Chapter 18: Autoimmune Diseases, Rheumatoid Arthritis (RA)
RHEUMATOID ARTHRITIS (RA)
Definition
Rheumatoid Arthritis is a multisystem chronic inflammatory disease of unknown etiology, particularly involving smaller peripheral joints and commonly leading to cartilage destruction. There is the involvement of the joints and synovial membranes. In cases, there is systemic involvement as well.
Rheumatoid arthritis (RA) represents an unusual patient response to one or more etiological factors. An infection etiology is possible but still not established.
Epidemiology:
It is quite common in chronic conditions in the USA. In the USA,>2.5 million people are suffering from RA.
In most of the populations, it is 1% to 2% where these studies were done.
RA occurs worldwide, and there is no geographical or climatic variation in the incidence that has been documented.
RA is more prevalent in the first degree of relatives having RA.
Age:
70% of the cases are seen in the second and third decades but may also be seen at any age. The peak age is 35-50 years.
But this disease can start at any age.
Older and obese persons are risk factors for arthritis.
Sex:
Again, this is a females disease with a male: female ratio of 1 : 3 to 5. Women, two to three times, are more likely than men for the RA.
Distribution:
RA has a worldwide distribution with a prevalence of 1% approximately.
Major Immunologic Features
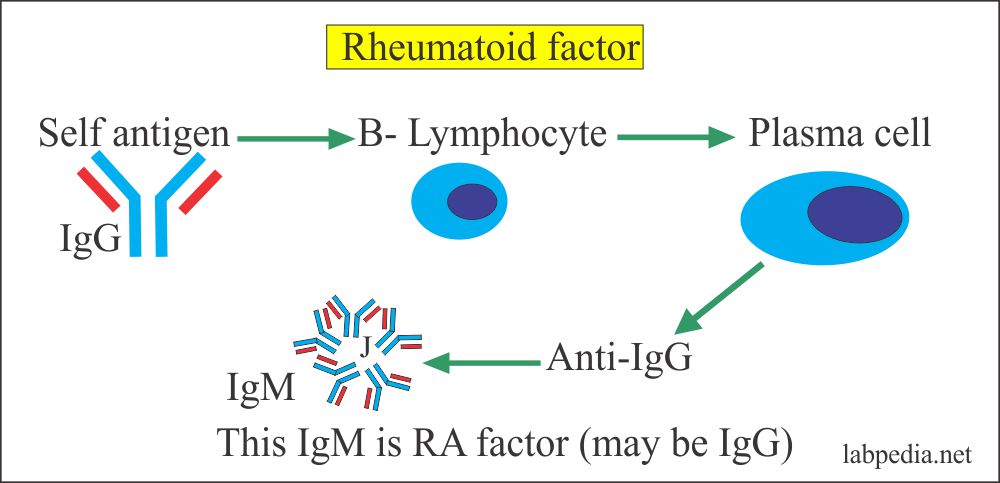
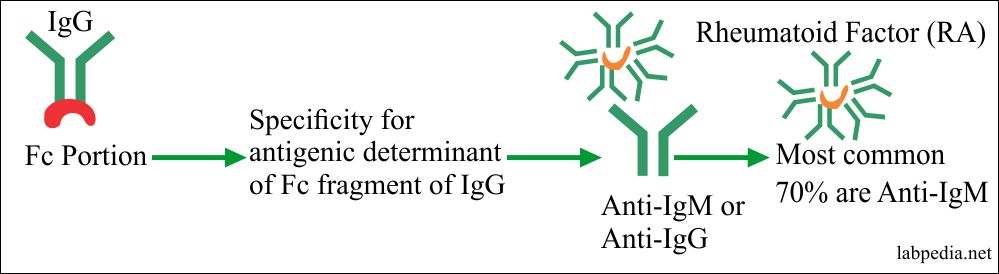
- Presence of rheumatoid factor, which may be IgM and IgG.
- There is a decrease in the complement level.
- Increase the level of β-Microglobulin.
- There is a synovial fluid formation.
Pathogenesis
- Genetic Role: This is the genetic component’s role. There is familial clustering of the disease, more common in monozygotic twins than dizygotic twins, and more common in HLA – DR1 and HLA – DR4.
