Chapter 8: Specific Immune cells, B and T Lymphocytes, NK cell, Null cell, APC
SPECIFIC (ACQUIRED) IMMUNE CELLS
There are two types of specific immune cells:
- B-lymphocytes
- T-lymphocytes
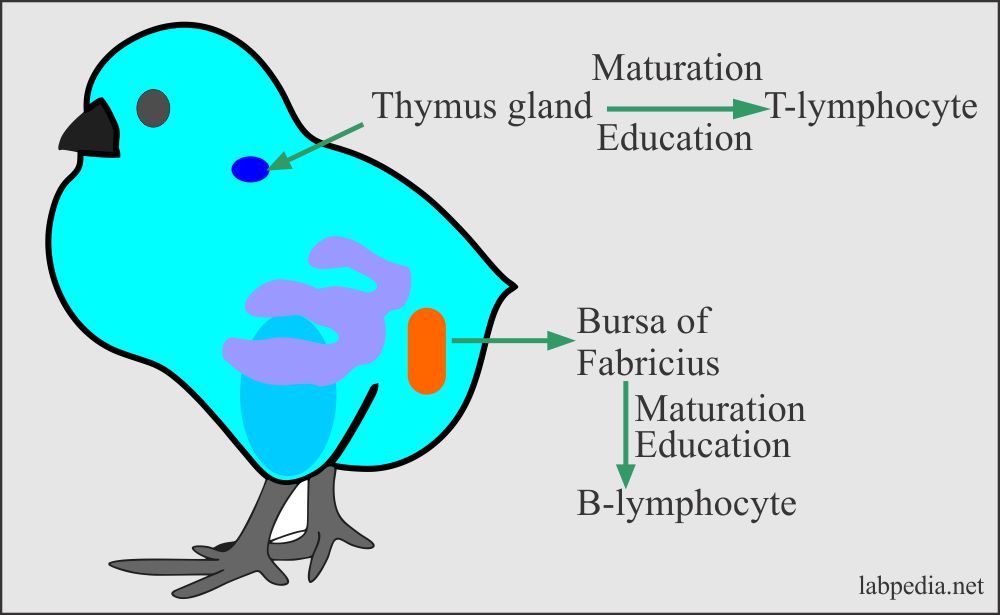
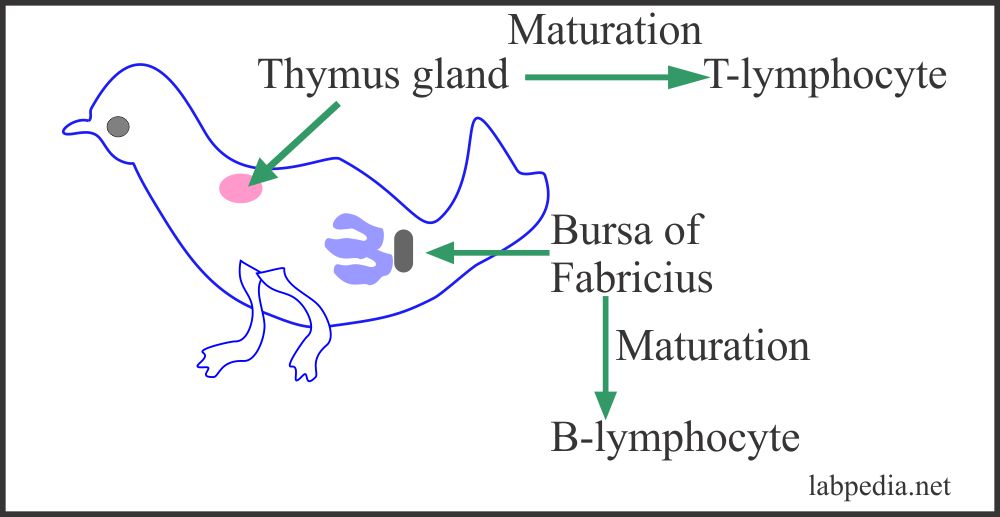
It is a famous experiment on the chicken where they took three groups of chicken:
- Normal group.
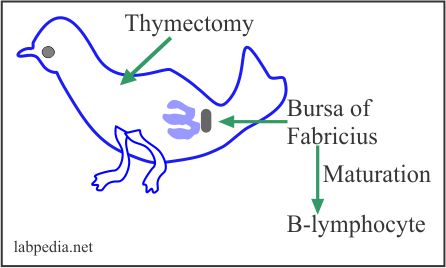
- Chicken with thymectomy.
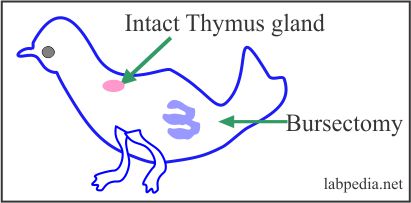
- Chicken with bursectomy.
The following experiment elaborates the origin of B and T lymphocytes:
| Group of Chicken | TLC | Ig Conc. | Ab Response | T.T | Graft Rejection |
|
1. Normal group |
1400 | ++ | ++ | ++ | ++ |
|
2. with Thymectomy |
9000 | ++ | + | – | – |
|
3. With Bursectomy |
13200 | – | – | + | + |
| Dependent on B-Lymphocytes | Dependent on T-Lymphocytes | ||||
Table VI – Maturation site of B and T cells elaborated from the above experiment
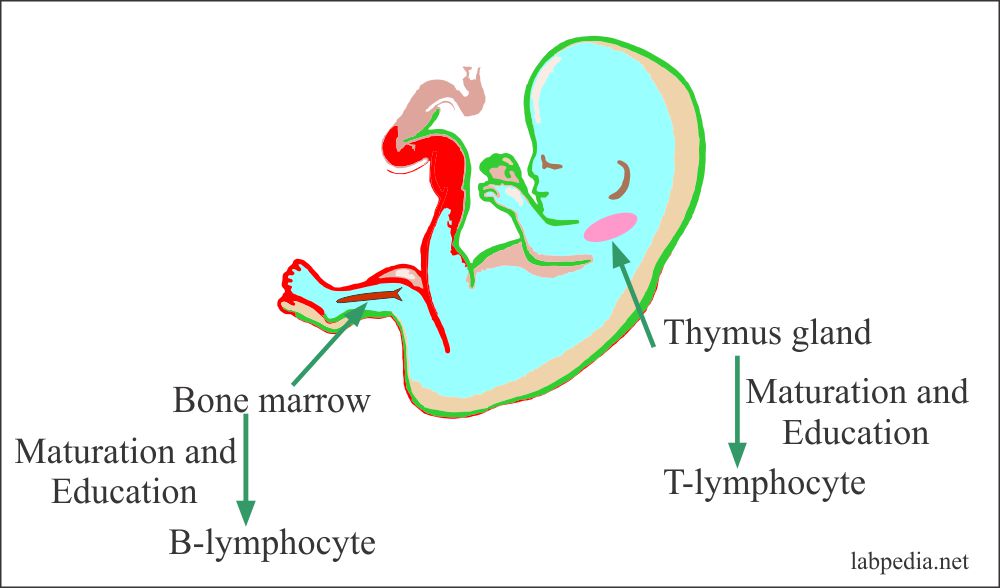
It shows that one set of lymphocytes for its maturation is dependant on an intact thymus gland called T-lymphocytes. In contrast, another set for its maturation is dependant on intact bursa in a bird called B-lymphocytes.
In thymus glands, T-lymphocytes get an education under the control of a humoral factor called thymosin. Many cells will die in the thymus glands, and these are the self-reacting lymphocytes that will react with the self-antigens
In humans, T-L is dependant on the intact thymus gland, while B-L is dependant on bone marrow and payer patches of gastrointestinal tracts.
Development of B-L and T-L:
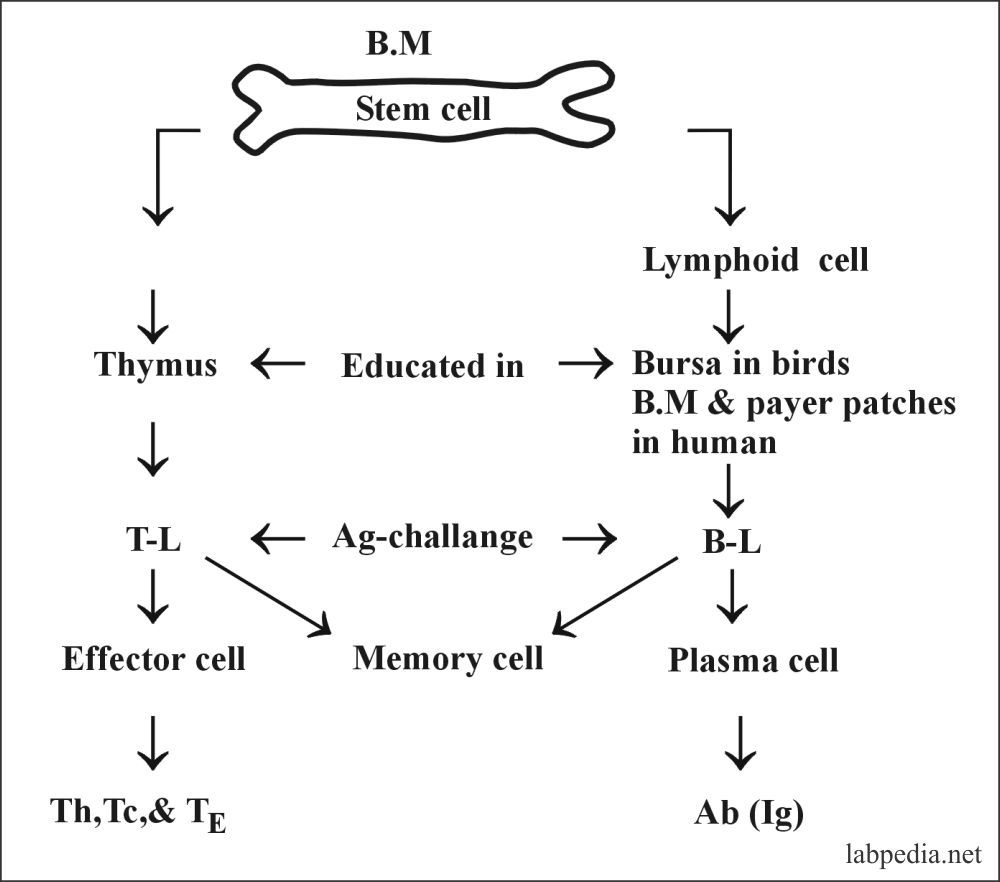
B-L and T-L develop from the stem cells in the bone marrow. These cells are matured in the thymus gland and the bone marrow. Now they will have different functions according to their site of maturation.
The stem cell is the mother cells for the formation of B-L and the T-L. Then these cells differentiate into different functional cells.
T- lymphocytes give cell-mediated immunity, and this will be effective against:
-
- viruses.
- Fungi.
- Rejection of the foreign tissue.
- Control the growth of the tumors.
B-lymphocytes are associated with humoral immunity and effective against:
- Viral infection.
- Bacterial infections
Distribution of the B and T lymphocytes in various organs:Lymphoid organ B-lymphocyte % T-lymphocyte % Bone marrow 90 10 Thymus 0 100 Blood 20 80 Spleen 55 45 Lymph nodes 40 60
B-LYMPHOCYTES
Definition of B-Lymphocytes:
Bone marrow-derived or called B-lymphocytes.
B-lymphocytes are the precursors of the immunoglobulin producing cells, Plasma cells, and are identified by immunoglobulin over their surface.
B- Lymphocyte s are 10-20% in the peripheral blood (another reference says 5 to 15 of the peripheral blood).
B-lymphocytes are also present in the bone marrow, peripheral lymphoid tissue, tonsils, lymph nodes, and spleen. Also present in the nonlymphoid tissue like gastrointestinal tract mucosa.
