Typhi and Paratyphi.
- This is useful for epidemiological investigations into the outbreak’s source.
Identification of S. paratyphi:
- Biochemical tests indicate gas formation during sugar fermentation.
- Blood and urine cultures can also identify these organisms.
- Serology shows H and O antisera positive tests.
- Bacteriophage typing identifies the different types of Salmonella paratyphi.
| Type of Salmonella | Motility | Indol/Urease | Lysine decarboxylase | Gas production |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
How will you treat Salmonella paratyphi?
- Ciprofloxacin and Co-trimoxazole can be given.
- The drug of choice is chloramphenicol, but it is not used because of its complications.
- Treatment of carrier:
- The chronic carrier is less common but can be treated with ampicillin, chloramphenicol, and ciprofloxacin.
- Ultimately, advised cholecystectomy.
How will you control the spread of Salmonella paratyphi?
- Public health, including general hygiene, should be discussed with the public.
- The carrier should not be employed in the food industry. They should be taught public hygiene, such as washing hands and a clean water supply.
- Vaccination will also help to decrease the incidence of the disease.
Questions and answers:
Question 1: What is the difference between typhoid fever and Salmonella paratyphoid infection?
Question 2: What are the types of Salmonella paratyphi?