Chapter 6: Immunological (Antigen and Antibody) Reactions, Monoclonal Antibody
IMMUNOLOGICAL (ANTIGEN AND ANTIBODY) REACTIONS (OR SEROLOGICAL REACTIONS)
Antigen and Antibody react with each other in three stages:
| Primary stage | Secondary stage | Tertiary stage |
| Combination of antigen + antibody | 1. Agglutination | 1. Opsonization |
| 2. Precipitation | 2. Lysis | |
| 3. Complement activation | ||
| 4. Neutralization | ||
| 5. Blocking of antigen sites |
Primary Stage
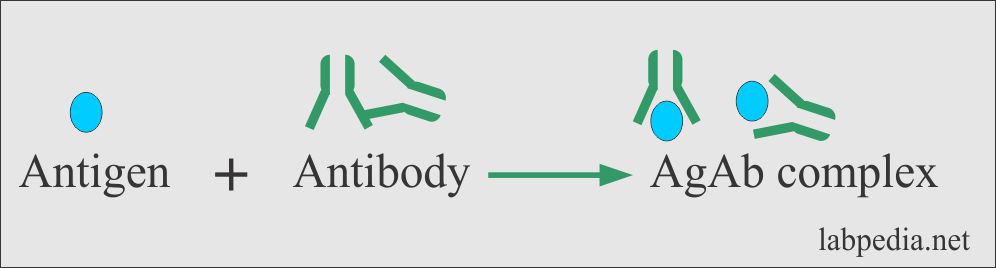
In the primary stage, a combination of antigen and antibody gives rise to antigen and antibody complex formation (Ag + Ab).
Secondary Stage
Agglutination
- Definition:
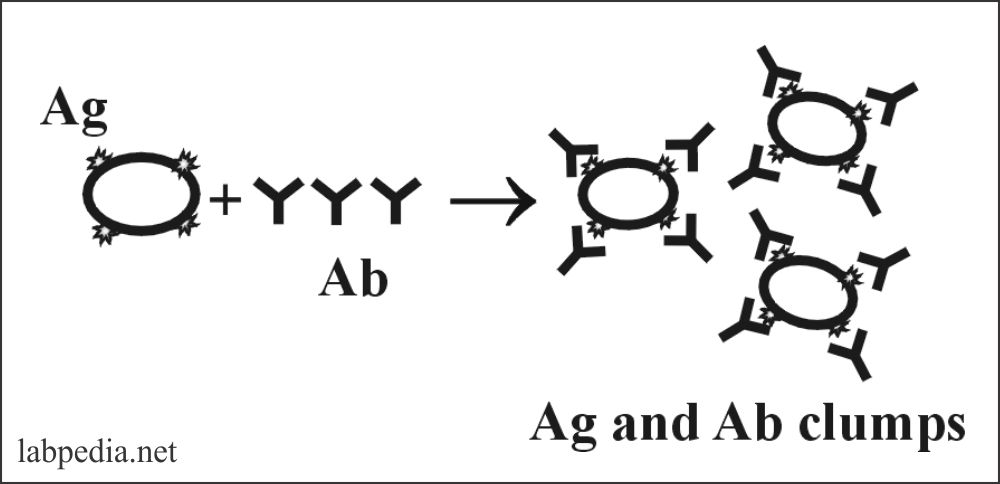
- Agglutination is the visible form of aggregation of antigen and antibody, with the formation of the network in which antigen particle (molecule) alternate with the antibody molecule.
- The ability of the particular antibody to attach with the antigen is its specificity.
- This is the property of the Fab portion called combining sites; a cleft is formed by the hypervariable of heavy and light chains.
- This specificity lies in the Fc portion of the antibody.
- Examples of the carrier are:
- In the case of soluble antigens, latex particles or colloidal charcoal are needed.
- RBCs can be used as a biological carrier.
- Bacteria possess an antigen that reacts with the antibody.
- Quality of the agglutination depends upon:
- Time of incubation of the patient serum, which contains antibody.
- The condition where the tests are run like pH and protein concentration.
- Amount the antigen conjugated with the carrier.
- The antibody, which gives rise to agglutination, is called agglutinin.
- Mechanism of agglutination:
- It occurs in two stages:
- Sensitization is the binding antibody to the antigenic sites.