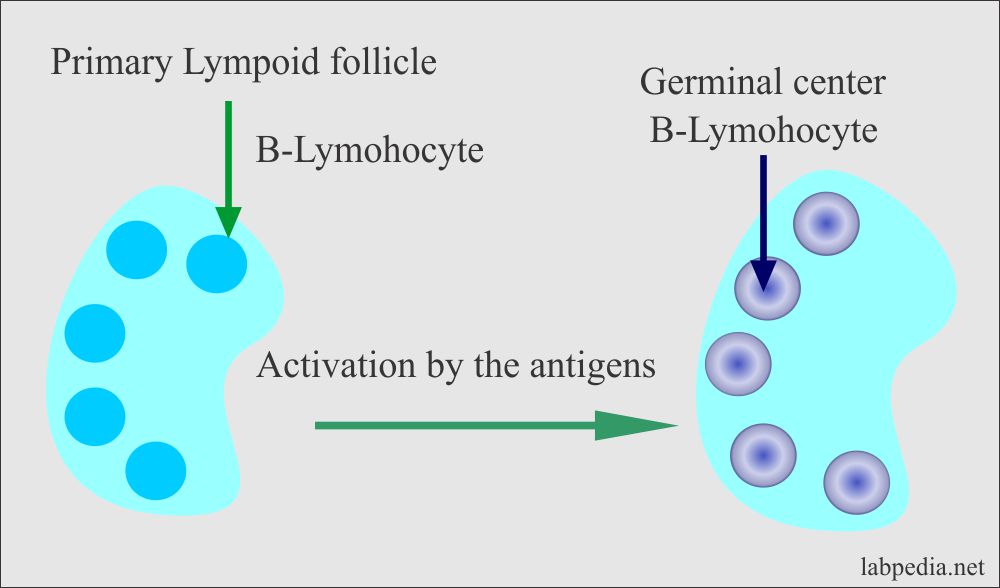
B-Lymphocytes development takes place in three phases:
- In the bone marrow from stem cells.
- From Bone marrow in the lymph node and spleen.
- In the lymph node in the germinal centers.
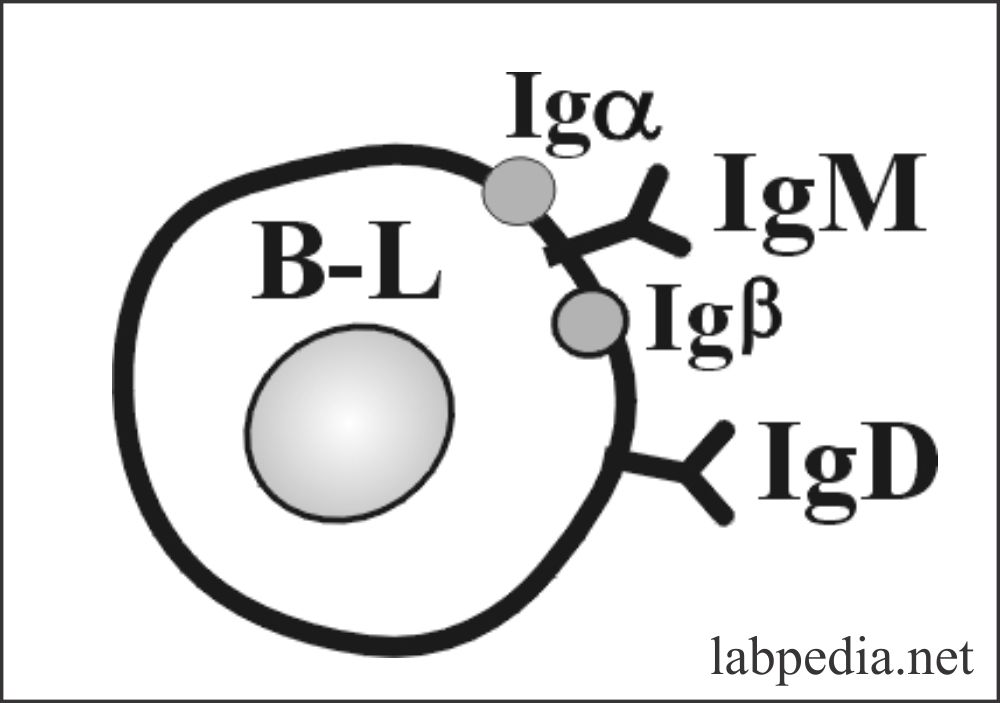
- The majority of the B-lymphocytes have both IgM and IgD on their surface.
- Roughly one fourth has one of the immunoglobulins, either IgM or IgD.
- 1% shows IgG or IgA.
Life Span
It is 5-7 days, and memory cells live for several years.
Site of Formation of the B-lymphocytes
- In the fetus, the site is the liver, yolk sac, and spleen. It starts at the 7-8th week of gestation. After 12-16 weeks in fetal life, Bone marrow takes over the function.
- These are present in the follicle of the cortex of the lymph nodes and the white pulp of the spleen.
- Follicular and medullary area germinal centers of the lymph nodes.
- The medullary cord of the lymph nodes.
- Primary follicle and the red pulp of the spleen.
- Follicular area of gut-associated lymphoid tissue (GALT).
- After stimulation by the antigen, the germinal center is formed in the follicles, which contains mainly B-lymphocytes.
Names at Various Stages of Development of B- Lymphocytes
- Pre B cell: It is present in BM and is immature cells.
- Immature B cell: still in BM & not ready to respond to antigen.
- Virgin B cell: present in lymph nodes and spleen with fully rearranged surface immunoglobulin but has not encountered the antigen.
- Mature B cell: present in lymph nodes and spleen, this possess antigen specificity.
- Memory B cell: This keeps the encounter antigen’s memory and is present in the lymph node.
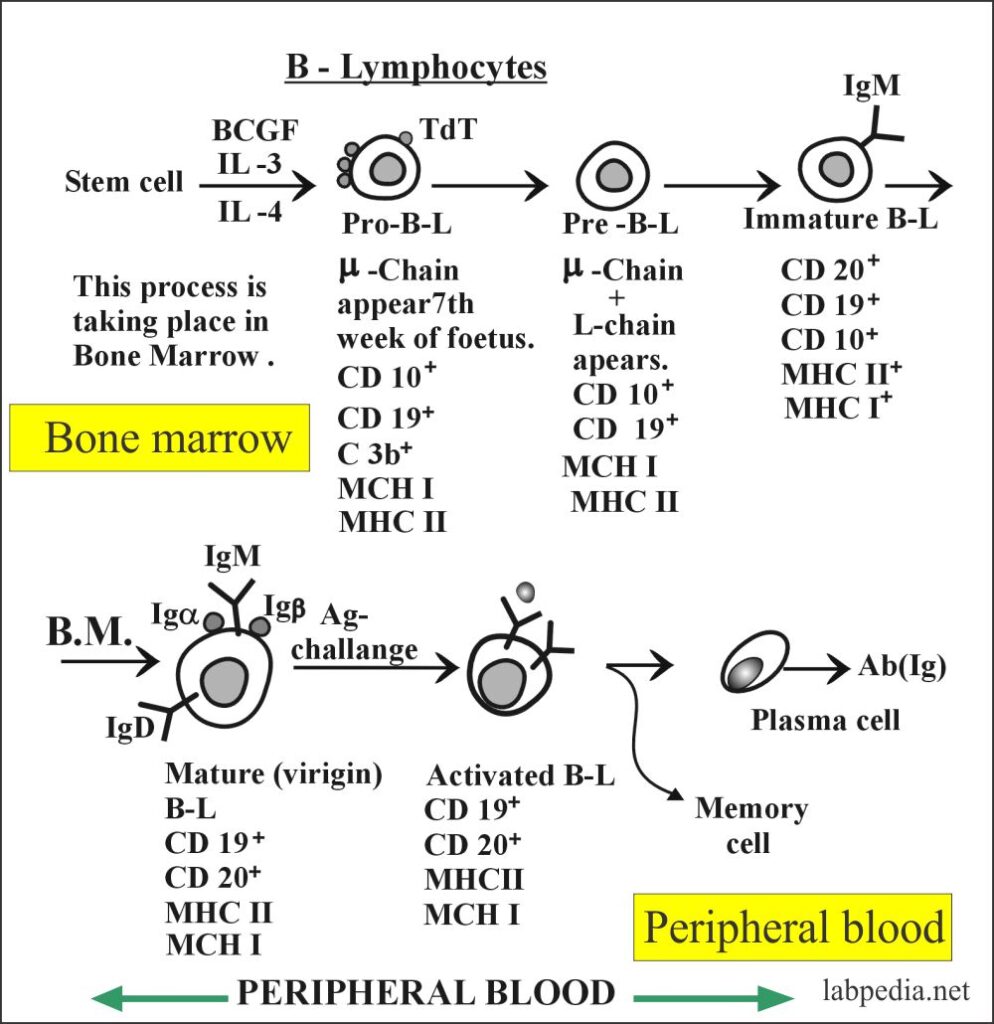
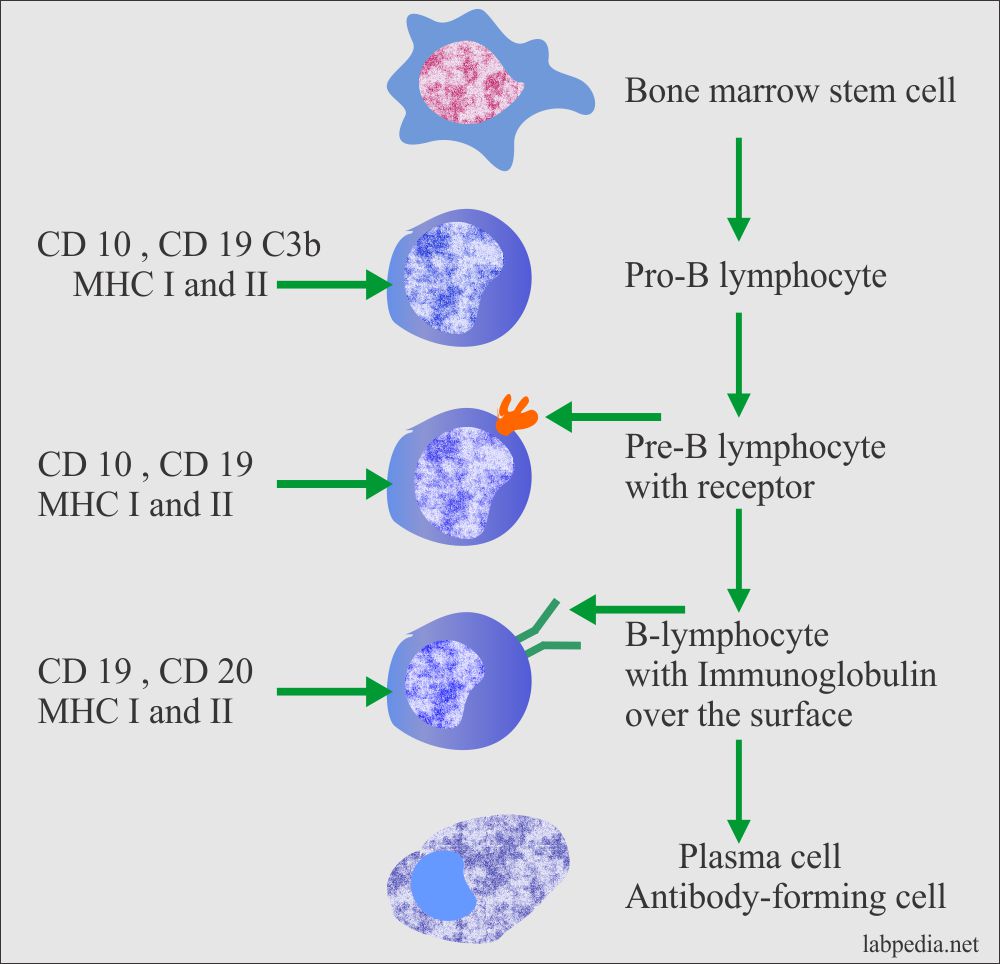
- Summary of B-L maturation:
- Bone marrow stem cell
- Pro-B-L
- Pre-B-L with the receptor on the surface.
- B-L with the antibody on the surface.
- B-L develops into plasma cells.
Surface Markers of Mature B-Lymphocytes
- In human, there are four types of cell surface markers:
- Immunoglobulin (Ig) receptor. The monoclonal antibodies detect these.
- An Fc receptor. It binds the Fc portion of the IgG antibody.
- B- cell surface antigen coded by MHC class II molecule.
- Receptor for the cleaved complement C3. This is seen in roughly 75% of the cells. It binds C3b and iC3b and C3d.
