Chapter 28: Immune Deficiency, Immune Deficiency disorders
IMMUNE DEFICIENCY
Definition:
- Immune Deficiency is a failure in the immune system to perform the normal function.
- OR Clinically relevant illness resulting from a defect or deficiency in one or more immune system components, which may be congenital (primary) or acquired (secondary).
- Immune deficiency disorders may be caused by a defect in the quality or quantity of lymphocytes, which may be congenital or acquired.
- This may be combined disorders of B and T lymphocytes or either T lymphocytes or B lymphocytes.
- Immune deficiency disorders reflect an impairment in the mechanism of immunity like:
-
- The defensive part of the body like:
- Skin.
- Respiratory mucosa and its lining.
- GIT mucosa and lining.
- Defective phagocytosis and inflammatory response, including complement and other biological components.
- Cell-mediated delayed hypersensitivity reaction.
- The major congenital or inherited causes are rare.
- The defensive part of the body like:
-
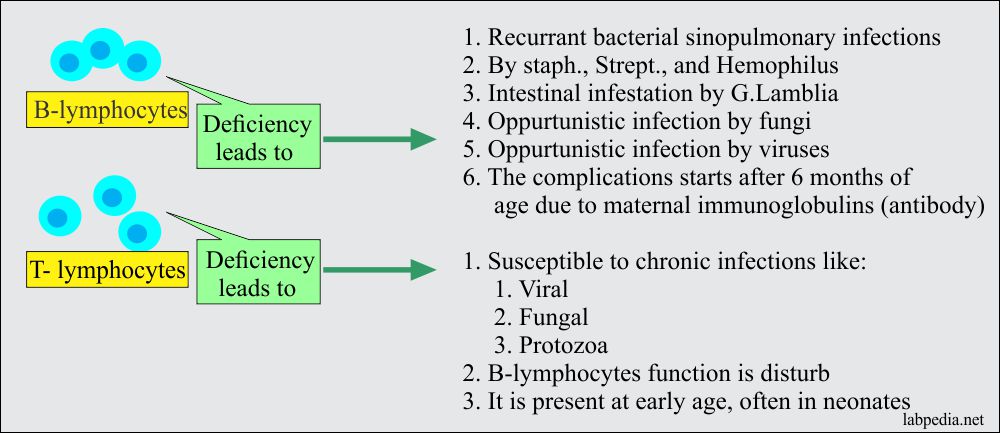
- B-lymphocytes defect (deficiency):
- B-L defect appears after 6 months of the age, that period is covered by the maternal antibodies.
- Defective B-L function is characterized by a recurrent bacterial infection like the sinopulmonary area:
- Staphylococcal.
- Streptococci.
- Hemophilus.
- Intestinal infestation with G lamblia.
- Opportunistic infections are common by fungi and viruses.
- T-lymphocytes defect (deficiency):
- T-L deficiency patients are susceptible to viral, fungal, and protozoal infections.
- These diseases present at an early age often in the neonatal period.
- These cases are often associated with B-L deficiency to a certain level.
- Severe combined immunodeficiency (SCID):
- This is a syndrome characterized by decreased or absent T-L function, low or undetectable immunoglobulins level, and thymic dysplasia.
- This will lead to life-threatening immunodeficiency that is only treated by bone marrow transplantation.
- This disease is due to genetic abnormalities like:
- 50% of the cases are X-linked recessive and due to defects in the IL-2.
- Rest 40% of the cases are autosomal recessive and are due to an enzyme deficiency of adenosine deaminase.
- The third is JAK3 deficiency, purine nucleoside phosphorylase, CD3 deficiency, and RAG1/RAG2 deficiency.
B-L and T-L disorders:
| B-L diseases | T-L diseases |
| Congenital causes | Congenital causes |
| Bruton’s agammaglobulinemia | DiGeorge’s syndrome (Thymic hypoplasia) |
| Acquired causes | Acquired causes |
|
|
The immunodeficiency may be:
- Primary: Due to a defect in congenital or genetic abnormality.
- Secondary: More common and is due to other conditions or therapy like steroids or immunosuppressive therapy.
