Chapter 20: Autoimmune diseases, Progressive Systemic Sclerosis (PSS), and Scleroderma
PROGRESSIVE SYSTEMIC SCLEROSIS (PSS)
Definition
Systemic sclerosis (Scleroderma) is a chronic disabling condition of unknown etiology, characterized by fibrosis of the skin, blood vessels, and internal organs, e.g., lung, heart, kidney, and gastrointestinal tract.
PSS is a generalized disorder of the connective tissue, characterized by fibrosis and degenerative changes in the blood vessels, skin, skeletal muscles, synovium, and internal organs like kidneys, lungs, and heart GIT.
PSS or scleroderma have various presentations. Eosinophilic fasciitis is also considered one of this type.
This is associated with various professions and drugs.
Types: It has two types:
- Localized morphea, scleroderma, is a limited cutaneous form in which skin thickening is limited to the distal extremities and face (scleroderma).
- Diffuse progressive systemic sclerosis (PSS), there is more severe diffuse cutaneous involvement and the internal organs.
- There may be overlap in the above two types.
Age: Third and fourth decades of age, but no age is immune.
Sex: This is more common in females with a Male: Female ratio of 1:2 to 5 ( three times more common in the females.).
Etiology and Pathogenesis
- The exact cause is unknown.
- The basic problem is the increased deposition of collagen.
- Occupational exposure to:
- Vinyl chloride.
- Silicosis.
- Bleomycin sulfate.
- Tryptophane.
- Carbidopa.
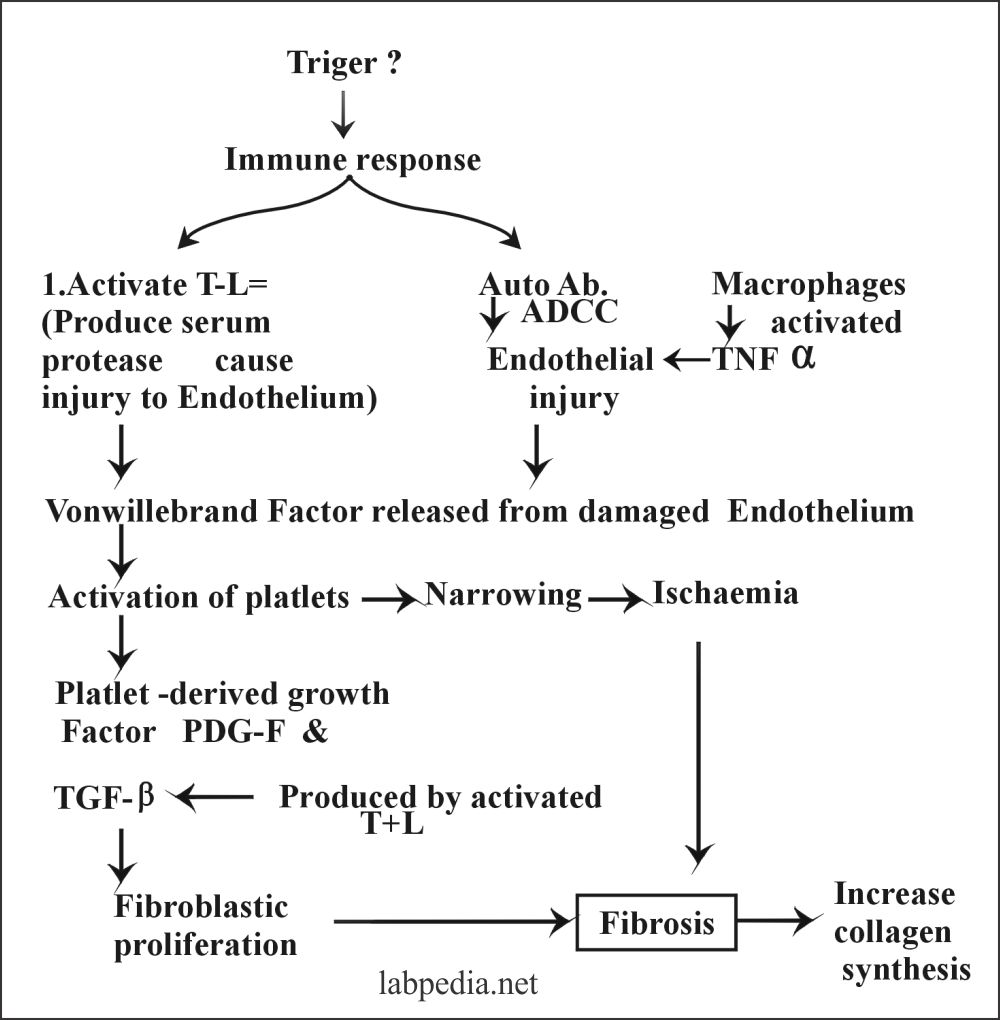
The pathogenesis of Progressive systemic sclerosis is based on the following changes:
- Microvascular injury.