- Unidentified environmental factors cause alteration in HLA-Ag, and this may be due to viruses.
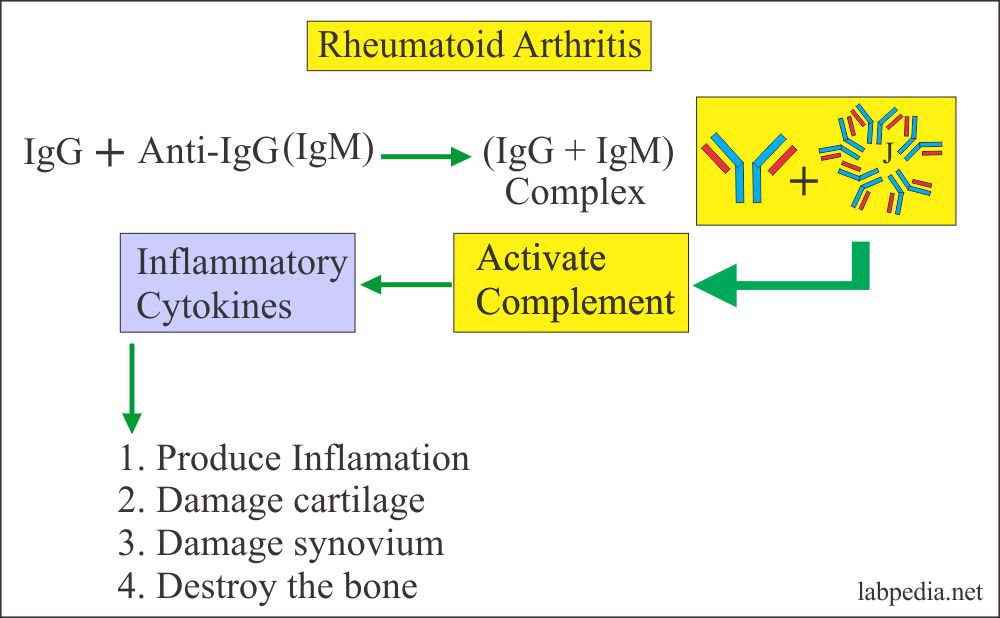
- The viruses may stimulate B-L which produce antibody against IgG, and there is IgG + Anti-IgG complex formation, which leads to local arthritis reaction.
- Viral Role: Possibly EBV, which may suppress Ts or give rise to polyclonal activation of B-L; other viruses blamed are Herpes, Rubella, and Mycoplasma.
- The etiology of the viruses or bacterial is never proved.
- Synovial lymphocytes produce IgG, which is recognized as foreign and give rise to immune complex (IgG + Anti IgG). There are autoantibodies to IgG, IgA, and IgM, known as Rheumatoid factors (RF).
Mechanism of Injury
Any stimulus, maybe microbes, stimulates the synovial B-L against the Fc portion of IgG and gives rise to anti-IgG-Ab, predominantly IgM (Pentameric form). Other Ab IgG and IgA may also be found. Now immune complex forms (IgG + Anti – IgG) activate complement and lead to damage to cartilage with PANNUS formation.
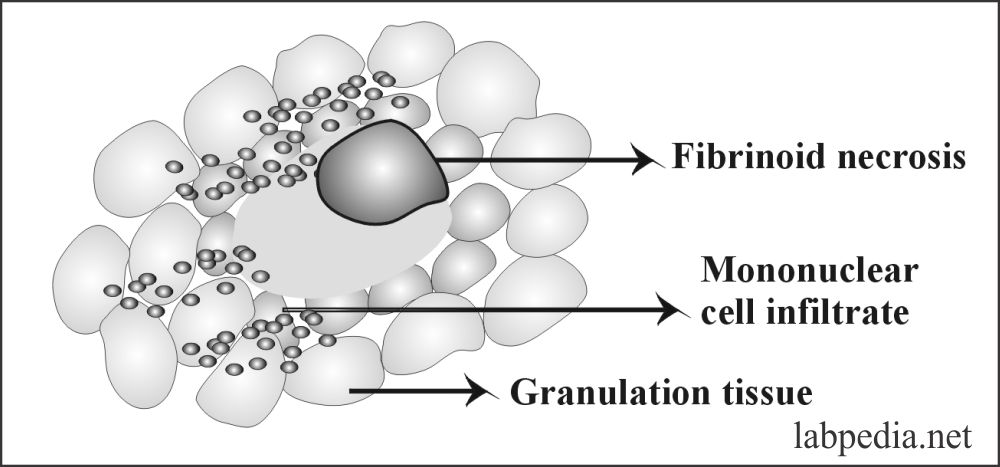
Pannus
Its formation is by hyperplasia and hypertrophy of the synovial lining with a microvascular injury with tissue edema. Synovial tissue protrudes into the synovial cavity are called Pannus. It consists of inflammatory exudates with mononuclear cells infiltrate surrounding vessels, and these consist of T-L, macrophagic cells, and B-lymphocytes.