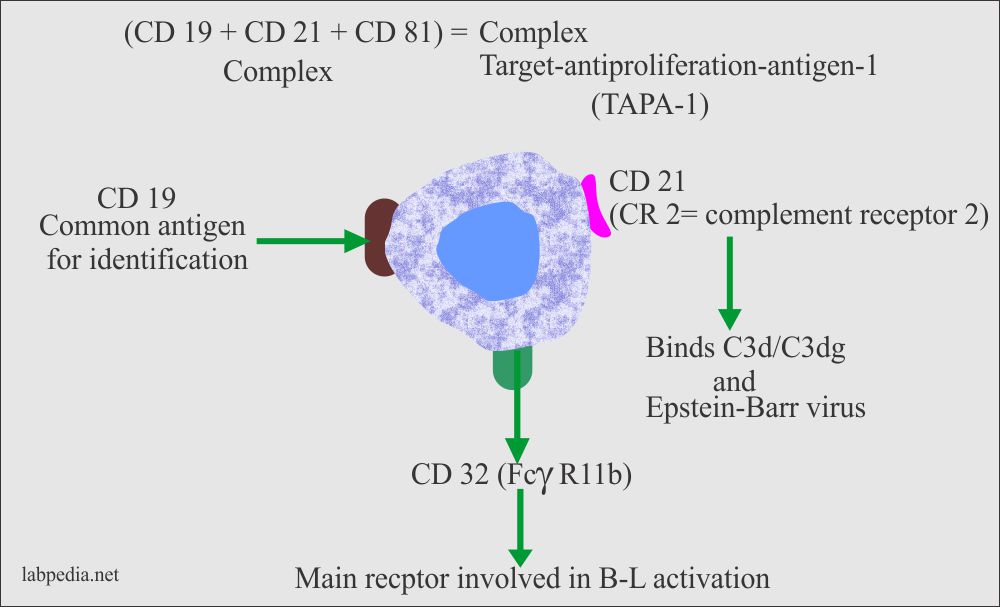
- Pan B-antigens is CD19 and CD20. CD19 is called a common marker.
- TdT is a terminal deoxynucleotidyl-transferase enzyme present only on immature cells and 2% positivity while absent on mature B cells. Immature T-L shows 90% positivity.
- CD10 is also called CALA Ag (common acute lymphocytic leukemia antigen).
- Other CD molecules are CD22, CD40, and CD45.
- Surface receptors for Fcγ R, C3b, EBV, and transferrin are present.
- The antigen receptor is called BCR (B-Cell receptor for an antigen), which consists of:
- IgM and IgD as an antigen receptor.
- A signal transduction complex comprising of Igα/Igβ is present near the IgM molecule.
- B7 (CD80 & CD86): This is co-stimulatory molecule. It interacts with CD28 and (CTLA-4) on T-L.
- CD40: It is important for the development of BCR.
- FcγR II (CD32): This helps in the antibody feedback mechanism. This is involved in the activation of the B-lymphocytes.
- MHC molecules: Both MHC, I & II molecules are expressed over the surface.
Formation of Immunogloubolins by B-Lymphocytes
- IgM synthesized in fetal life by the 10th week of gestation.
- IgM appears after 5 -10 days of antigen exposure, and then IgG appears after another 2-3 days.
- IgA appears by the 30th week of fetal life.
- IgG, IgM, and IgA are 95% and relatively small contributions from the IgD and IgE.
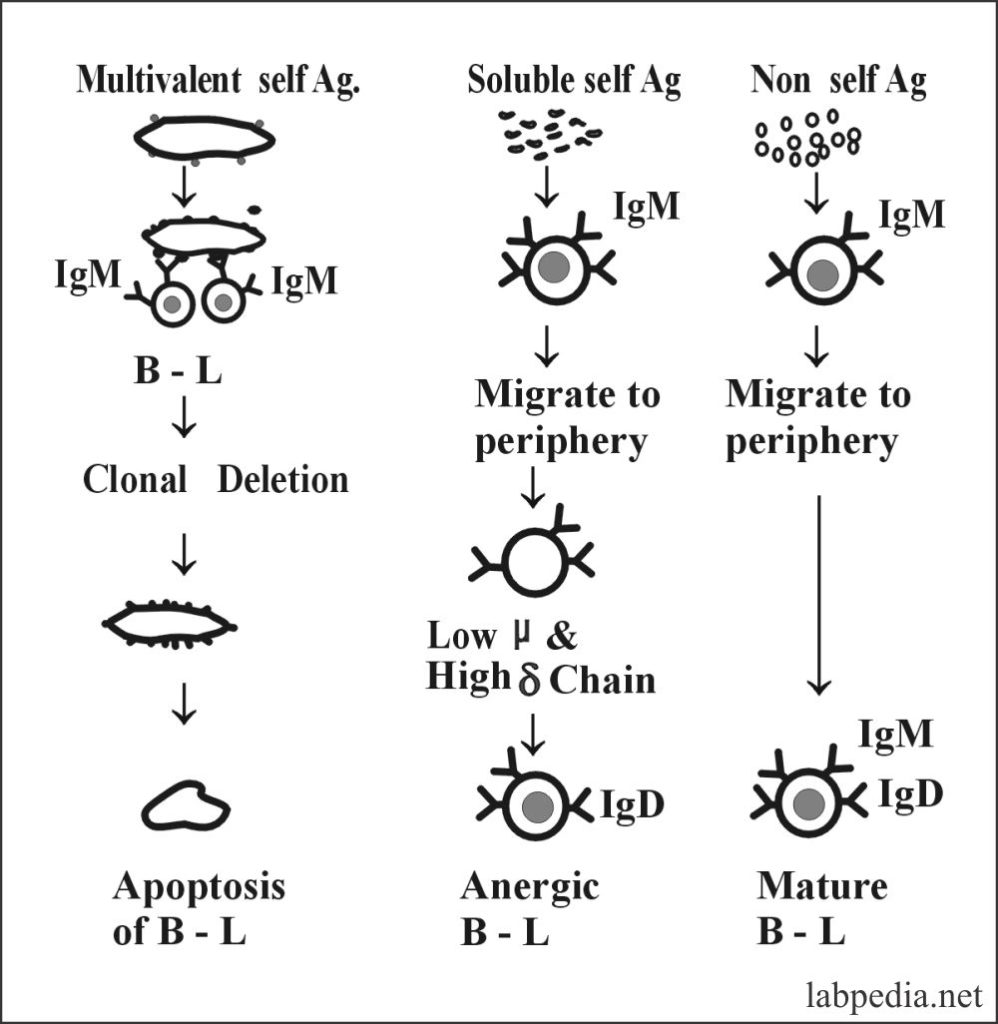
Self-Reacting B-Lymphocytes
Self-Reacting B-Lymphocytes are eliminated or inactivated by contact with self-antigen during the developmental stages of maturation; this process occurs in the bone marrow by immature B-L elaborated in the diagram below where self reacting antigens are either deleted or made anergic.
B1 – lymphocyte:
- These are the subset of the B-lymphocytes and have a very long life.
- B1-L are found in the fetal liver and embryonic omentum and not in the bone marrow.
- B1-L are of two types:
- B1-CD5 positive are labeled as B1a.
- B1-CD5 negative are labeled as B1b.
- This B1-L is frequently associated with autoantibody production.
- This B1-L also produce IL-10.
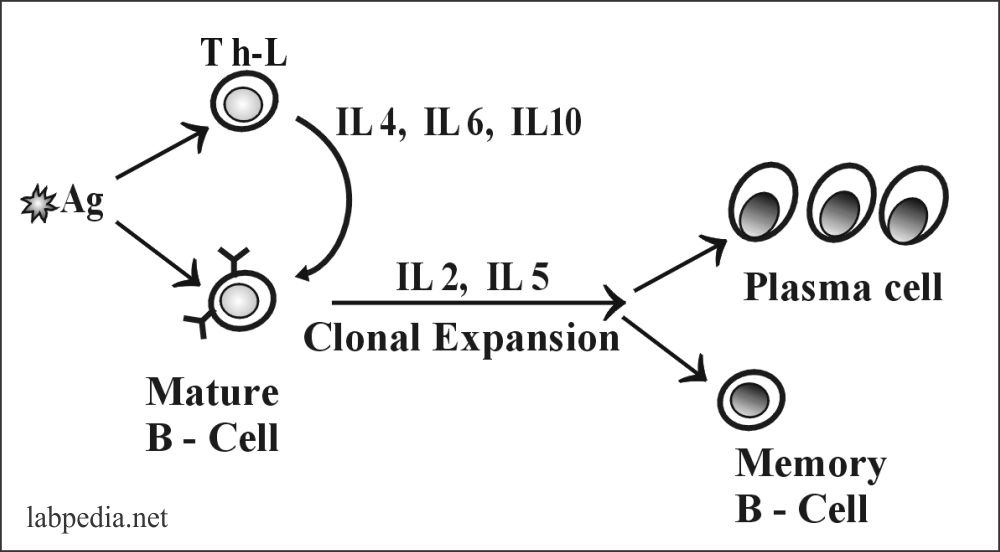
Activation of B-Lymphocytes
This may be:
- Single signal T-L independent stimulation.
- Two signal T-L dependent stimulation.
- Cytokines of B-L activation.
A. Single signal T-L independent stimulation
Where the antigen directly stimulates B-lymphocytes, one can say that these antigens are T-L cell Independent. Mostly the antigens are lipopolysaccharides or antigens with multiple antigenic sites that cross-link the surface immunoglobulin.
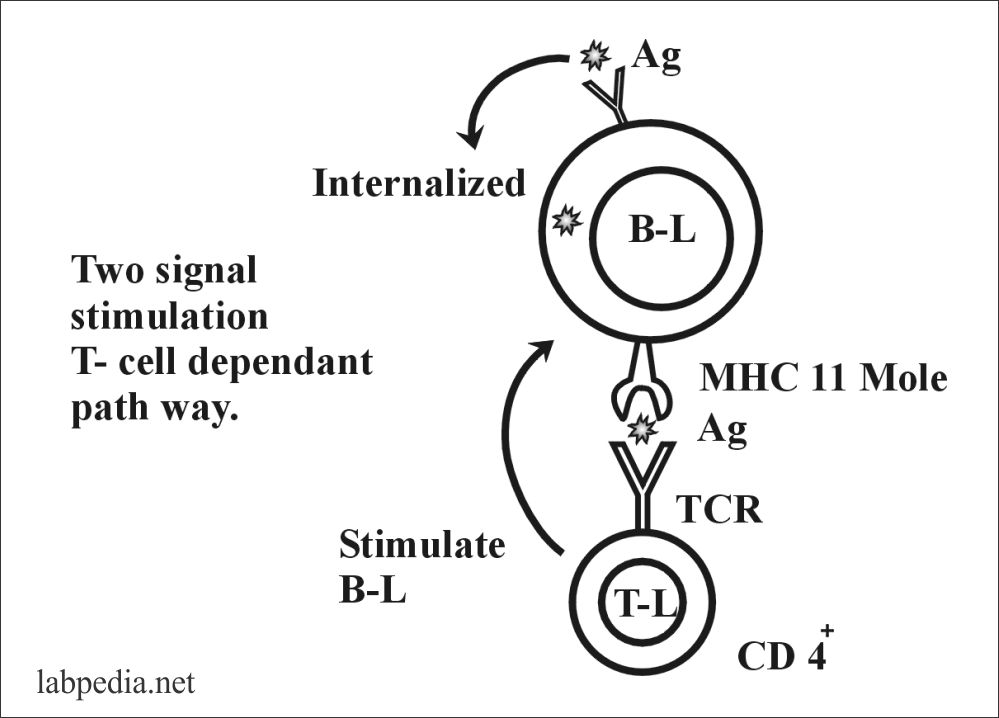
B. Two signal T-L dependent stimulation
In this case, B-Lymphocytes need help from the T-L cell, so one can say that there are antigens, T-cell dependants.
First, antigens are processed by APC (or B-L, which acts as APC), then presented to T-L (CD 4+), where TCR recognizes antigen along with MHC II molecule and which will send signals to B-L, this will be activated and transform into plasma cells and memory cells.
C. Cytokines for B-L Activation
IL-4 is the main B-L activator, and also it stimulates B-L growth, and IL-5 is to some degree. IL 2 promotes clonal expansion. IL-6 is a B-L growth factor that also enhances the switching of IgG production.