- Formation of bridges or lattice between antibody sensitized cells.
- The antigen is always in particulate form, and it has multiple antigenic sites.
- First, a combination of Ag and Ab leads to lattice formation when a better fit of Ab (IgM & IgG) to antigen gives rise to larger clumps, which the naked eye can see.
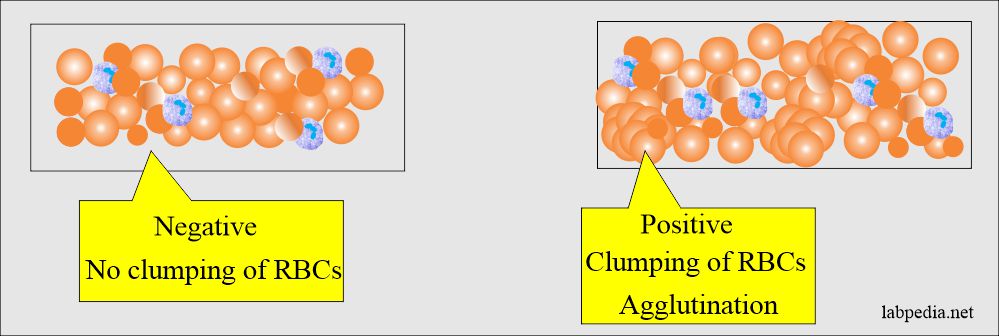
- The best example is the red blood cells; these have antigens on their surface.
- This agglutination depends upon:
- Physical attachment of the antibodies to the antigenic sites on the antigen like the RBC membrane. This will depend on the number of antibodies and antigenic sites on the RBC cell surface. This is called sensitization.
- Lattice formation: This is the cross-linking of the antibodies with the antigenic sites on the antigens.
- It occurs in two stages:
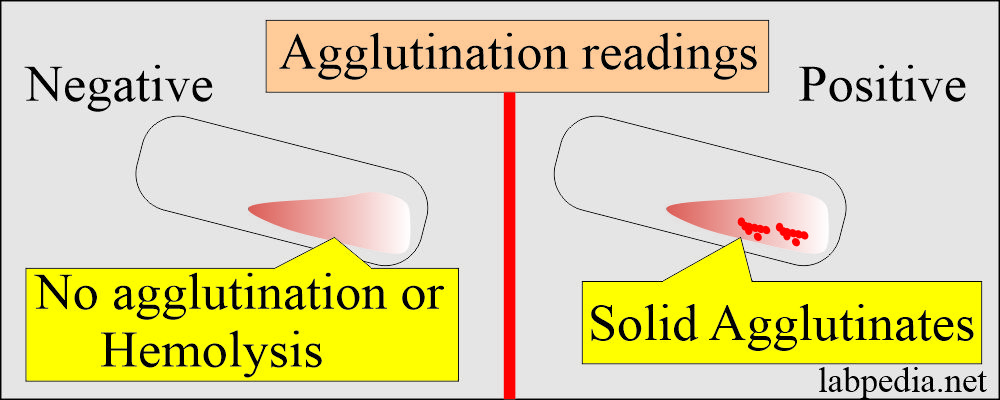
The results of agglutination can be read:
- Directly by the naked eye.
- Under the microscope.
Type of immunoglobulins Degree of agglutination IgG 1+ IgM 3+ IgA 1+ - IgM is considered a complete antibody because of its ability to give good agglutination because it is more efficient than IgG and IgA.
- The incomplete antibody may fail to show agglutination, and these are nonagglutinating. In these cases, the antigenic determinants may be hidden and located deep within the surface membrane or may show restricted movements of their hinge portion, making them functionally monovalent.
- Reading of the agglutination:
Degree of agglutination The appearance of the clumps Supernatant Zero No agglutination is seen Dark turbid Weak Tiny agglutinates can see under a microscope Dark, turbid 1+ Many small agglutinates Turbid 2+ Medium-sized agglutinates Clear 3+ Many large agglutinates Clear 4+ One large agglutinate, no free cells Clear
The examples of Agglutination are:
- ABO blood grouping (blood banking).
- Widal test
- Types of serological agglutination tests are:
- Latex agglutination.
- Flocculation tests.