Rheumatoid Nodule: An extra-articular manifestations. It consists of central fibrinoid necrosis surrounded by palisading macrophagic cells and an outer zone of granulation tissue.
Signs and Symptoms
- The start of the synovitis inflammation is the initial lesion.
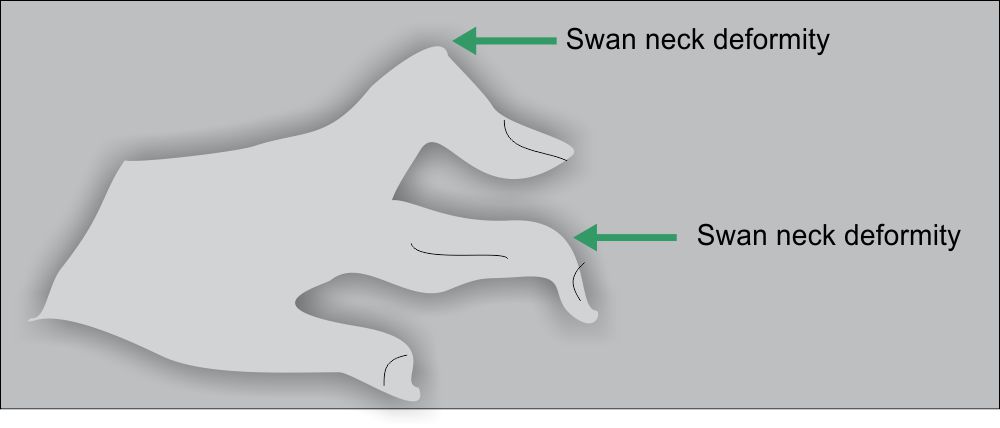
- Deformities of smaller joints (hand & feet) are commonly seen as “Swan-neck.”
- There is an ulnar deviation, dorsal interosseous muscle deformity.
- There is swelling of the wrist characteristic of RA.
- Extraarticular presentation of Rheumatoid Arthritis:
- These patients may have malaise, fever, and weight loss.
- Skin: The rheumatoid nodules in the skin are seen in 20% of the cases.
- Cardiovascular system—Involvement is uncommon and may see as constrictive pericarditis.
- Lung: Coal-miners workers show lungs’ involvement (pleuritis and diffuse fibrosing alveolitis), and polyarthritis is called Caplan’s syndrome.
- Felty’s syndrome: In these patients, there is splenomegaly, neutropenia, anemia, and thrombocytopenia.
- Lymphoreticular system often there is a regional enlargement of lymph nodes, and maybe enlarged liver and spleen.
- Ocular: Sometimes, there is keratoconjunctivitis sicca.
- Blood vessels: There is vasculitis.
- Amyloidosis may be seen as a complication.
Revised criteria by the American Rheumatism Association for the diagnosis of a Patient for Rheumatoid Arthritis:
Four of the seven criteria are required to classify the patient as having rheumatoid arthritis.
- If the following symptoms are present for 6 weeks, then the patient can be labeled Rheumatoid arthritis.
- Morning stiffness: This is present around joints in the morning and lasts at least one hour before any improvement.
- Arthritis of 3 or more areas: The physicians observe at least 3 joints. There is soft tissue swelling or fluid in the joints.
- There is possibly involvement of 14 joints areas.