- Humoral, serological findings.
- 40% to 90% shows ANA bodies, and these antibodies are formed against:
- Extractable nuclear antigen.
- Against nucleolus.
- Against centromere.
- Scl-70
- The anti-centromere antibodies are specific for patients with Scleroderma and CREST syndrome (calcinosis, Raynaud’s phenomenon, esophageal dysfunction, sclerodactyly telangiectasia).
- 40% to 90% shows ANA bodies, and these antibodies are formed against:
- The cell-mediated immunity role in PSS. T-lymphocyte hyperactivity indicates disease progress.
- Activated T-cells can result in both vascular changes and increased collagen formation in the case of scleroderma.
- It is believed that vascular changes and fibrosis result from cellular immune activation.
- Activated T-cells produce cytokines, which leads to vascular injury.
| Microvascular Injury | Humoral Serologic Abnormalities | Altered collagen synthesis |
|
1. Recurrent injury to Endothelium 2. There is a serum factor 3. cytotoxic to endo- thelium 4. Auto Ab damage the Endothelium. 5. Endothelial injury 6. Platelet aggregation. 7. Narrowing 8. ischemia is a stimulus for fibroblastic proliferation and leads to Fibrosis. |
1. Ig is raised by 50%. 2. ANA, present in 70-90%. 3. R.Factor, present in 25%. 4. Scl-70, present up to 70%. 5. Anti- centromere Ab, present in 80-90%. All these indicate a humoral disorder. |
1. It is increased collagen synthesis but It is all normal form. 2. Abnormal CMI and attract and activate fibroblast and leads to increase collagen synthesis. 3. T-L, IL1, and TNF-α attract and activate Fibroblasts. 4. The result is fibrosis |
Table XXV – Pathogenesis of Progressive Systemic Sclerosis
Signs and Symptoms of PSS and Scleroderma:
- The first presentation is usually Raynaud’s phenomenon preceding other systems by months or years. It is typically triggered by cold, and the patient will have pallor and/or cyanosis of fingers followed by redness.
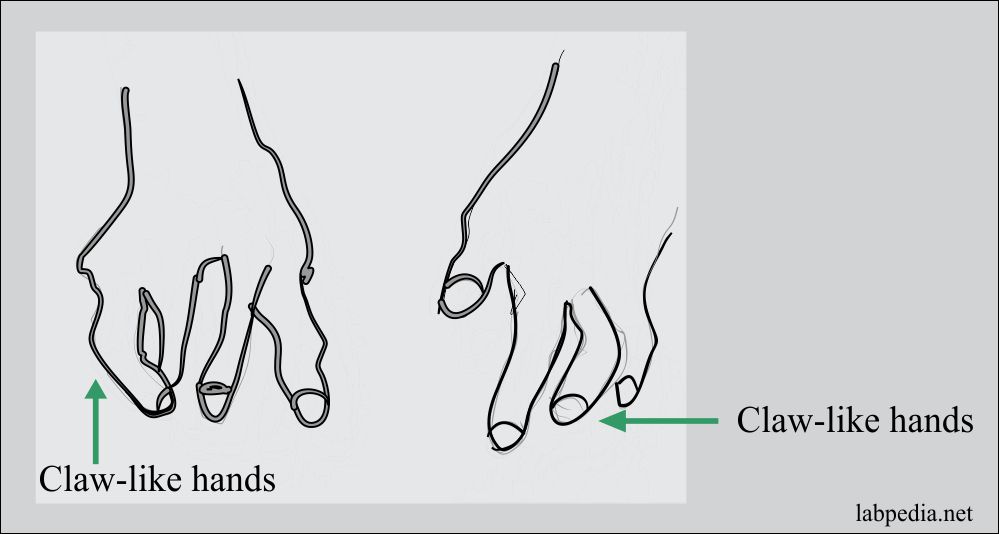
- Skin involvement leads to a limitation of movements as an extension of digits. The involvement of the face shows the loss of wrinkles and microstomia. There is a loss of hair.
