Chapter 23: Autoimmune diseases, Hashimoto’s Thyroiditis and Grave’s disease
AUTOIMMUNE THYROID DISEASES
The spectrum of thyroid autoimmune diseases is vast. There are two major forms of the autoimmune disease of thyroid are known.
- Chronic autoimmune thyroiditis.
- Grave’s disease.
- Chronic lymphocytic thyroiditis (Hashimoto’s thyroiditis) is a classic example of the organic specific autoimmune disease.
- Other thyroid diseases are Transient thyroiditis syndrome and idiopathic hypothyroidism.
There are 1 to 2% of populations in the UK, and the USA has thyroid diseases.
Thyroid autoantibodies are frequently detected in healthy individuals, particularly in women.
More than 2% of older people have autoimmune thyroid disease.
The thyroid produces thyroxine, and it is needed for body growth and metabolism.
HASHIMOTO’S THYROIDITIS (Chronic lymphocytic thyroiditis)
It is also called autoimmune thyroiditis.
Definition
A chronic disease characterized by enlargement (goiter) and dense chronic lymphocytic infiltrates in the thyroid tissue, hypothyroidism.
Age
- This disease can occur at any age. The peak is in middle age.
- Peak age is 3rd to 5th decades of life and more common in the females than the men.
- The fibrous variant is more commonly found in middle-aged and older people.
Sex
- Four times more common in females and in the general population, approximately 0.5%.
- The mode of inheritance is unknown, but there is a strong tendency to inherit the trait to develop toxic antibodies.
- This is seen in the multiple members of the same family.
Signs and Symptoms
- This is the most common cause of sporadic goiter.
- In the beginning, the patient may be euthyroid, but with time, the patient will lose thyroid tissue and develop hypothyroidism.
- The patient will have fatigue, cold intolerance, dryness of skin, anorexia, weight gain, menstrual disturbance, huskiness of voice, mental slowing, and abnormal reflexes.
- There is a week association with HLA. In the UK, HLA DR5 has three times the relative risk.
- Some of the patients may have coexistence of Hashimoto’s thyroiditis and Grave’s disease.
- Gross appearance:
- There is a firm, diffusely enlarged, non-tender thyroid gland.
- The gland enlargement is lobulated.
Microscopically
- There is a loss of colloid in the follicles.
- In the early stages, occasional fibrosis, lymphocytic and plasma cells infiltrate is seen.
- In the florid form, lymphocytes are present in follicles and with the presence of germinal centers.
- There are destruction and distortion of the normal follicles.
- In the lymphoid aggregate, 20% macrophages are seen, while 30% B-L or plasma cells and remainder T-L (with a ratio of CD4: CD8 = up to 4: 1).
- There is a diffuse lymphocytic infiltrate.
- In the advanced stage, the thyroid tissue is replaced by lymphocytes and fibrosis.
Etiology and Pathogenesis
This is an autoimmune phenomenon. The exact mechanism is unknown.
- There are autoantibodies against thyroglobulin.
- Autoantibodies against thyroid peroxidase are found in high titers. This is the enzyme involved in the iodination of thyroglobulin.
- Other autoantibodies are against the thyroid-stimulating hormone receptor.
- These circulating toxic autoantibodies eventually destroy the thyroid gland and produce hypothyroidism.
- There is evidence of T-lymphocytic mediated cytotoxic reaction involving thyroid antigen. Specific T-Lymphocytes are present but are limited.
- This disease is associated with HLA-DR4 and HLA-DR5.
Mechanism
The mechanism of injury may be due to :
- Type II hypersensitivity reaction (Cytotoxic reaction, lysis).
- Cell-mediated reaction.
Laboratory Diagnosis
- TSH level is raised when the patient develops hypothyroidism.
- Later on, followed by the fall in the T4 and T3.
- There are antibodies against:
- Thyroglobulin. There is an increasing titer of the anti-thyroglobulin antibody. It is seen in 4% of the normal population.
- The absence of an anti-thyroglobulin antibody does not rule out the possibility of Hashimoto’s thyroiditis.
- This is also positive in Grave’s disease.
- Occasionally positive in thyroid cancers.
- Also occasionally seen in subacute thyroiditis.