- Right & left proximal interphalangeal, wrist, elbow, knee, ankle, and metatarsophalangeal joints.
- Arthritis of hand joints: This is arthritis of the hand joint, and at least one area is swollen in the wrist.
- Metacarpophalangeal and proximal interphalangeal joints.
- Symmetric arthritis: – There is simultaneous involvement of the same joint area on both sides of the body.
- Rheumatoid nodule: – These subcutaneous nodules present over the prominence of bones are observed by the physician.
- Rheumatoid factor: This rheumatoid factor is positive, while only 5% show positive tests in the control group.
- Radiographic changes: – Typical changes like erosions are seen. Even may see bony decalcification.
- If the following clinical criteria are found, then in that case-patients will have very severe RA. These are prognostic markers:
- High serum level of IgM rheumatoid factor.
- Early radiographic and functional deformities.
- Presence of some of the HLA class II.
- If the following clinical criteria are found, then in that case-patients will have very severe RA. These are prognostic markers:
Diagnosis
- A complete blood picture shows lymphocytosis, thrombocytosis, and raised ESR. There is normochromic and normocytic anemia.
- The ESR will be raised to a variable level. The level may correlate to the severity of the disease.
- Serum electrophoresis shows an elevated level of α-2 and gamma globulin fractions.
- γ-globulins increase is polyclonal.
- There is a mild to moderate decrease in albumin level.
- Synovial fluid examination shows mainly neutrophils (75%). The rheumatoid factor may be positive. Also, there is the presence of the immune complex (IgG +Anti IgG).
- Arthrocentesis is the aspiration of the synovial fluid, and this fluid analysis rules out the possibility of gout, septic arthritis, and calcium pyrophosphate dihydrate deposition disease. This also rules out the possibility of RA and SLE.
- Radiological findings show a narrowing of the joint spaces.
- Rheumatoid Factor (RF):
- Blood sample:
- Take venous blood to prepare the serum.
- A random sample can be taken.
- Immunological tests show rheumatoid factor (RF) positive in more than 70%.
- This is predominantly pentamer IgM but may see the presence of IgG, IgA, and IgM (monomer). Rheumatoid factor may be positive in SLE (30%) and Sjogren Syndrome (90%).
- RA factors correlate with:
- The severity of the disease.
- Involvement of the other organs like vasculitis, Felty’s syndrome, and Sjogren’s syndrome.
- Formation of the nodules.
- The serum complement level is usually normal except in patients with vasculitis.
- ANA (Antinuclear antibodies) are found in14% to 28% of RA patients.
Treatment
- This is simply symptomatic.
- The first line of defense is non-steroidal anti-inflammatory drugs. These drugs will control the symptoms by blocking cyclo-oxygenase and prostaglandin, prostacyclin, and thromboxane production.
- There are drugs, which modify the course of diseases like anti-malarial, D-penicillamine, and gold salt.
- Corticosteroids are used for symptomatic improvement, but their use is controversial.
- Cytotoxic drugs like azathioprine and cyclophosphamide may be used but avoided because of their side effects. Only useful in severe extra-articular manifestation.
Juvenile Rheumatoid Arthritis
This is the condtions of chronic synovitis starting during childhood.
The etiology and other hypotheses are like adult RA.
The etiology may be related to autoimmunity, infection, and trauma.
Signs and symptoms
- It is diagnosed before the age of 16 years. The swelling of the joint will be more than 6 weeks.
- Also, exclude all other condtions mimicking the Juvenile RA.
- 1/5th of the patients are suffering from Still’s disease. These patients are mostly HLA-DR5.
- Polyarthritis begins in 5 or more joints and is seen in 40% of the patients.
- There are two subgroups of this Juvenile RA:
- Girls younger than 6 years of age are ANA positive and have iridocyclitis. Iridocyclitis may lead to blindness.
- Boys are younger than 6 years of age with bilateral sacroiliitis. This subgroup is associated with HLA-B27.
- The rest of the 20% of patients meets the criteria laid by the American Rheumatism Association. The children in this group are HLA-DR4 positive.
- Diagnosis:
- The RA factor is positive in 1/5th of the patients. Rest children are negative (hidden RA factor).
- ANA is positive in very few patients.