- Arthritis symptoms sometimes resemble rheumatoid arthritis.
- Pulmonary fibrosis is frequent and pulmonary hypertension only appears in 10% of the patients.
- The patient may have pleuritis, pericarditis, and cardiac fibrosis.
- Renal involvement is rare but is fatal.
- Scleroderma (idiopathic) is considered an autoimmune disease because of autoantibodies associated with the disease.
- There is an overlap of other autoimmune diseases like Scleroderma-polymyositis and scleroderma-SLE.
- While progressive systemic sclerosis is a multisystem disease-causing thickening of the skin (Scleroderma) and other organs’ involvement.
- >50% of the case starts with Raynaud’s phenomenon before the start of other clinical manifestations.
- Involvements of the joints are common.
- Another common clinical feature is the hypomotility of the gastrointestinal tract.
Morphology
Virtually all organs are involved.
1. Skin
- Scleroderma shows only the skin’s involvement and is a localized disease compared to PSS, a multisystem disease.
- Bundles of collagen bind the skin to the underlying tissue.
- Changes take place in three stages.
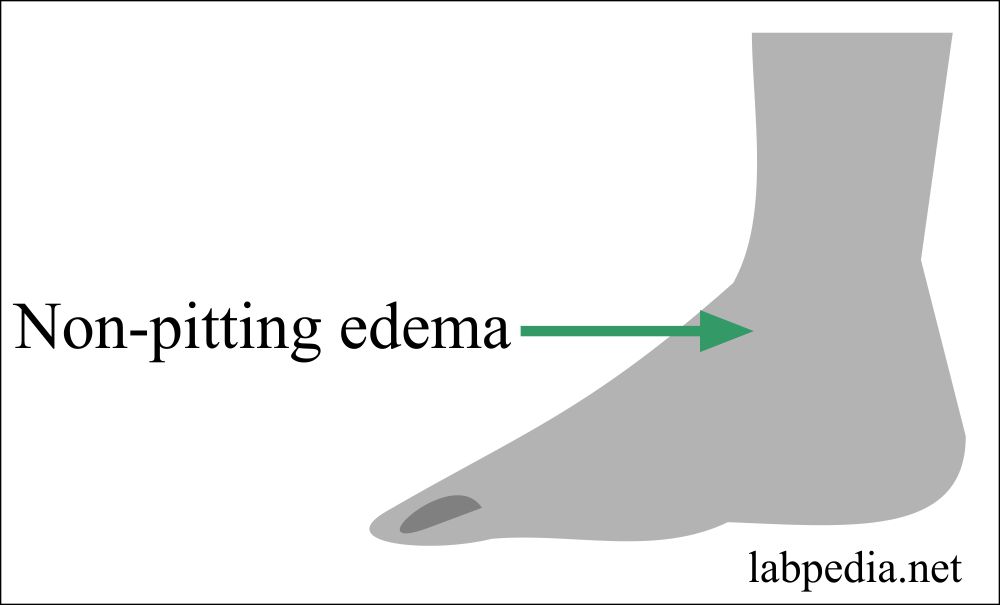
Stage I: There is edema, which is non-pitting and microscopically shows edema, perivascular lymphocytic infiltrate, capillaries and small arteries are thickened, and collagen deposition.