- Direct bacterial agglutination.
- Indirect or passive hemagglutination test.
- Microplate agglutination reaction test.
- Factors leading to False agglutination results may be due to:
- When the blood is completely coagulated, then you may be seen small fibrin strands.
- When there is increased protein in the patient serum or due to an abnormal protein.
- Patient serum may have an unexpected antibody that reacts at room temperature.
- Patients’ serum may contain transfused or transplanted RBCs or plasma.
- The patient’s RBCs may be coated with an antibody in vivo.
- Reagents or saline is contaminated.
- The reagent potency is degraded due to improper storage.
- Pipettes or glasware are not clean.
- The centrifuge machine is not working properly or not calibrated.
Precipitation
- Kraus’s first time described this was in 1897.
- Definition:
- Precipitation is the formation of relatively small, insoluble aggregates from the antigen and antibody reaction (AgAb).
- The antigen and antibody are soluble.
- The resulting complex is too large, and so it precipitates as an opaque, visible mass, or flocculation.
- The antibodies, which give precipitation, are called precipitin.
- The earliest finding is that antigen and antibody produce precipitation.
- Precipitins (antibody) can be produced:
- Against most of the proteins.
- Some carbohydrate.
- Carbohydrate-lipids.
- Precipitins (antibody) can be produced:
- The antigens are in soluble form; this differs from agglutination, where Ag is in particulate form.
- Antibodies are IgG and IgM.
- Precipitation is just like agglutination in that there is clumping of Ag and Ab.
- Example: Several serological precipitin reaction tests are used like:
- Widal test when done in tubes with dilution methods.
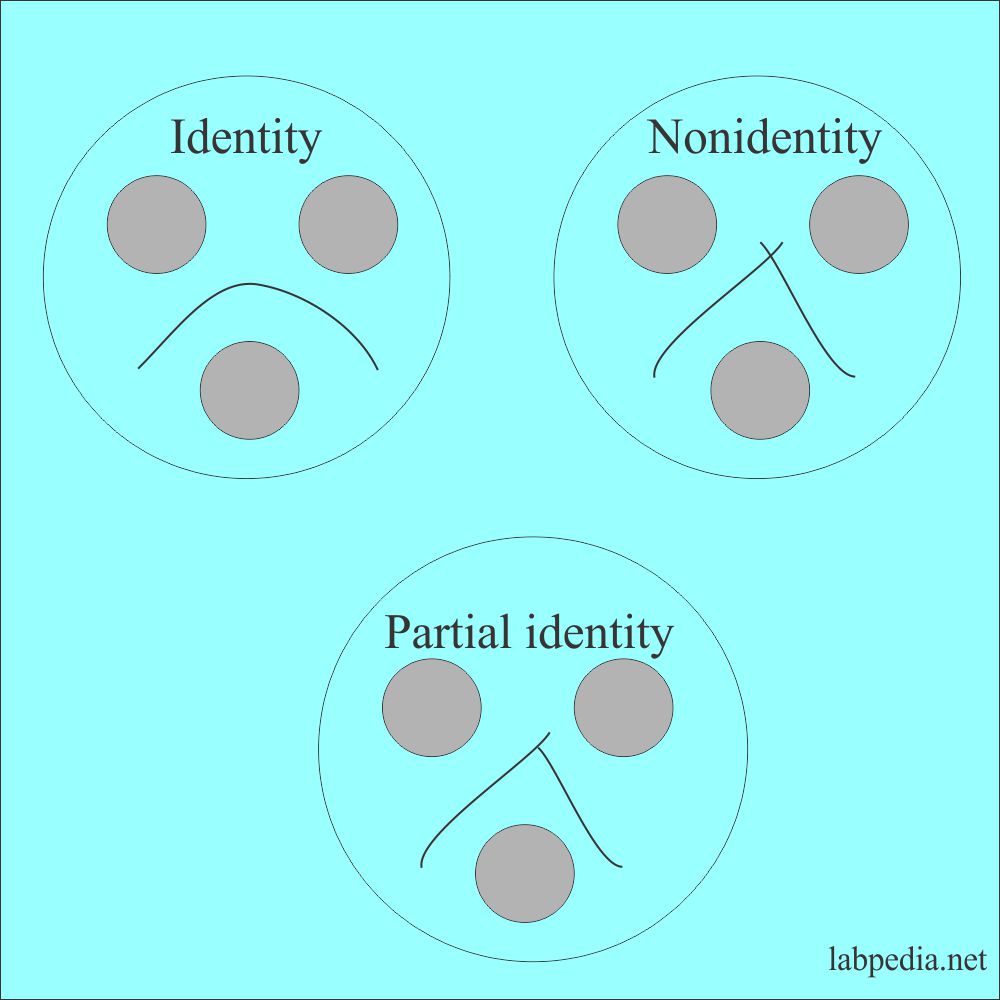
- Double immunodiffusion. It is reported as:
- Identity.
