Chapter 21: Autoimmune diseases, Hypersensitivity Angitis like Polyarteritis Nodosa, Henoch-Schonlein’s Purpura, Wegner’s Granulomatosis
POLYARTERITIS Nodosa (PAN), Henoch-Schonlein’s Purpura
Definition
Polyarteritis nodosa is a systemic hypersensitivity disease involving medium-sized arteries that usually spare the lungs. Still, frequently there is the renal glomeruli’s involvement, nerves (mononeuritis multiplex), mesenteric lymph nodes, and the skin.
Polyarteritis Nodosa is a disease characterized by swelling of the medium-sized vessels, associated with fibrinoid necrosis and inflammatory infiltrate representing non-infectious necrotizing vasculitis. As a result, there is aneurysm formation and vessel occlusion.
Henoch-Schonlein’s Purpura is also hypersensitivity of the blood vessels like Angitis affecting the small arteries of the skin, gastrointestinal tract, and joints.
Age: – Mostly seen in middle age.
Sex: – More common in males. The male: female ratio is 3:1.
Sign and symptoms
- A renal angiogram shows an aneurysm.
- It is a life-threatening condition with end-stage renal failure in 30%, and other complications are malignant hypertension and cerebrovascular accidents.
Pathogenesis: – It is completely unknown. It may be due to hypersensitivity to:
- Drugs like sulphonamide, phenylbutazone, and thiazide.
The mechanism of injury is a type III hypersensitivity reaction (immune complex disease).
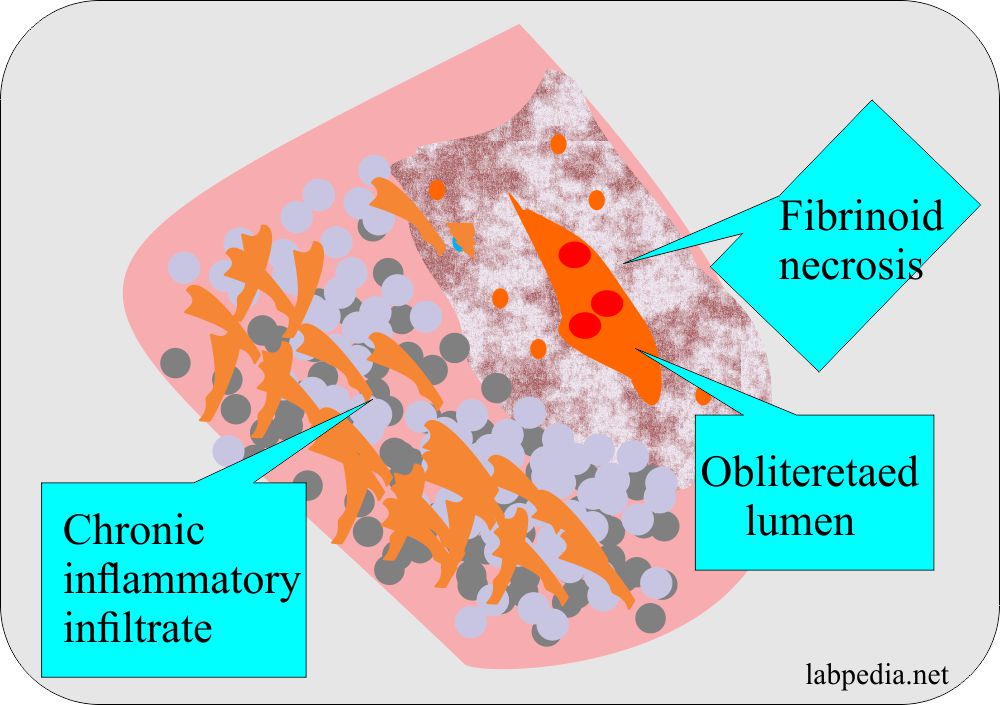
Microscopic Histology
- The affected vessels show segmental fibrinoid necrosis of the vessel wall with intense infiltrate of lymphocytes, plasma cells, and macrophages.
- The segmental nature of the involvement, with active and healing lesion next to the blood vessels’ normal segment, is highly characteristic.
- There is symmetrical involvement, which gives a nodular aneurysm called Nodosa. Common complications are thrombosis and infarction.
Diagnosis
- There may be raised ESR and leucocytosis. There is mostly eosinophilia.
- CRP positive and rarely raised Immunoglobulin.
- Renal angiogram.
- Muscle biopsy may be diagnostic to see vascular changes.
- A minority of the patients show pANCA(antineutrophil cytoplasmic antibodies).
Treatment
Aggressive therapy with corticosteroids and cytotoxic drugs are needed to control the disease.