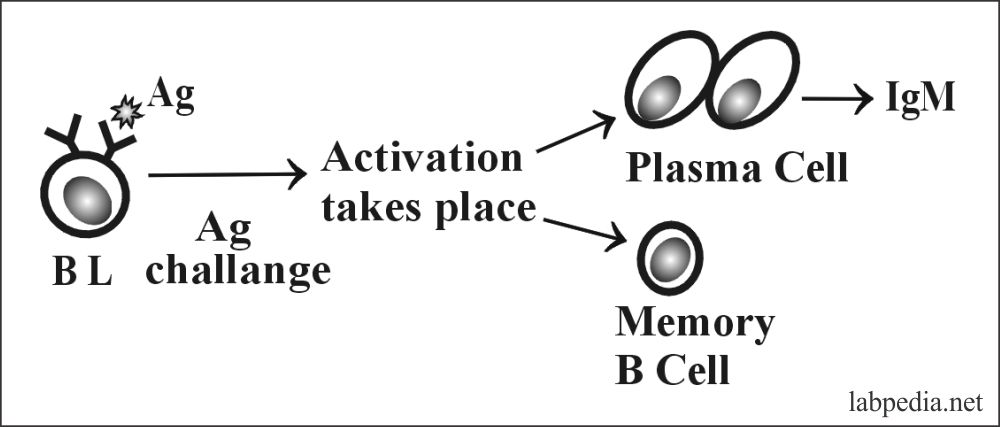
Consequences of B-L Activation
When an antigen activates B-L, the first primary immune response is IgM formation after a lag period of 5-10 days.
Primary Immune Response: The IgM-Ab formation is followed after 2-3 days by IgG formation
Secondary Immune Response: When the same antigen rechallenges B-lymphocyte, then primed memory cells are activated, and there is a quicker process (3-5 days) that produce IgG in much greater quantities.
Functions of B-Lymphocytes
It has two major roles.
- To ensure antibody production against the specific antigen.
- Ag-presenting function (APC), where it will process the antigen and present it to T-L.
- IgA is important for mucosal immunity.
- IgE has an important role in parasitic infestation and the allergic reaction.
Clinical Importance
B-L deficiency leads to various immunological diseases like:
- Bruton’s Syndrome.
- Selective IgA deficiency.
- Infections by H. Influenzae, Streptococcus Pneumoniae, Steph. Aureus, Echoviruses, and Giardia Lamblia are common.
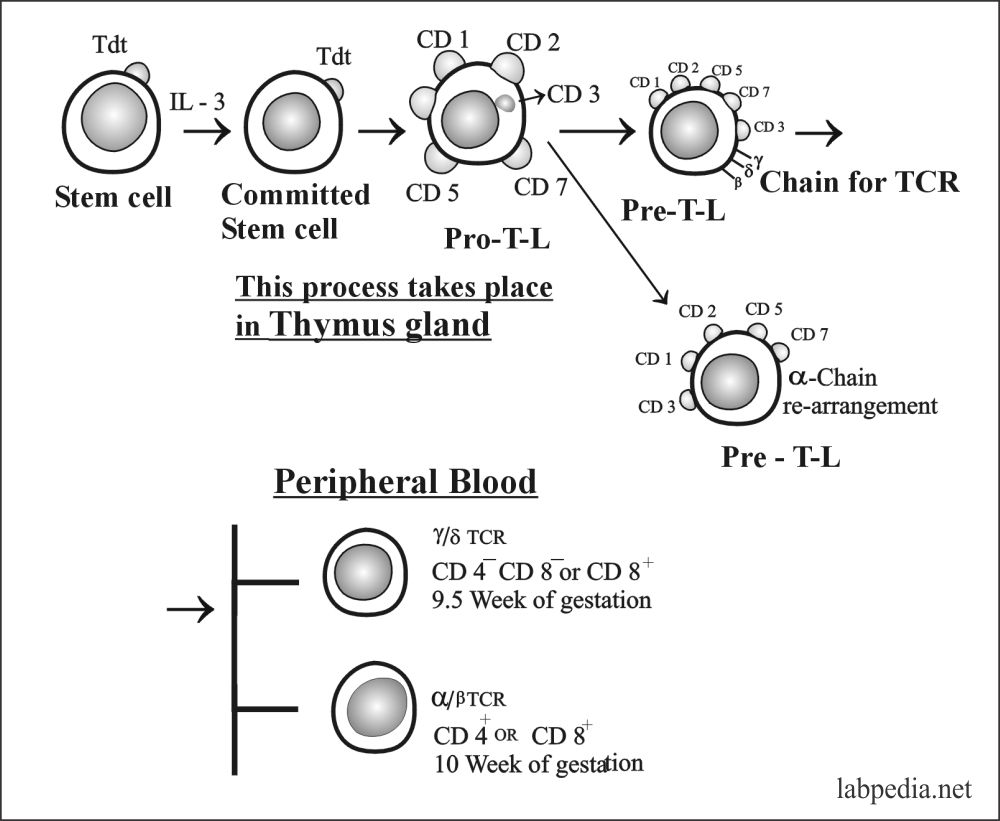
T-LYMPHOCYTES
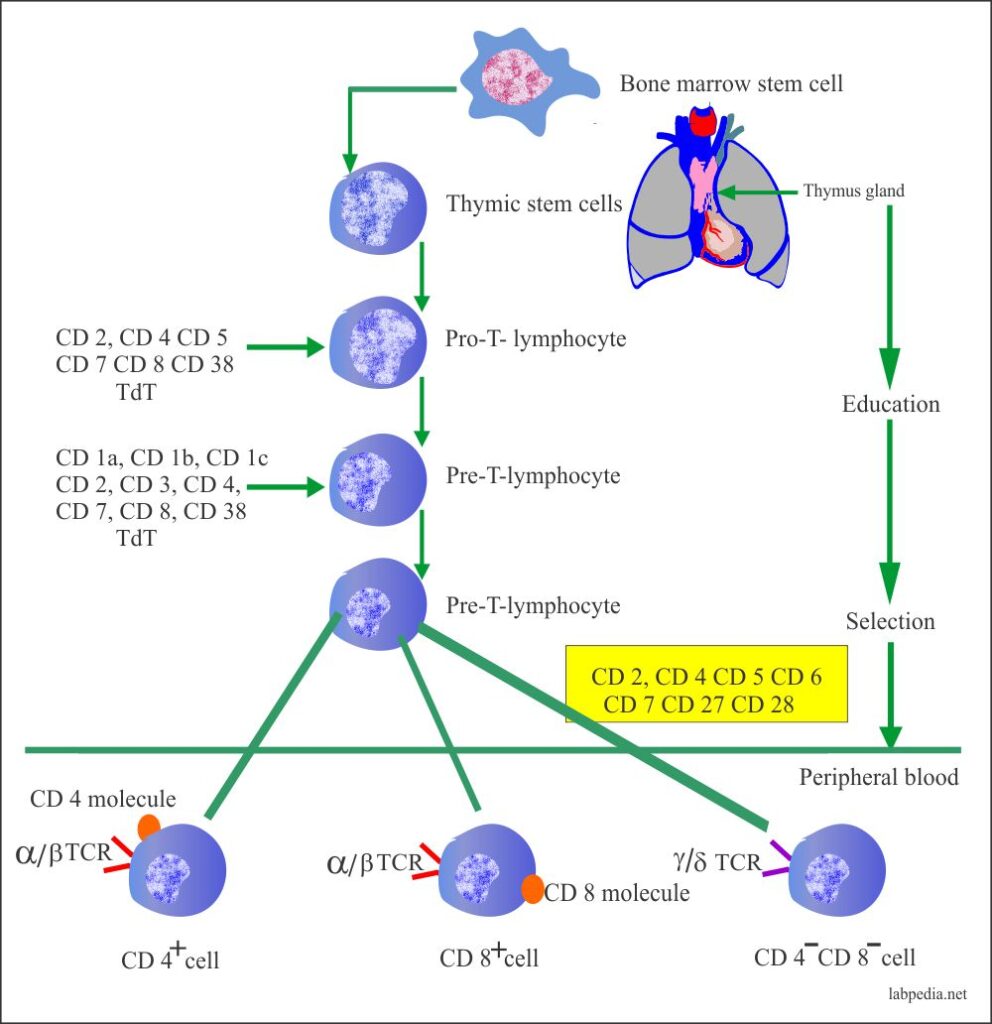
60 to 80% of the circulating lymphocytes are T-lymphocytes derived from the thymocytes that mature in the thymus glands under the influence of thymic hormones. These cells are responsible for the cellular immune response and regulation of the antibody reaction by activating or suppressing B-lymphocytes’ activation.
These T-lymphocytes play an important role in:
- Cellular immune response.
- Regulation of the antibody reaction either by helping or suppressing the activation of the B-lymphocytes.
- T-lymphocytes differentiation begins in the fetus and neonatal life when the lymphocytes precursors migrate to the thymus glands.
- In the thymus gland, T-L develops specific surface antigens and becomes functionally competent cells.
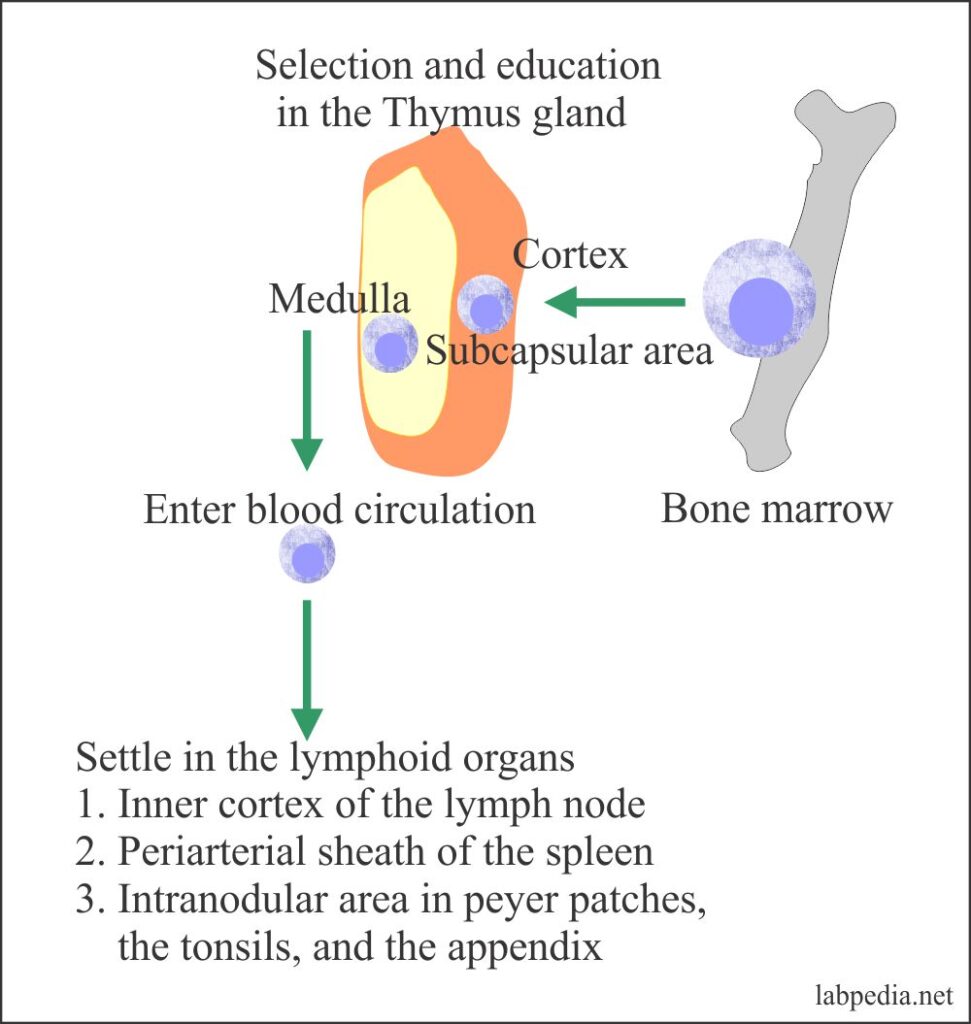
The T-lymphocytes develop from the bone marrow stem cell, then these are selected and educated in the thymus gland, from there they enter peripheral blood with specific functions.
T-lymphocytes are seen in the following area:
- Perifollicular and paracortical areas of the lymph nodes.
- Medullary cords of the lymph nodes.
- Periarterial region of the spleen as in sheath form.
- The thoracic duct of the lymphatic system.