- Nonidentity.
- Partial identity.
- Immunoelectrophoresis.
- Electroimmunodiffusion.
- Countercurrent electrophoresis.
- Radial immunodiffusion (RID).
Neutralization
Definition:
- Some of the antibody-like IgG that can neutralize toxins and viruses are called neutralizing antibodies.
- These antibodies will destroy the infectivity of the viruses.
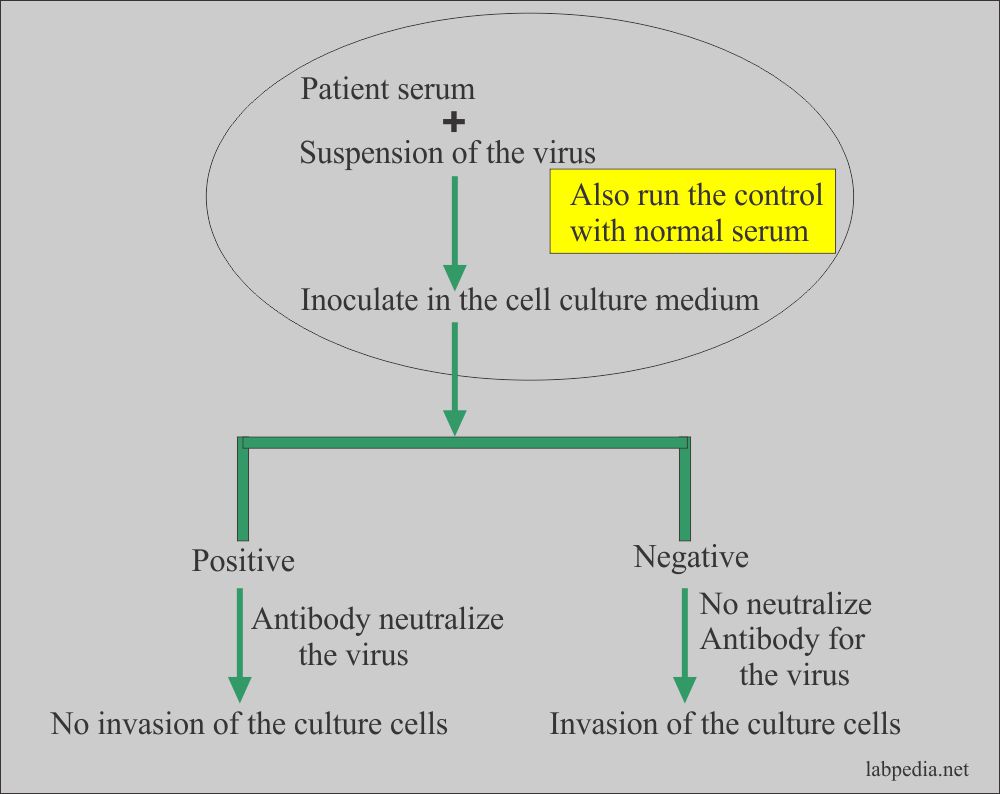
- Procedure to test the neutralizing property of the antibody:
- This test can be done by mixing the patient’s serum with the suspected virus.
- Then keep them in the cell culture media.
- If neutralizing antibody neutralizes the virus, then the cell is the culture will be intact.
Blocking of Antigenic Sites
These antibodies (e.g., IgG) can block the antigenic site, which is not available to antigen; these are called blocking antibodies.