Prognosis
With aggressive therapy 5 years, survival is more than 60%.
WEGENER’S GRANULOMATOSIS
Definition
This is necrotizing vasculitis affecting the respiratory system,e.g., Middle ear, sinuses, and lungs.
Also, there is the involvement of the kidneys.
In this case, vasculitis is seen in the lungs and kidneys.
This is a systemic vasculitis associated with a granulomatous lesion in the upper and lower respiratory tract, usually preceding the onset of glomerulonephritis. Friedrich Wegener first described this condition.
Age
It is seen in late middle-aged males and the elderly, while the mean age of 45 years.
Sex
It is more common in males.
Etiology and Pathogenesis
- This is more common in HLA-DR2, and there is increased relative risk 3 to 4 times.
- In the patients, there are ANCA-antineutrophil cytoplasmic antibodies. The main debate regarding the various types of ANCA is whether they are involved in the disease process or are generated secondarily.
- Autoantibody to the neutrophilic cytoplasmic antigen (ANCAs) is associated with various autoimmune diseases.
- In Wegener’s granulomatosis, the antibody against the proteinase-3, a cytoplasmic antigen (C-ACNA), is found.
- Antibodies to P-ANCAs are characteristics of vasculitis and glomerulonephritis.
- These antibodies’ role in the pathogenesis appears to be small, but these have important diagnostic values.
Clinical Features
- Respiratory lesions may lead to epistaxis or hemoptysis.
- Constitutional systems like fever, malaise, and weight loss reflect the systemic nature of the illness.
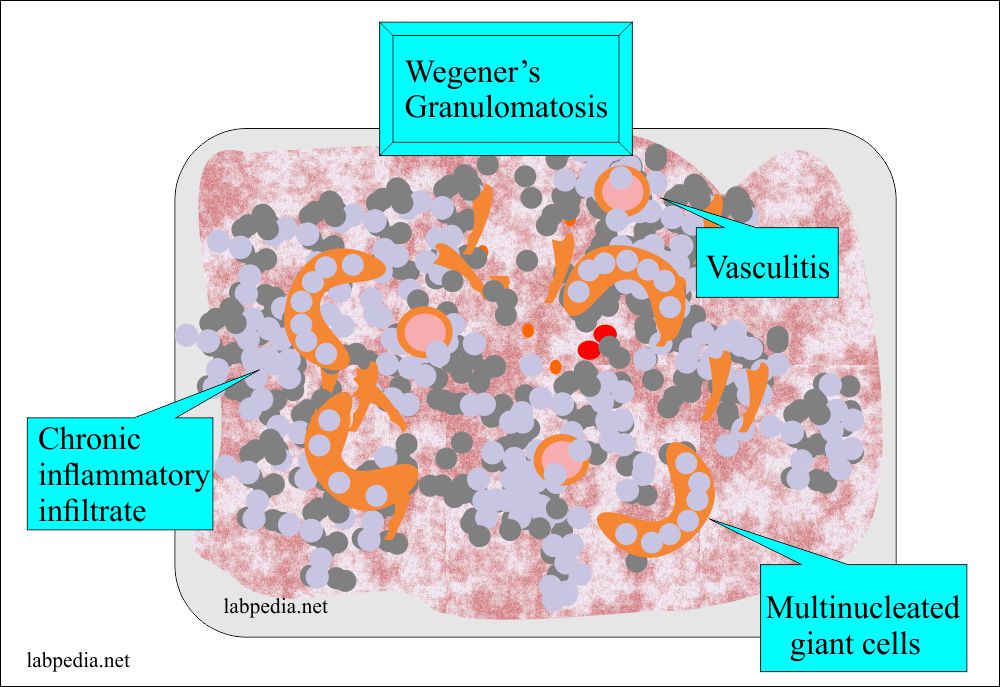
Microscopic Picture
- Typically there is focal, proliferative glomerulonephritis often associated with necrosis and crescent formation.
- There is a rapidly progressive (necrotizing) glomerulonephritis.
- The typical lesion in the kidneys is focal segmental necrotizing glomerulonephritis.
- The respiratory tract shows granuloma, which consists of necrosis, infiltration by lymphocytes and macrophages, and multinucleated giant cells.
- In the lungs, there is the involvement of small, medium-size arteries, arterioles, and venules.
- There is a necrotizing vasculitis.
- The necrotizing granulomatous vasculitis is characteristic of Wegener’s granulomatosis.
Diagnosis
- Biopsy from the respiratory tract shows granuloma.
- The measurement of cANCA is specific and can be used to know the response to treatment.