Deficiency diseases of B and T lymphocytes (Primary/secondary immune deficiency diseases):
| Clinical manifestations | Deficiency of B-lymphocytes | Deficiency of T- lymphocytes | Deficiency of both B and T -lymphocytes |
| Congenital causes | |||
| Bruton’s agammaglobulinemia |
|
||
| Autoimmune diseases | B lymphocytes | ||
| Multiple myeloma | B lymphocytes | ||
| Secondary causes | |||
| AID’s | T lymphocytes | ||
| Chronic lymphocytic leukemia | T lymphocytes | ||
| Hodgkin’s lymphoma | T lymphocytes | ||
| Chronic mucocutaneuos candidiasis |
|
||
| Genetic abnormality based immunodeficiency diseases | |||
| DiGeorge syndrome | DiGeorge syndrome
|
||
| Wiskott-Aldrich syndrome |
|
||
| Ataxia-telangiectasia (Louis-Bar syndrome) |
|
||
| Duncan disease (X-linked lymphoproliferative disease) |
|
||
| B-L various deficiencies |
|
Primary immune deficiency diseases are:
B-lymphocytes related diseases:
- Selective IgA deficiency diseases associated with:
- Allergy.
- Autoimmune diseases.
- Gastrointestinal diseases.
- Central nervous system diseases.
- Pulmonary infections.
- Malignancy.
- Selective IgM deficiency.
- IgG subclasses deficiency.
- X-linked infantile aggamaglobulinmeia.
- X-linked immunodeficiency with hyper-IgM
- Common variable hypogammaglobulinemia
T-lymphocytes related diseases:
- Thymoma.
- DiGeorge’s syndrome.
- Ataxia telengiactasia.
- Wiskott-Aldrich syndrome.
- Chronic mucocutaneous candidiasis.
- Leukocytes adhesion deficiency.
- Combined immune deficiency:
- Swiss-type.
- Thymic alymphophasia.
- Adenosine deaminase deficiency.
- Nezelof syndrome.
Complement deficiencies related diseases:
These are mostly congenital in origin. These patients are more susceptible to recurrent infections.
| Complement deficient | Associated diseases |
| C1 (C1r and C1q) | Gram-positive infection mainly in the respiratory system |
| C2 | Gram-positive recurrent infections:
|
| C3 | Recurrent gram-positive infections |
| C4 |
|
| C5 |
|
| C6 |
|
| C7 |
|
| C8 |
|
| C9 |
|
Secondary causes of immune deficiency diseases:
- Hematological and lymphoproliferative diseases:
- Leukemias.
- Hodgkin’s lymphoma.
- Multiple myeloma.
- Sickle cell disease.
- Aplastic anemia.
- Agranulocytosis.
- Viral infections:
- Acquired immune deficiency syndrome (AIDS).
- Immunosuppressive drugs:
- Corticosteroids.
- Radiation.
- Antimetabolites
- Metabolic and other systemic diseases:
- Diabetes mellitus.
- Malnutrition.
- Aging.
- Nephrotic syndrome.
- Renal failure (uremia).
- Protein-losing enteropathy.
- Liver diseases.
- Surgical procedure:
- Splenectomy.
- Surgical procedure:
- In case of burns.
Classification of immune deficiency:
It is preferable to classify the immune deficiency state according to the immune system’s component rather than classify it as primary or secondary.
| Immune Component deficiency |