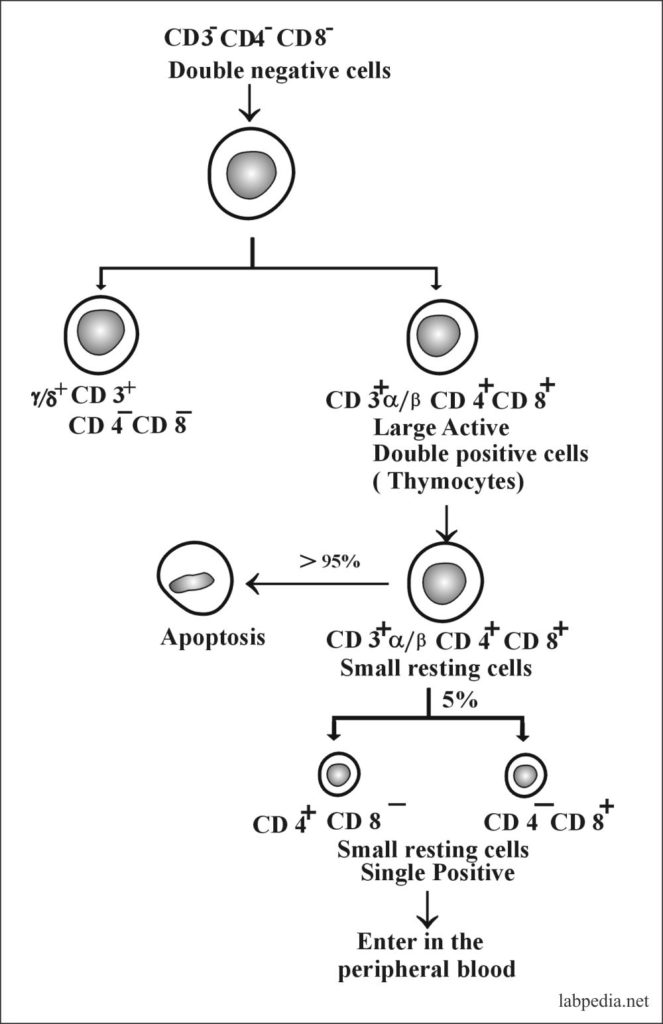
In the early development of the thymus gland, some of the antigens appear and then disappear, and ultimately when the lymphocytes leave the thymus gland, they are either CD4+ or CD8+ cells.
Role of Thymus Gland in Selection & Education of T-Lymphocyte
The Thymus Gland is the site for selecting and educating the T-lymphocytes (CD4+ and CD8+ cells). It performs the following selection:
A. Positive selection – Recognition of self-MHC.
- MHC recognition leads to cells’ death by Apoptosis, and MHC recognition also leads to Positive selection.
B. Negative selection – There is the clonal deletion of all self-reactive T-L.
Most T-L development takes place in the cortex. Only single positive thymocytes are seen in the medulla. Lymphocytes enter thymus glands as double negative cells. Then in the thymus glands as thymocytes, differentiate into double-positive cells with a low level of TCR. Then (CD4+ CD8+) cells enter the thymus cortex and undergo a positive selection for self-MHC restriction and start to lose one of the two co-receptor molecules.
When lymphocytes leave the thymus glands are either CD4+ or CD8+ cells.
The self reacting lymphocytes are generally deleted during the maturation process.
Later on, there is an involution of the thymus glands, and 95% of the gland mass is lost during the first 50 years of age.
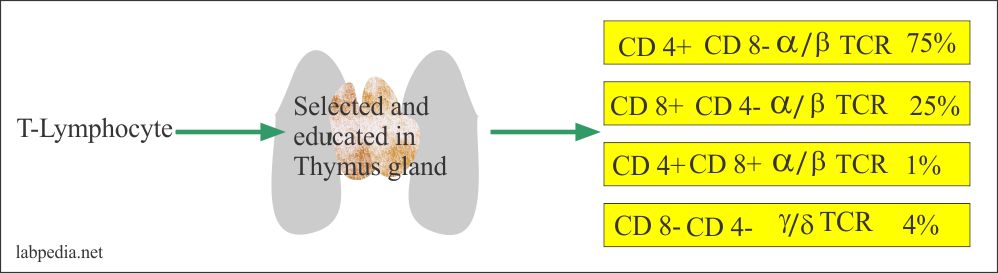
Types of T-Lymphocytes
- T-helpers cell CD4+ α/β TCR (Th).
- T-suppress or cytotoxic cell = CD8+ α/β TCR (Ts/Tc).
- CD4+ CD8+ α/β TCR.
- CD4– CD8– γ/δ TCR.
- The normal ratio of helper cells and suppressor cells (Th/Ts) ratio is roughly 2:1, which may reverse in certain conditions.
The following table shows the various T-Lymphocytes and their characteristics.
| CD8+ | CD4+ | CD4–8– | CD4+8+ | |
| MHC I Restriction | Class I Molecule | Class II Molecule | ? | ? |
| Functions | Cytotoxic | Helper | Cytotoxic | ? |
| Frequency | > 25% | > 75% | > 4% | > 1% |
| Antigen Receptor | α/β TCR | α/β TCR | γ/δ TCR | α/β TCR |
Table VII- Types and Characteristics of T-Lymphocytes
| The cluster of differentiation CD molecule as an antigen | The old nomenclature | Distribution in the lymphocytes |
| CD1a | Leu-6 | <1% T-lymphocytes |
| CD2 | Leu-5b, T-11 | 78 to 88% of T lymphocytes and NK cells |
| CD3 | Leu-4, T3 | 68 to 82% Mature T lymphocytes (TCR complex) |
| CD3+CD2 | Leu-4+5b | 83±5% NK cells and T lymphocytes |
| CD4 | Leu3a, T4 | 35 to 55% of mature T lymphocytes and monocytes |
| CD5 | Leu-1 | 65 to 79% T lymphocytes, B cell subset |
| CD7 | Leu-9 | 75% T lymphocyte and NK cells |
| CD8 |
Leu-2a, T8, Leu-2b |
20 to 36% mature T lymphocytes 19 to 37% mature T lymphocytes |
| CD10 | CALLA | >90% of ALL, acute lymphoblastic leukemia, immature B lymphocytes, and granulocytes |
| CD16 | Leu-11a, Leu-11b, Leu-11c | 8 to 22% NK cells, neutrophils |
| CD19 | Leu-12 | 5 to 15% of B lymphocytes |
| CD20 | Leu-16, B4, B1 | 5 to 15% of B lymphocytes |
| CD21 | B2 | 5 to 15% mature B lymphocytes, dendritic cells |
| CD23 | Leu-20 | <10% of B lymphocytes, Activated B lymphocytes |
| CD 38 | Leu-17 | 24 to 44% T lymphocytes, NK cells, Activated T lymphocytes, B lymphocytes subset |
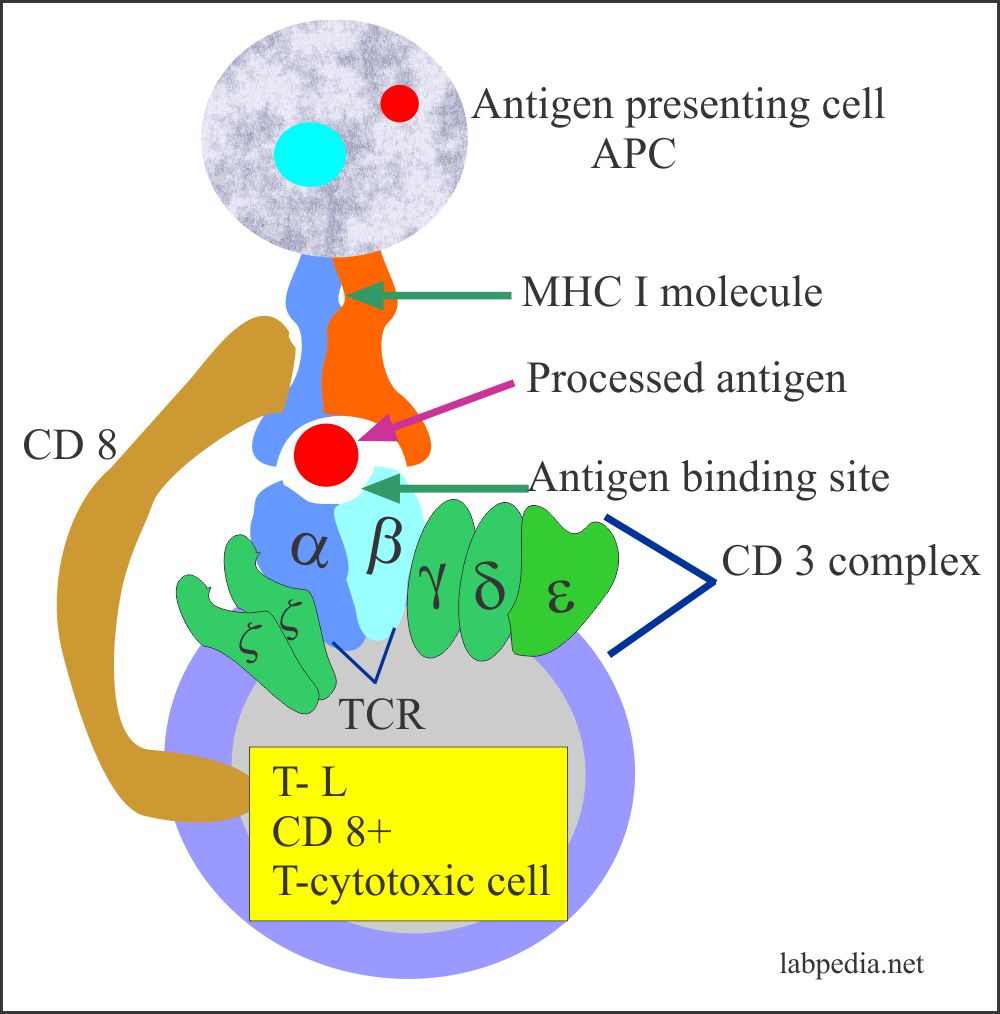
A. CD8+Tc
- CD8+ Tcytoroxic cells have the capacity to kill the other cells.
- CD8+ cells representing suppressor/cytotoxic cells and accounts for 25 to 40% of the peripheral T lymphocytes.
- These are T-cytotoxic cells.
- The Ts/Tc control and inhibit antibody production either by suppressing CD4+ helper cells or turning off the B lymphocyte activation.
- There are two subsets of CD8+ cells:
- Leu 9.3+ exerts cytotoxicity.
- Leu 9.3 – exerts suppression.
- α/β TCR and CD 8 molecules are identified on their surface.
- Tc-cytotoxicity takes place with the help of:
- MHC- class I molecule.
- The activated cell produces IL-2 & γ-interferon.
- CD 8+ cells recognizes MHC 1 (HLA-A, B ,C) of the target cells.
B. CD8+Ts
- T-suppressor cell suppresses the immune system by:-
- Release of soluble suppressor factor (TGF-b).
- Suppress T-h cells.
- Inhibit differentiation of B-L.
- It suppresses the antibody formation by the plasma cells.
- It suppresses the contact sensitivity.
- It suppresses the T-cytotoxic (Tc) cells.
- Idiotype anti-idiotype network.
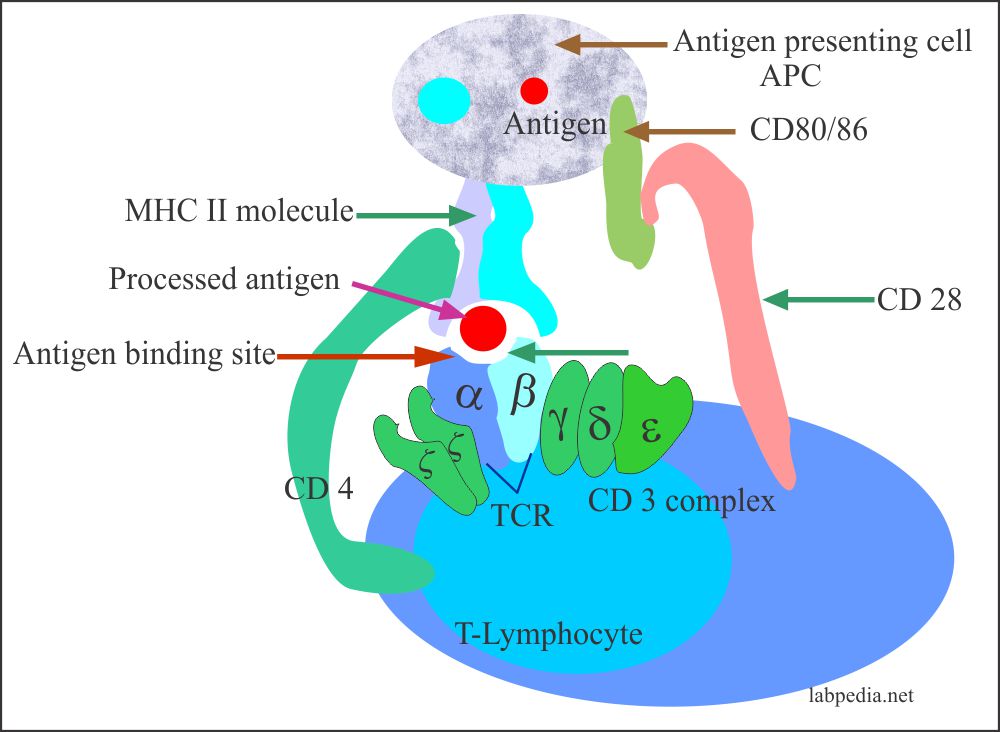
C. CD4+ Th
- CD4+ cells were called helper/inducer T lymphocytes and are 55 to 70% of the peripheral T-lymphocytes.