Tertiary Stage
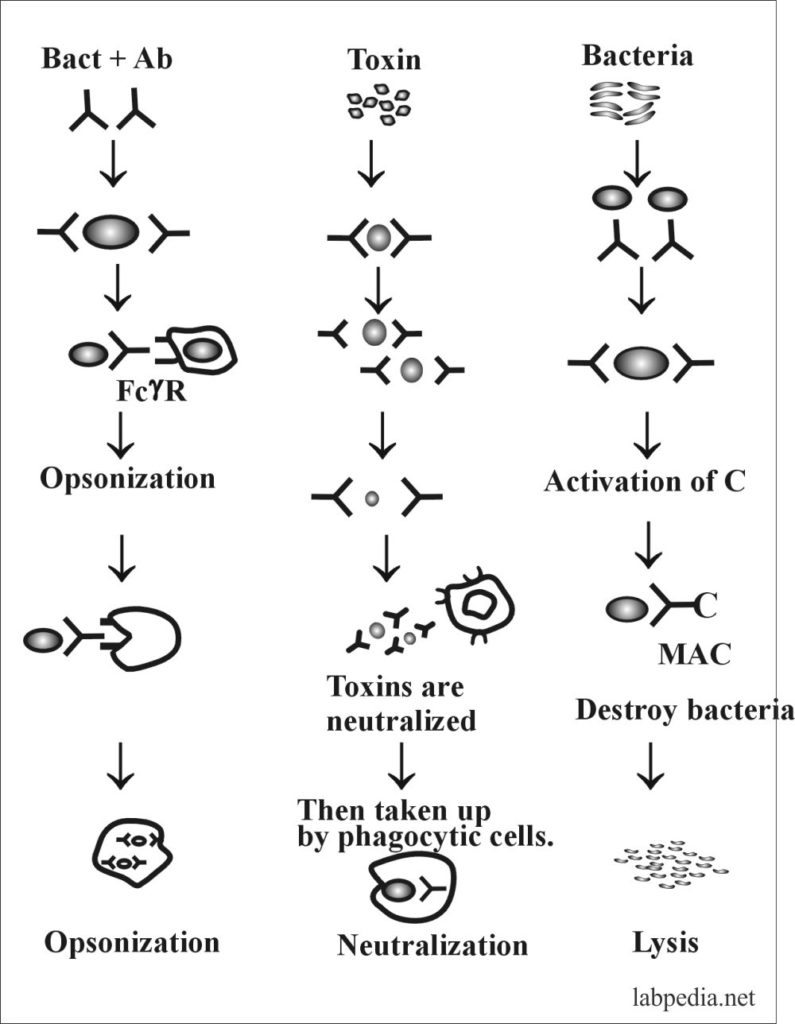
Opsonization
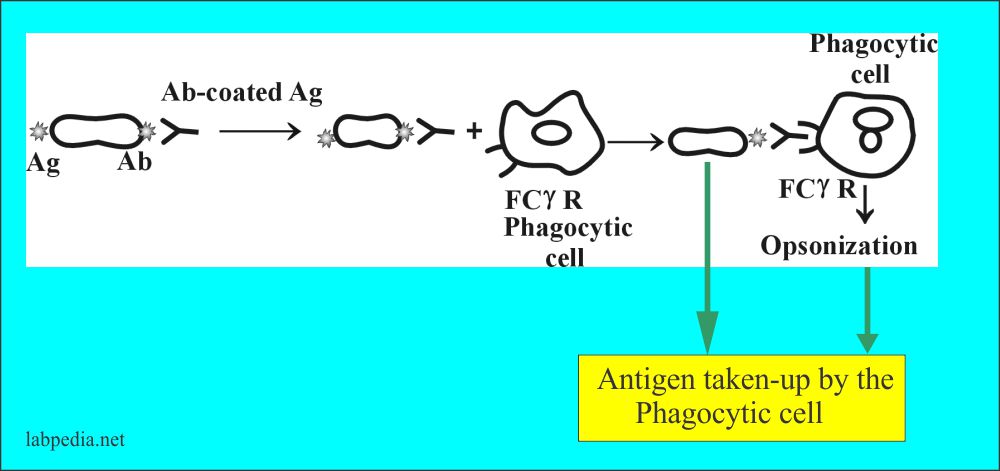
- The antibodies, which give opsonization, are called opsonin.