- This may be used to monitor thyroid cancer.
- Thyroid microsomes. Antibodies against thyroid microsomes are found in about 7% of the population, ranging from 1:100 to 1:1600.
- Even its low level (titer) correlates with thyroid involvement by autoimmune disease.
- Second colloidal antigen (CA2 antigen). This is directed against a colloidal protein and can be detected by the immunofluorescent technique.
- This is positive in about 50% of the cases of subacute thyroiditis.
- This is also detectable in some patients with Hashimoto’s thyroiditis.
- Thyroxine (T4) and Triiodothyronine (T3). These antibodies against T4 and T3 are seen in most patients suffering from autoimmune phenomena like goiter and hypothyroidism.
- The thyroid gland’s FNA is also helpful, along with serology, to diagnose the lymphocytic (Hashimoto’s) thyroiditis.
- The biopsy also lymphocytic infiltration with the presence of germinal centers
- Thyroglobulin. There is an increasing titer of the anti-thyroglobulin antibody. It is seen in 4% of the normal population.
various methodology to diagnose thyroid diseases:
| Antigens (antibodies will form against these antigens) | Lab Methods to find these antibodies |
| T4 and T3 |
|
| Second colloidal antigen (CA2) |
|
| Thyroglobulins |
|
| Microsomal antigen |
|
| Thyroid membrane receptor |
|
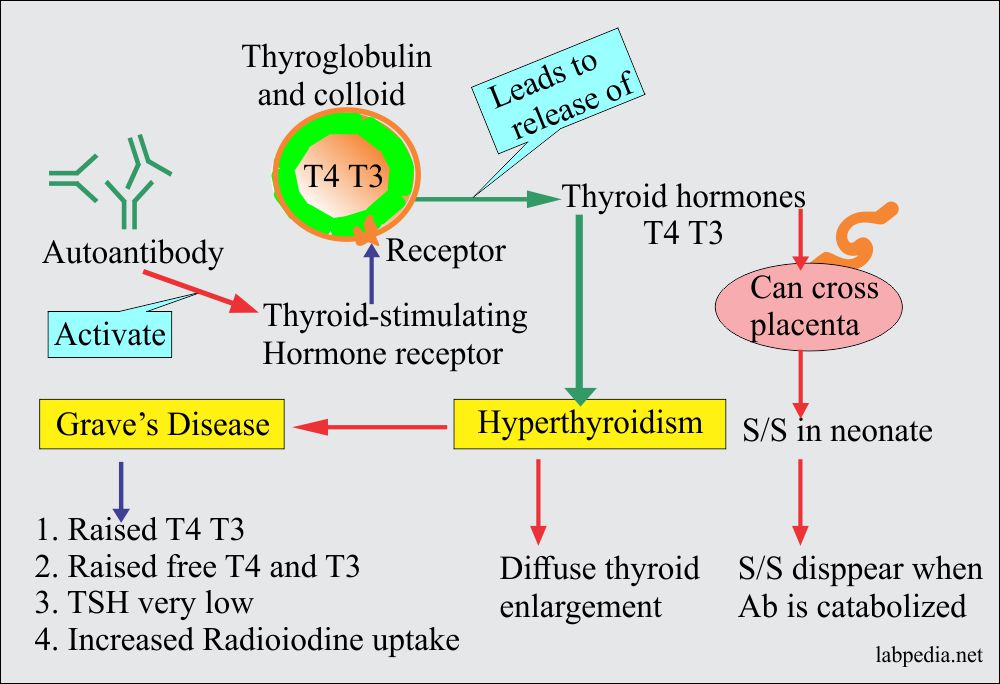
GRAVE’S DISEASE
Definition
Grave‘s disease is characterized clinically by hyperthyroidism and goiter (diffuse toxic goiter).
Age
- Peak age is the third and fourth decades and approximately 0.1-0.5% in the general population.
- In children, this is the most common cause of hyperthyroidism.
Sex
- Typically affecting young adult females.
- Male: Female ratio is 1:7 (seven times more in females than men).
Pathogenesis:
- Grave’s disease is due to the presence of autoantibodies that stimulate the glandular function resulting in hyperthyroidism.
- There are autoantibodies against the TSH receptors.