- α/β TCR and CD4 molecules are identified on their surface.
- CD4+ cells recognize MHC II molecules of the target cells.
- Functions:
- Increase B-L activity and generate antibodies.
- CD4+ cells recognize foreign antigens or markers on the infected cells and help activate the B lymphocytes.
- Recognize antigen with MHC-II molecule.
- The activated cell produces IL 2, which serves as a growth factor and increases Tc and NK activity.
- Control the production and switching of types of antibodies formed.
- Activates CD8+ Ts cell and cytotoxic cells and the natural killer cells (NK).
- Influence the Tc and NK cells to kill the infected cells.
- They influence the activity of monocytic-macrophagic cells.
- IL-4 increases B-L and T-L growth.
- These cells have a severe impact on the defense against viruses, fungi, parasites, and few bacteria, including mycobacteria.
- Some anti-T cell antibodies are present in patients with Juvenile rheumatoid arthritis (JRA). Based on these antibodies, these cells are divided into:
- CD4+ + helper/inducer (CD4+JRA-).
- CD4+ inducer/supressor (CD4+JRA+).
The subpopulation of Th-Cell (CD4+)
Th0—Produces mixed cytokines: γ-interferon, IL2, IL4, IL5, IL6, and IL10.
Th0 differentiate into:
A. Th1: Th1 cells are called inflammatory cells that synthesize and secrete IL-2 and g-interferon. Their main role is in Cell-Mediated Immunity (CMI). It activates macrophagic and Tc cells.
B.Th2: Th2 cells are called T-helper cells. It produces IL4, IL5, IL2, IL6, and IL10. It also activates B-L and antagonizes Th1.
Markers of T-Lymphocytes
- Terminal deoxynucleotidyl-Transferase or TdT enzyme is present on 90% of the immature T-Lymphocytes.
- Common T-L Antigens are CD3 (& CD2) present on all peripheral T-L.
- They have CD 4 or CD 8 molecules.
Functions of T-Lymphocytes
- T-helper cells activate B-L and lead their proliferation and inducing them to produce antibodies by transforming them into plasma cells and memory cells.
- Recruitment and activation of specialized cytotoxic cells (CD8+).
- Recruitment and activation of mononuclear phagocytic cells in Cell-mediated Immunity.
- Secretion of cytokines responsible for growth and differentiation of a range of cell types, including T-L, B-L macrophagic cells, and eosinophils, e.g., Interleukine and g-interferon.
- Regulate immune response.
- CD2/E is a receptor that binds sheep RBC and gives rosette-formation.
- It does not recognize intact antigens unless processed by APC and presented along with MHC I or MHC II molecules.
- T-lymphocytes protect the human against:
- Intracellular pathogens.
- Viral infection.
- Fungal infection.
- Protozoan.
- Chronic rejection in organ transplantation.
T-CELL RECEPTOR FOR ANTIGEN(TCR)
TCR was identified in the mid-1980s. The genomic organization of TCR is just like immunoglobulin family genes.
Types of TCR
- α/β TCR: It is present in 95% of the T-L.
- γ/δ TCR: It is rare (1-10%) on T-L. It is also present in epidermal cells and intestinal epithelial cells.
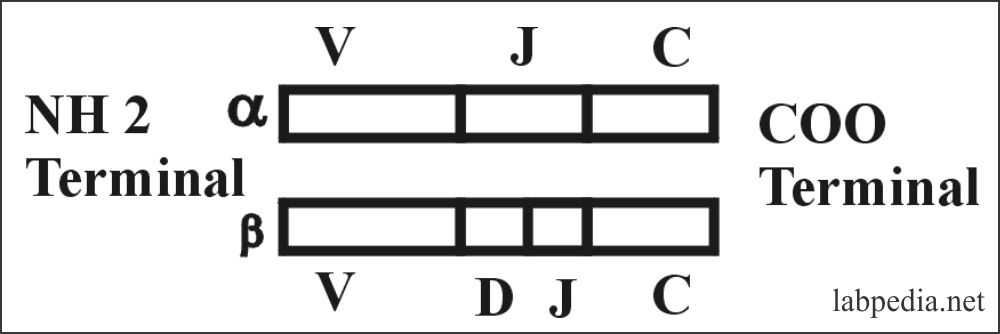
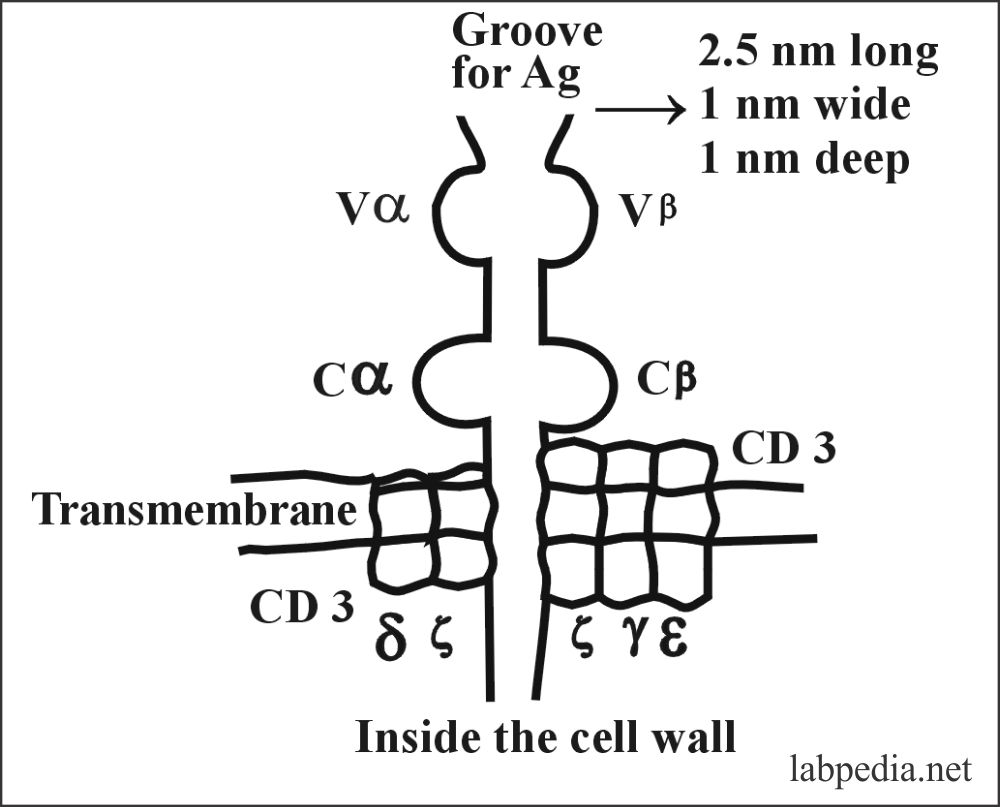
Structure of α/β TCR
TCR consists of α- chain with a 50,000, and β-chain with a molecular weight of 40,000 with variable portion and constant portion, these are linked by disulfide bonds.
V: Variable C: Constant J: Joining change D: Diversity
- The variable portion of α & β chains of TCR is similar to the variable portion of an immunoglobulin.
- TCR also shows idiotypic determinants similar to immunoglobulin.
- TCR has hypervariable areas (CDR or Hot spot) like immunoglobulin.
Functions of TCR
- The function of TCR is to recognize the Antigen complex with the self-MHC molecule, which is formed when the antigenic peptide becomes embedded within the MHC groove.
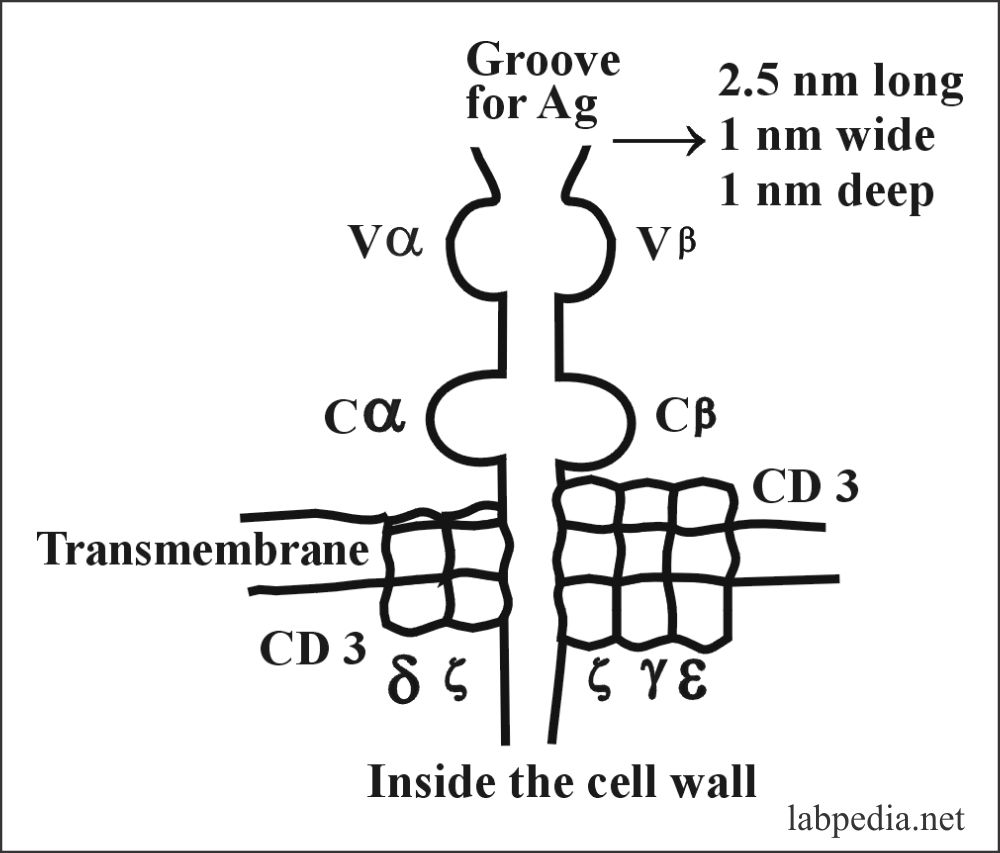
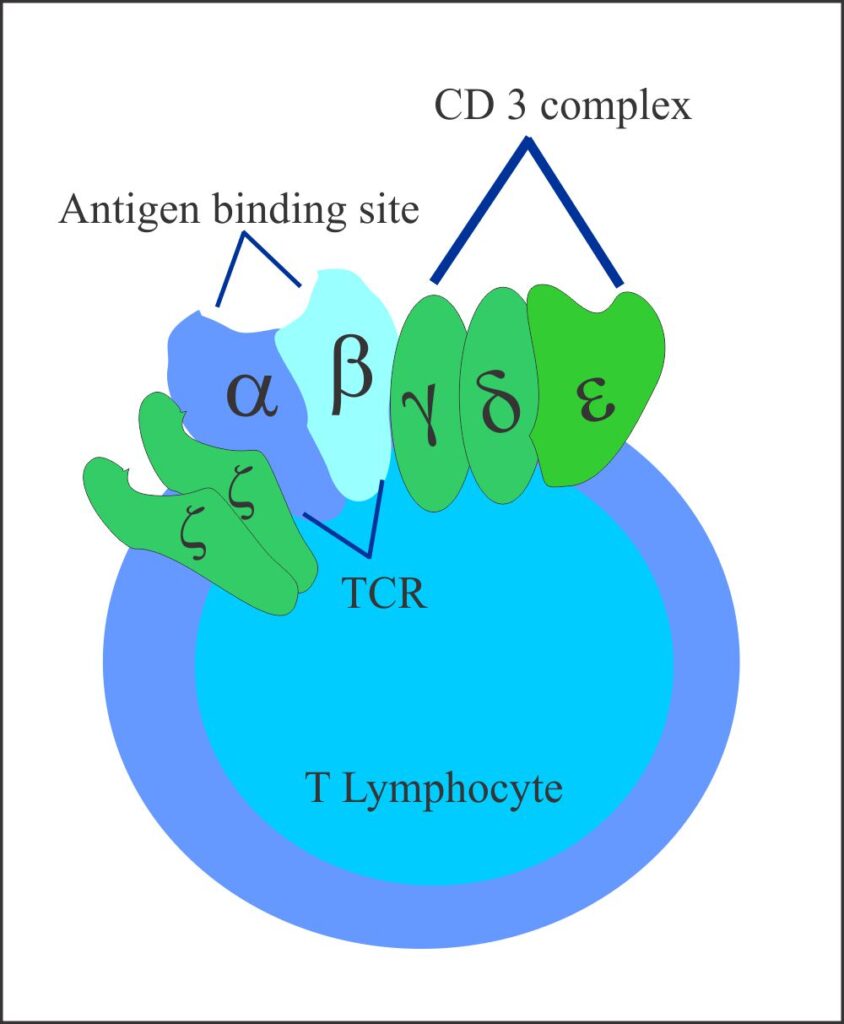
- TCR recognizes antigen along with MHC molecules. CD3 molecule activates T-Lymphocyte by sending signals to the interior of the cells.