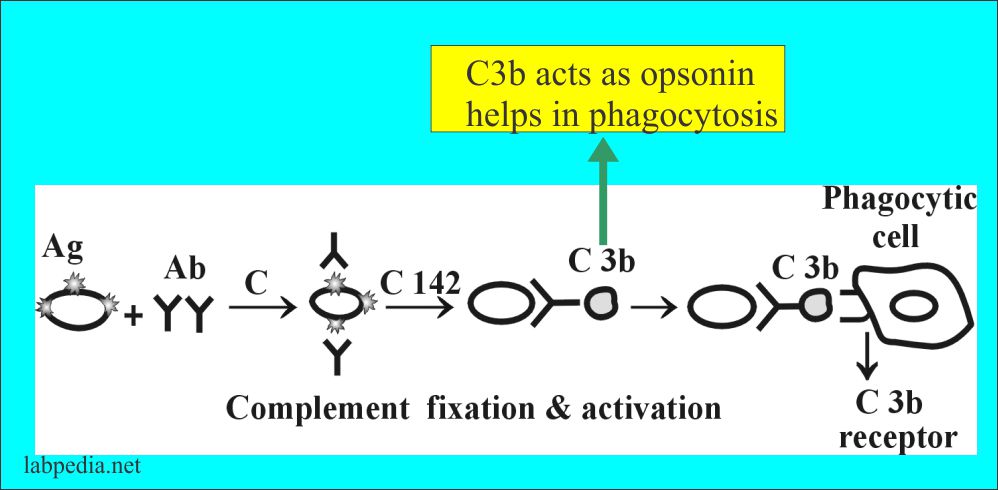
- Another opsonin-like function is C3b.
- The Ab (IgG) helps in the process of opsonization (phagocytosis) by bringing the bacteria coated with Ab (IgG) close to phagocytic cells that possess FcγR (Fcγ-receptor).
- The antibody can activate complement and leads to phagocytosis by C3b because phagocytic cells also possess C3b receptors. This is dependant upon the C3b receptor.
Lysis
- Definition:
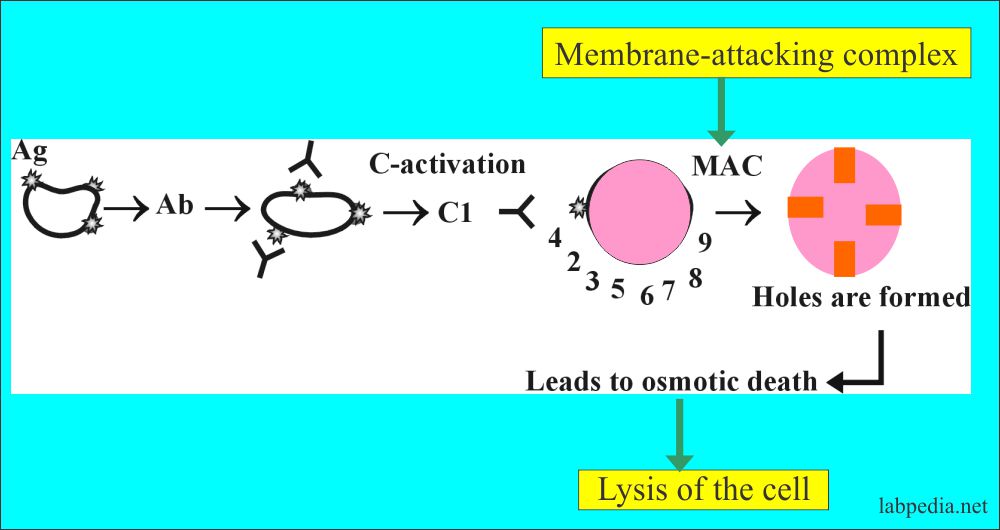
- These are antibodies that lead to lysis (destruction) of the antigens, called lytic antibodies. This cytolysis is complement dependant where complement is activated and leading to lysis of antigens, e.g., hemolysis of RBC.
- Ag & Ab complex is recognized by complement, and there is classical complement pathway activation, making holes formation in the cell membrane and leading to osmotic death.
- The antigen-antibody reaction leads to the lysis of bacterial cell walls, or RBCs are valuable procedures in serological testing.
- Lysis is visible disintegration, showing that antigen and antibody have reacted.