- A long-acting thyroid stimulator (LATS) binds the TSH receptors and stimulates thyroid hormone production.
- Thyroid growth-stimulating immunoglobulin stimulates the growth of thyroid follicular epithelium.
-
- TSH binding inhibitor immunoglobulin binds to TSH and prevents normal TSH-binding receptors while mimicking TSH function.
- Autoantibodies (IgG type) that compete for TSH for binding to TSH-receptor are now called TSH receptor autoantibody. This autoantibody blocks the TSH receptor site, blocks TSH action, and stimulates the cell through TSH-receptor.
- HLA-DR3 people have a relatively increased risk of four times.
- – Monozygotic twin has disease in 50%.
- – Stress has frequently been blamed as a precipitating factor.
- The differential diagnosis for other causes of hyperthyroidism are:
- Toxic follicular adenoma.
- Toxic goiter.
- Inappropriate TSH secretion.
- Trophoblastic malignancies.
- Struma ovarii.
- Grossly the thyroid is diffusely and symmetrically enlarged without any nodularity.
- The cut surface is uniformly red to brown.
Signs and Symptoms
The patient will have typical clinical features like:
- Palpitation, tachycardia, arrhythmias.
- Sometimes these patients come with atrial fibrillation.
- Patients are irritable.
- Heat intolerance.
- Increased appetite.
- Weight loss, weakness.
- Muscles weakness.
- Diarrhea.
- Proximal myopathy, tremors.
- Ophthalmopathy, there is exophthalmos.
- Pretibial myxedema and thyroid acropachy.
- Thyroid acropachy is swelling of the extremities, clubbing of the fingers and toes due to periosteal new bone formation, and infiltrative ophthalmopathy.
Microscopically
- There is an increase in size and increased vascularity.
- There are hyperplasia and hypertrophy of the gland.
- There is marked hyperplasia of the follicular epithelium. The cells are columnar and basally oriented nuclei.
- The cell’s cytoplasm contains glycogen and fat.
- There are papillae structures without any core.
- Lymphocytic infiltrate is less than Hashimoto’s thyroiditis. The presence of germinal centers may or may not be present.
- Lymphocytic infiltrate predominantly consists of T-lymphocytes with a ratio of CD4: CD8 = 2:1. The T-lymphocytes are CD4 and CD8 positive.
- B-lymphocytes are much less common, approximately 10% of the infiltrate.
- Fibrosis is unusual.
Differential diagnosis
- Isotope scan shows diffuse uptake.
- Autoantibodies, including those to the TSH-receptor, are not used widely for diagnosis.
- Differential diagnosis is from:
- Nodular hyperplasia.
- Papillary carcinoma.
Laboratory Findings
- Elevated T4 and T3, Free T4, and Free T3.
- Low TSH, or often undetectable.
- Thyroid-stimulating immunoglobulin (TSI), this is also called long-acting thyroid-stimulating (LATS), is characteristic of the diagnosis of Grave’s disease.
- Anti-microsomal antibodies are found in 60% of the cases.
- Antithyroglobulin antibodies are found in 30% of the cases.
- In a clinically suspected case, only the following tests are sufficient:
- Free T4.
- TSH.
- Radioiodine uptake.
Treatment
- These patients can be medically suppressed in the hyperthyroid state with or without subtotal thyroidectomy.
- Iodine can be given, which will cause involution of the follicular epithelium and colloid accumulation by blocking the thyroglobulin secretion.
- Radioiodine can be given to destroy the thyroid gland.
- Antithyroid medicine, when given, will suppress the function, and these medicines are:
- Methimazole
- Carbimazole.
- Propylthiouracil.
Prognosis
- If 5 grams of each lobe are left after subtotal thyroidectomy, then mostly the patients become euthyroid.
- The incidence of cancer is like the normal thyroid gland.
Thyroid function tests interpretations:
| Clinical disease | T3 | T4 (total) | T4 (free) | TSH |
| Hypothyroidism | Decreased | Decreased | Decreased | Increased |
| Hyperthyroidism | Increased | Increased | Increased | Decreased |
| Grave’s disease | Increased | Increased | Increased | Decreased or very low |
| Single toxic nodule | Increased | Decreased |