Role of B7 Family of Co-Stimulatory Molecules
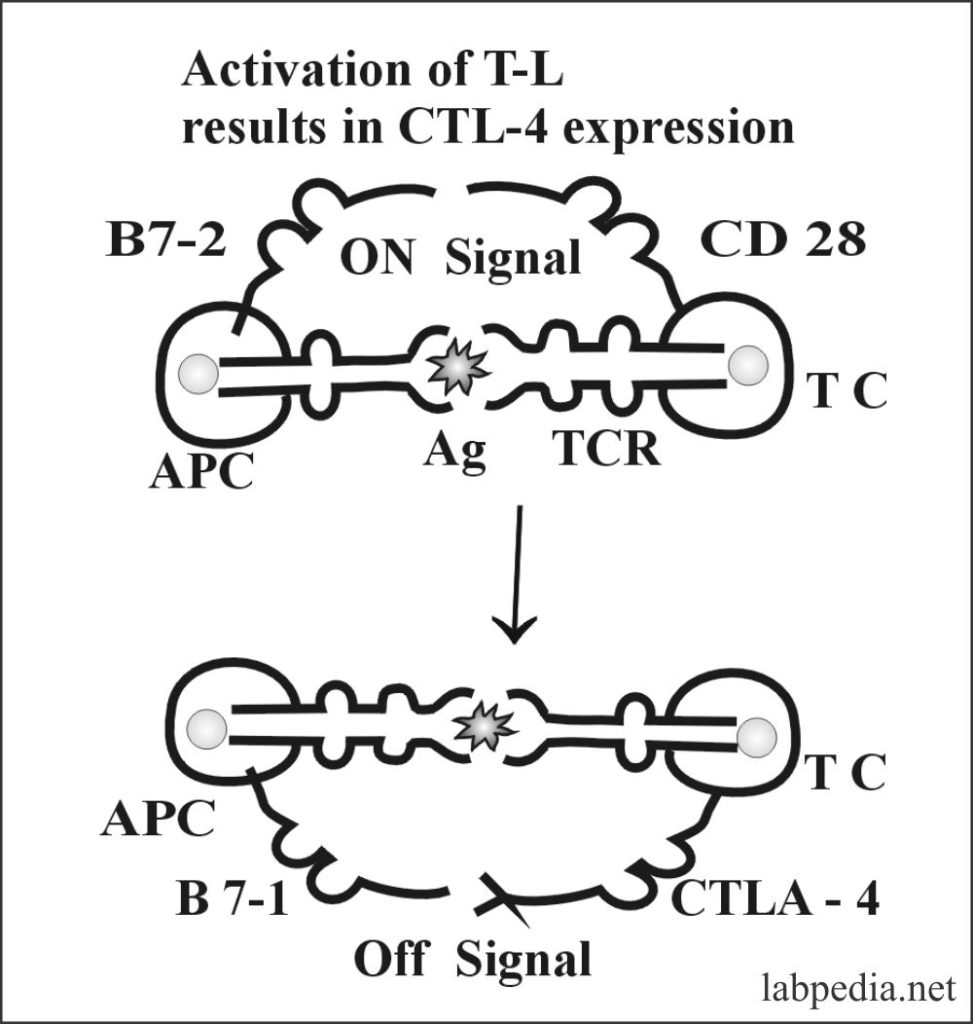
T-cell is activated by the interaction of TCR with presenting Ag (MHC molecule), and there is a second co-stimulatory signal from B7-2—CD28 interaction, that is, on a signal. B7 family is present on APC co-stimulatory molecules CD28/CTLA-4 present on T-cell and their counterpart and B7 family present on APC. B7 group has two main molecules, B7-1 and B7-2. So both CTLA-4 and B7-1 molecules interaction is off-signal. Or, during activation, CTLA-4 (Cytotoxic T-Lymphocytes) is induced, and it is binding to B7-1—CLTA-4 on APC is an off-signal.
B and T lymphocytes are identical by light microscope and E/M appearances. The difference is due to the presence of surface proteins.
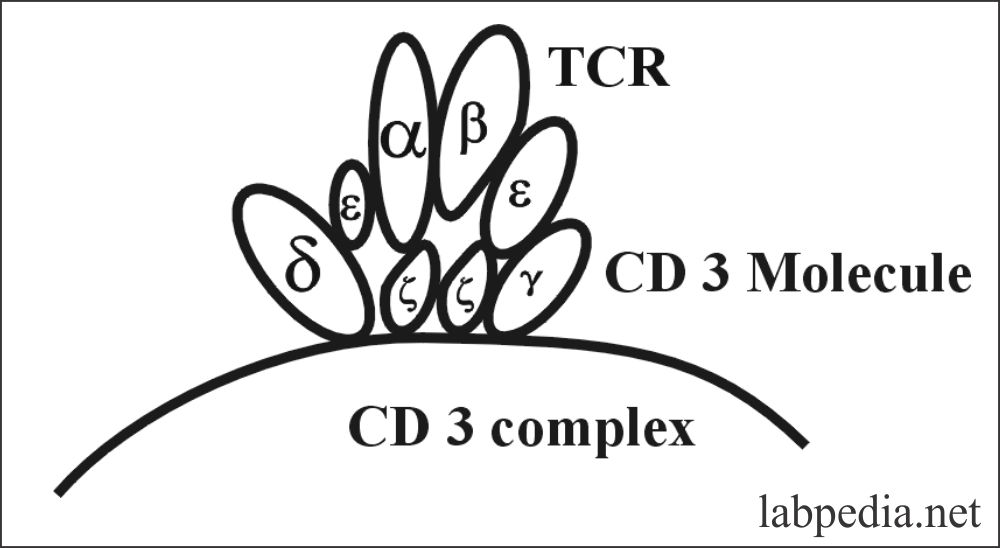
CD3 Molecule
All T-Lymphocytes that express TCR also express the CD3 complex. It is termed as “Pan T-cell marker.” The main function of the CD3 complex is the transduction of signals coming from TCR to initiate cell activation.
CD3 complex is composed of five different transmembrane protein chains denoted by Greek Letters:- γ,δ,ε and ζ.
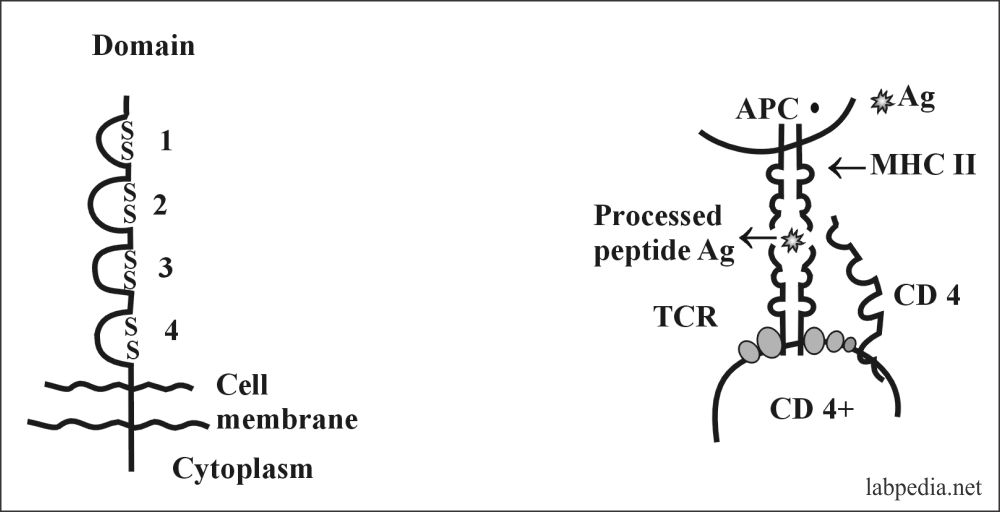
CD4 Molecule
This is membrane glycoprotein with a molecular weight of 55 Kd. It is expressed as a monomer and is a member of the Ig-supergene family. It provides some adhesive forces between interacting cells and provides necessary activation signals.
CD4 molecule has a specific affinity for the MHC-II molecule. It acts as an adhesion molecule for MHC-II.
CD8 Molecule
CD 8 molecule is a disulfide bond linked dimmer. It consists of α-chain (32Kda) and β-chain (34Kda). Each has an Ig-like domain. There is a groove for processed Ag, which is presented along with MHC –class 1 molecule.
It acts like CD4 as an adhesion molecule and binds to the MHC-I molecule with processed antigen.
- B-L and T-L are identical by light microscope and E/M appearances. The difference is due to the presence of surface proteins.