Some scientists divide Antibodies into the following groups:
- Natural
- Induced
- Cross reacting
- Complete
- Incomplete
ANTIBODY ROLE IN HOST DEFENCE
Antibody protects the host by following ways (Functions):
- The primary function of the antibody is to bind the antigen.
- Neutralization of viruses and toxins.
- Opsonization by phagocytic cells is Ab-dependant.
- Complement activation leads to phagocytosis and lysis.
- Activation of complement by IgG1 and IgG3, while IgG2 is less effective.
- IgG can cross the placental barrier.
PRODUCTIONS OF MONOCLONAL ANTIBODIES
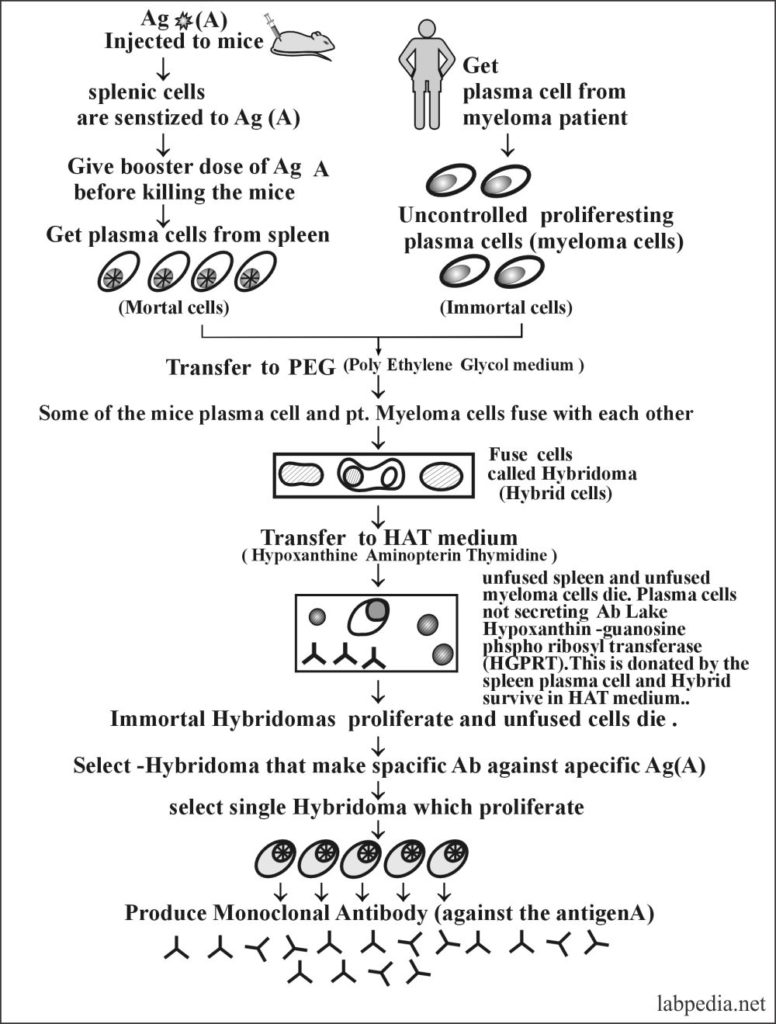
George Kohler and Cesar Milestone invented monoclonal antibodies in 1975, and they were awarded Noble Prize in 1984.
The somatic cell hybridization is the process where they found that some of the hybrids were manufacturing large quantities of specific antisheep RBCs antibodies.
The multiplying hybrid cell culture is called a hybridoma.
The immunoglobulins derived from a single clone of the cells are called monoclonal antibodies.
Definition of a monoclonal antibody:
- Monoclonal antibodies are purified antibodies cloned from single cells.
- These are engineered to bind to a single specific antigen.
- The process of producing monoclonal antibodies takes 3 to 6 months.
This is possible that we can get immortal clones of plasma cells from myeloma patient, which are directed to produce only one type of antibody against a specific antigen for an unlimited period by producing Hybridomas.
After the combination of the patient’s myeloma cells with antigenically stimulated plasma cells from mice will give rise to immortal plasma cells called Hybridoma. These Hybridomas proliferate to produce monoclonal antibodies.