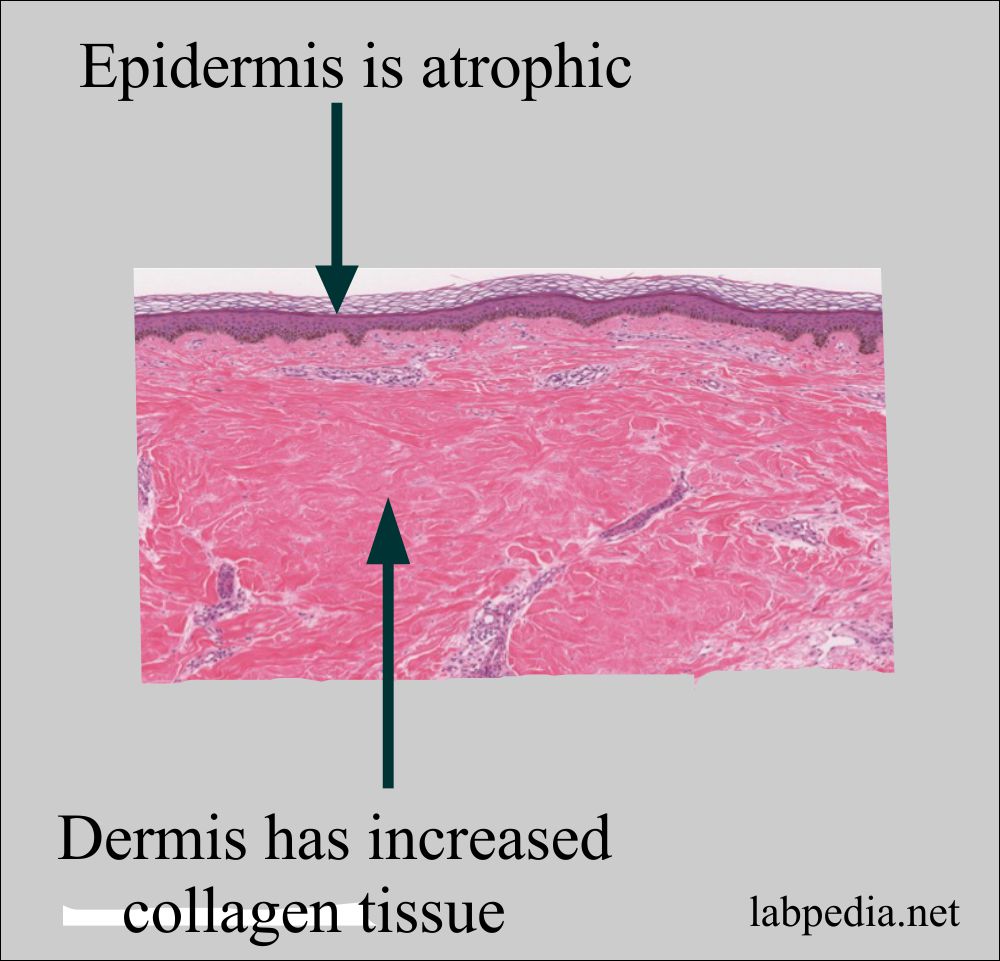
Stage II: Due to an increase in collagen formation, wrinkles disappear. The epidermis becomes thin.
Stage III: This is the atrophic stage where claw-like hand, the face is drawn and mask. Microscopically there is atrophy of the epidermis and increase collagen. Calcification may be seen.
- In the late stages, due to loss of blood supply, ulceration may take place.
Skin involvement may be a part of CREST syndrome. Where:
| Abbreviation | Clinical presentation |
| C | Calcinosis |
| R | Raynaud’s phenomenon |
| E | Esophageal involvement |
| S | Sclerodactyle (localized sclerosis of the fingers) |
| T | Telangiectasia |
2. Gastrointestinal
Gastrointestinal involvement is seen in >50% of the cases. The esophagus show thin mucosa, frequently ulcerated, covers abundant collagen deposition in the lamina propria, submucosa, and serosa. The esophagus will show a rubber-hose appearance and is inflexible. There are mononuclear cells infiltrate. Similar changes are seen in other segments of the gastrointestinal tract.
3. Musculoskeletal system
There are inflammatory synovitis and fibrosis in the muscles.
4. Liver
Sometimes may see primary biliary cirrhosis.
5. Lung
There is diffuse fibrosing alveolitis.
6. Kidney
There may be involvement in 2/3 of the cases. There is a thickening of the intima of interlobular arteries and fibrinoid necrosis of the intima and media of afferent arterioles. The patient may show hypertension in 30% of the cases.
7. Blood vessels
These may show vasculitis.
Diagnosis
- There is normochromic and normocytic anemia. Also, there are raised ESR.
- Increased Immunoglobulins.
- The biopsy of the skin and muscles is diagnostic.
- The synovial fluid shows mainly neutrophils.
- Radiological findings show a narrowing of the joint spaces.
- One-fourth shows a low titer of rheumatoid factor.
- Also, show scl-70 (Ab against DNA-topoisomerase 1).
- Antinuclear autoantibodies are considered to be specific for systemic sclerosis.
- ANA is positive in 90% of the cases.
Prognosis
It is not good, 50% die in 2-3 years.
Treatment
- It is symptomatic.
- For Raynaud’s phenomenon, keep hands warm and reduce stress.
- Renal hypertension may be controlled by drugs blocking the Renin-Angiotensin system (captopril, enalapril).
- Esophagus and intestinal hypomotility can be improved with metoclopramide.