LYMPHOCYTES CLASSIFICATIONS AND CHARACTERISTICS
| LYMPHOCYTES | FUNCTIONS | |
| Th |
CD4+ CD2+ CD3+ α/β TCR |
|
| Ts |
CD8+ CD2+ CD3+ α/β TCR |
|
| Tc |
CD8+ CD2+ CD3+ α/β TCR |
|
| Te |
CD4+ CD2+ CD3+ α/β TCR |
|
| Tm |
CD4+ CD2+ CD3+ α/β TCR |
|
| B-Lymphocytes |
CD19+ CD20+ Surface IgM and IgD |
|
| NK Cells |
CD2+ CD3+ CD16+ and CD56+ |
|
| Null Cells |
No characteristic of T or B-cells Majority posses FcgR |
|
Table VIII- CLASSIFICATION OF LYMPHOCYTES
Differences between B and T-Lymphocytes:
| T-Lymphocytes | B-L | ||
| 1. Site of origin | Thymus |
|
|
| 2. Location |
|
|
|
| Immune response | Cellular | Humoral | |
| 3. Antigen receptor | α/β TCR(¡/d TCR) | BCR (IgM & IgD) | |
| 4. Sheep RBC rosette | + | – | |
| 5. Surface Ig, C3b, Fcg-R | – | + | |
| 6. CD molecule | CD4, CD8, CD2, CD3 | CD19, CD20 | |
| 7. HLA-ABC | ++ | ++ | |
| 8. HLA-D/DR | – | ++ | |
| 9. Receptors For | IL2 -IL1 | C3b, FcγR, EBV, Transferrin | |
| 10. Frequency |
|
80% 85% 65% rare |
20% 15% 35% Many |
| 11. Life span | Long | Short | |
|
12. Mitogen response Sol. Mitogen Radiation |
? + |
+ ++++ |
|
| 13. Functional type | Th, Tc, Ts, Te | The precursor of plasma cells | |
| 14. Polyclonal activation | – | + | |
| 15. Functions |
|
|
|
Table IX – Differences between B and T-Lymphocytes
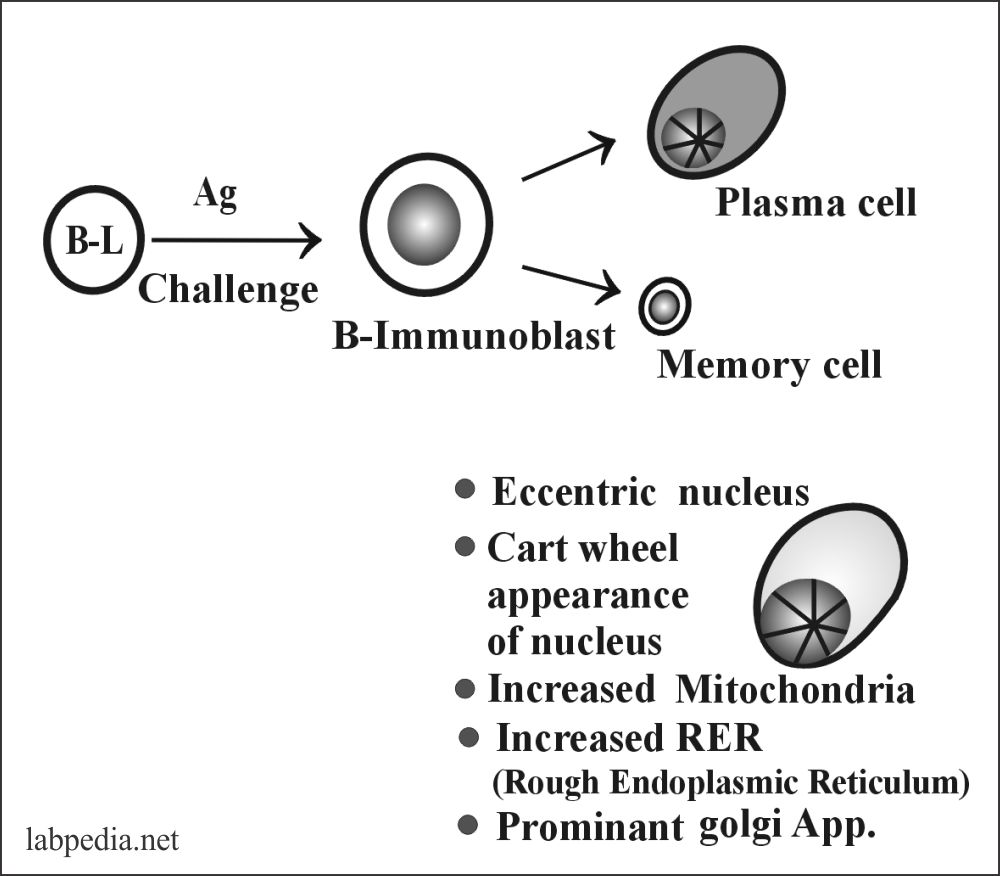
PLASMA CELLS
These are mature, actively antibody-producing cells. These are derived from activated B-lymphocytes into immunoblast and then transform into plasma cells.
- Plasma cell Ag-1
- CD19
- CD20
- CD21
- CD38
Structure of Plasma Cells: The Plasma cells are round to oval in shape, and the nucleus is eccentric. Its chromatin is cartwheel in appearance. Isotype switching and splicing yields and secretes γ, α, ε mRNA
- Plasma cells have no surface Ig.
- Plasma cells are short-lived.
NULL CELLS:
No characteristics of B or T-cell. The majority possesses FcγR, so maybe killer cells in ADCC.
Now, these are basically the Nk cells.
Natural killer cells (NK cell)
Definition:
- NK cells are large granular lymphocytes that lakes:
- TCR-CD3 complex of the T-lymphocytes.
- Surface immunoglobulin characteristic s of the B-lymphocytes.
- These are 10 to 15% of the peripheral blood lymphocytes.
- These cells are derived from the stem cells of the bone marrow.
- These are non-T and non-B cells, previously called Null cells.
- These are infrequent in lymph nodes and thymus.
- Some of these have FcγR, so take part in ADCC.
- No receptor for antigen seen.
- There is no presence of the MHC II molecule.
- These cells produce interferon and IL-2
- These have a receptor for IL-2 & g-interferon
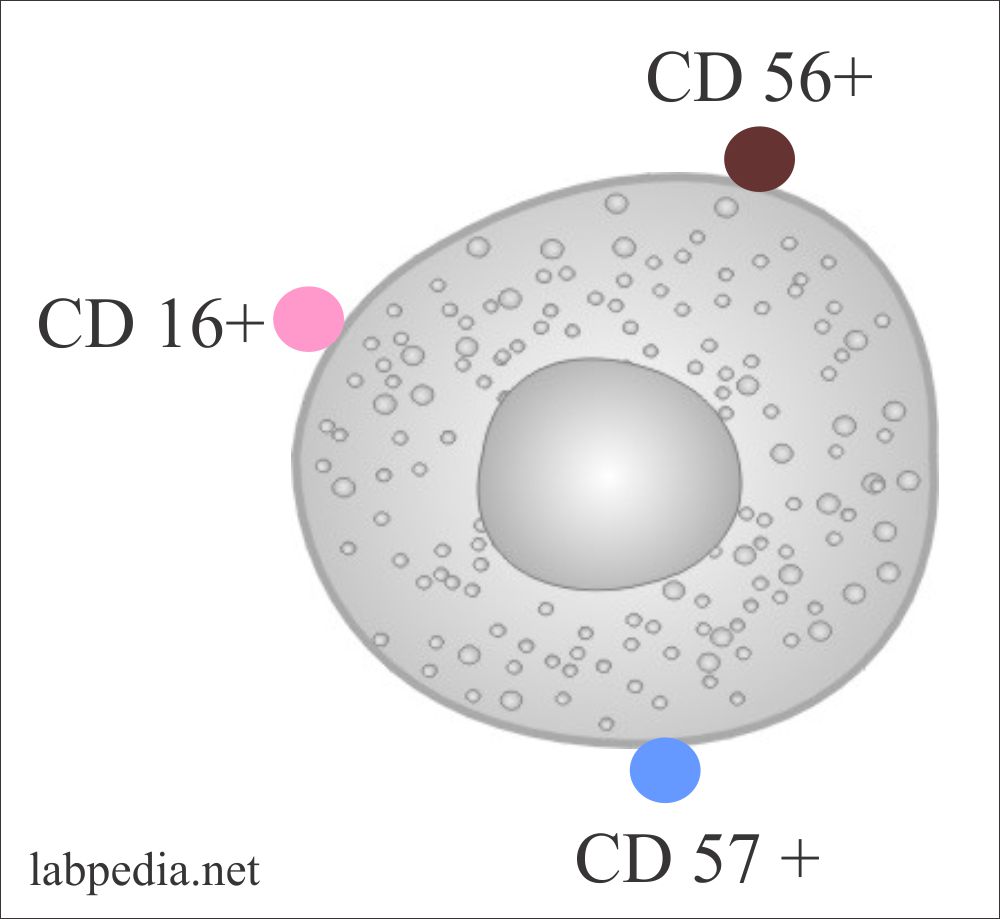
Markers of NK Cells
- NK cells show CD16+, CD56+ CD57+.
- Sometimes CD3+ CD16– most of these are CD3 and TCR negative.
Functions of NK Cells
- Spontaneously cytotoxic to virus-infected cells and even cancer cells because of the presence of azurophilic granules in the cytoplasm.
- The killing of the viruses and the tumor cells are nonspecific without prior sensitization or the presence of cytotoxic antibodies.
- NK cells may also kill the normal cells as well.
- The cytoplasmic granules contain pore-forming protein, which leads to lysis.
- They release γ-interferon which activate phagocytic cells and recruit T-L.
- These may be the first line of defense.
- NK cells can be increased in vitro by IL-2.
- IL-2 proliferate the NK cells and produce IFN-γ, which will promote several immune reactions.
- Interferon increases its killing activity.
- Prostaglandin E2 is highly suppressive of NK-cells.
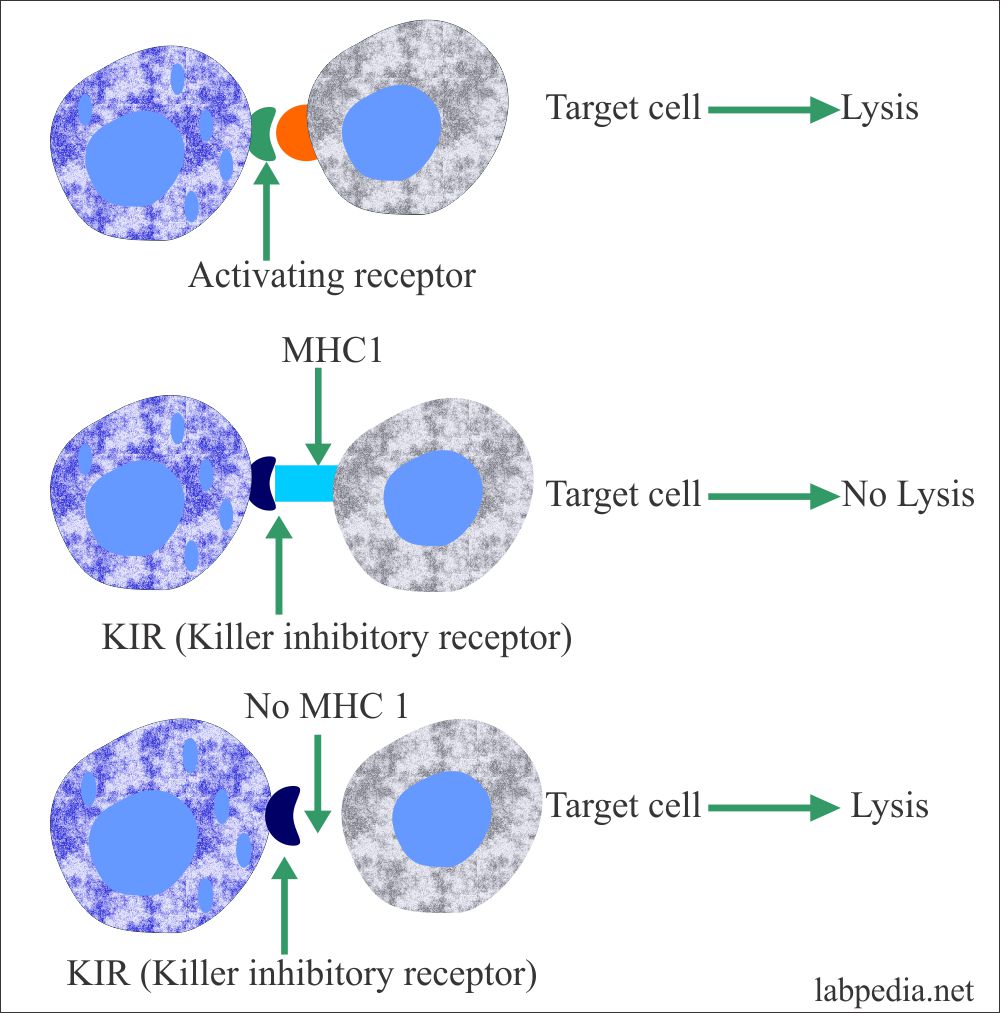
- NK cells have two types of receptors:
- One receptor called the Activating receptor recognizes ill-defined molecules on the target cells and causes lysis of the target.
- The second receptor is called the killer inhibitory receptor (KIR). This will not cause the lysis of the target cells having an MHC1 class molecule.
- When MHC1 class molecules are reduced (or absent) by the viruses or cancer cells, the target cell will be lysed by the NK cells.
ANTIGEN PRESENTING CELLS (APC)
Definition
These are the type of immune cells that enable the T-L to recognize the antigen and gives the immune response against the antigen; these are called antigen-presenting cells (APC). The APC are:
- Langerhan’s cells (Dendritic cells, macrophage family).
- Mature dendritic cells in lymph nodes.
- Macrophages.
- B-Lymphocytes.
APCs are of two types:
- Professional APC expresses MHCII molecules.
- These APCs have MHCII molecules and need co-stimulatory stimulus by CD 80/86 from APC and CD28 from the T-L CD4+ (helper cells).
- Nonprofessional APC expresses MHCI molecules.
Functions of APC
- APC Pick up the antigen.
- APC Process the antigen.
- APC Present antigen along with MHC I and MHC II to T-L.
- MHCII molecule activates the CD4+ cells.
- MHCI molecule activates CD8+ cytotoxic cells.



Hello!
Looking a bit in this immunology textbook, and noticed that high up in chapter 8 you have a table showing in which organs you find the cell types. For the thymus it says that B-cells constitute 100 % of the cells there, but it should be T-cells. Probably an error in constructing the table.
Thanks for a great site!
Best regards
Pontus
It is corrected. Thanks for your comments.
Dear Pontus
I am really thankful for your comment.