Diseases |
| T-lymphocytes Deficiency |
|
| B-lymphocytes Deficiency |
|
| Combined B and T-cells Defect |
|
| Neutrophil Defect |
|
| Complement Deficiency |
|
| Phagocytic NK Cells | Chronic granulomatous diseases |
Table XXVI – Immune Deficiency Disease
Diseases caused by the immune deficiency of B and T lymphocytes:
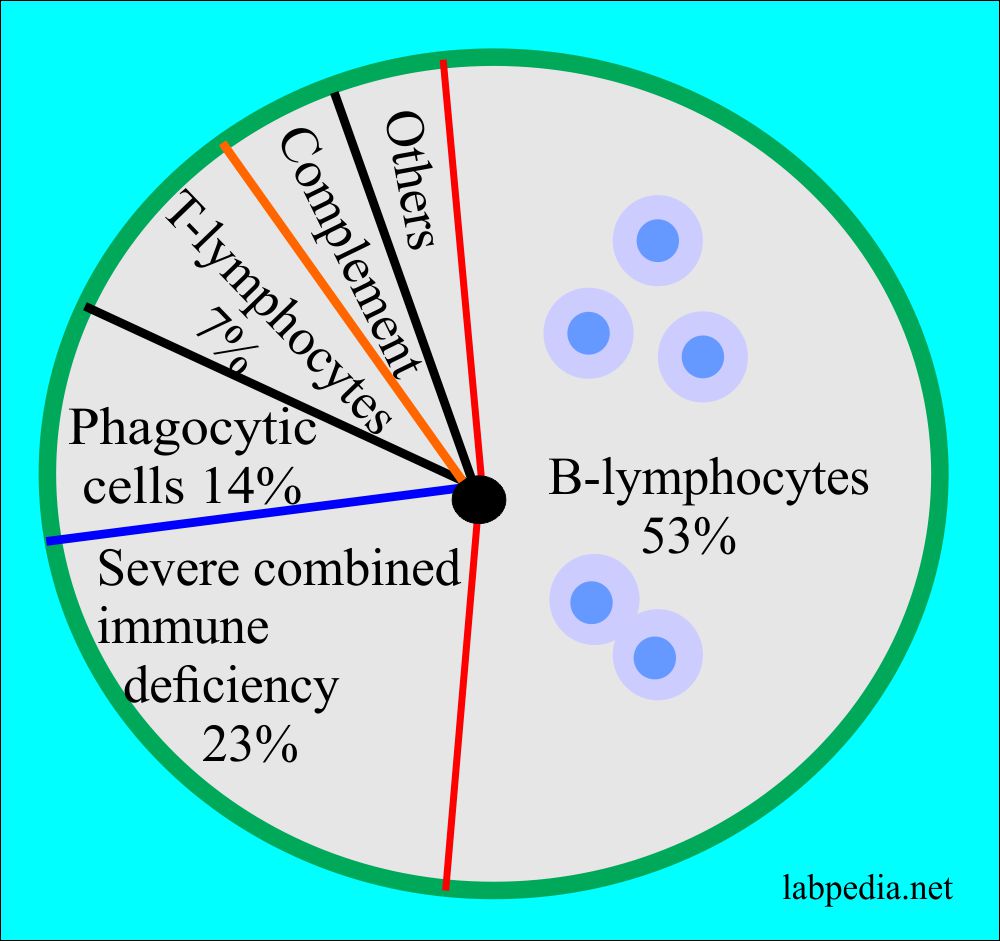
Distribution of the immune deficiency diseases:
- The most common immune deficiency diseases are due to B-lymphocytes disorders is 50%.
- This is followed by severe immune combined deficiency (SCID) is 23%.
- This disorder develops in infants resulting from a lake of both B and T lymphocytes. As a result, there is no formation of immunoglobulins (antibodies).
- Disorders of the phagocytic cells are 14%.
- While T-lymphocytes deficiency is hardly 7%.
Clinical Features of immunodeficiency diseases:
- Immune deficiency may arise at any age, but infections associated with them have several typical features:-
- There is often chronic or recurrent infection.
- These may resolve only partially with conventional therapy.
- Infections are usually severe.
- The organisms involved may be unusual.
- The chances for opportunistic malignancies are more.
Causes of recurrent infections in immunodeficiency:
| a) In B-cells deficiency:- |
|
|
b) T-cells and cell-mediated deficiency:- |
|
|
c) Phagocytic cells deficiency:- |
|
| d) Complement deficiency:- |
|
|
e) T-cells deficiency leading to opportunistic infections:- |
|
Table-XVIII – Infection suggesting immune deficiency (Recurrent infection)
Infective microorganisms in various immune deficiency disorders:
| Infective Agent | B-Lymphocyte (defect) |
T-Lymphocyte (defect) |
Decrease Phagocytes | Deficiency of C – Classical Pathway | Deficiency of C-MAC |
| Bacteria |
|
|
|
|
|
| Viruses |
|
|
|||
| Flagellate parasite |
|
||||
| IntracellularMicro-organism |
|
||||
| Fungus |
|
||||
| Protozoa |
|
|
Table XXVII – Pattern of infectious organisms encountered in immune deficiency
Diagnostic Approach
- Take detail H/O patient, including family history.
- Look for the lymphocytes and other parameters in:
- Peripheral blood.
- Bone marrow.
- Lymph nodes.
- Spleen.
- Thymus.
- Tonsils.
- Enumerate B-cells, T-cells, and macrophages.
- Look for products by the immune response like:
- Ig level.
- Complement assay.
- Look for immune responsiveness like:-
- Mitogenic response.
- Specific Ab-response.
- Rate of H2O2 productions.
- Cytochrome b. content.
Functions of B and T – lymphocytes and their functional tests:
| Tests | T-lymphocytes | B-lymphocytes | Phagocytes |
| Enumeration |
|
|
Neutrophil count |
|
Assessment of invitro function |
|
|
|
|
Assessment of in vivo function |
|
|
Table XXVIII – Useful Screening Tests for the Assessment of Immune Function in Diagnosing Immune-Deficiency