Chapter 13: Hypersensitivity Reaction Type III, Immune Complex Disease
TYPE – III HYPERSENSITIVITY REACTION (IMMUNE COMPLEX DISEASE)
Definition
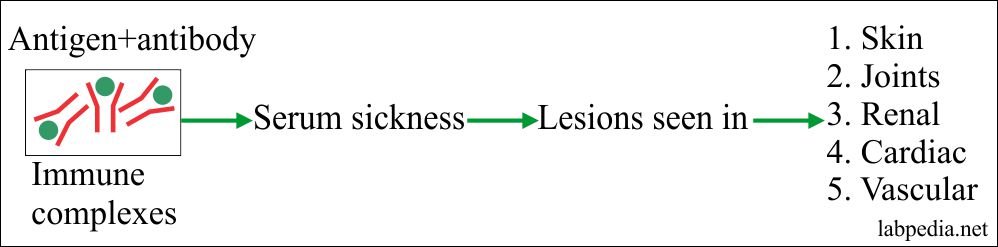
This was observed when foreign serum was injected into humans, there were a number of unpleasant side effects. This was called serum sickness and it resulted in cardiac, vascular, renal, cutaneous, and joints lesions.
When antibody meets antigen, give rise to immune complex formation. Mostly these immune complexes are removed by the mononuclear phagocytic system. But sometimes these Ag+Ab complexes persist and deposit in various tissues and organs. The complement and the effector cells mediated damage is called type III hypersensitivity reaction or immune complex disease. This Ag +Ab complex formation gives rise to acute inflammation.
The smaller complexes escape the phagocytosis and precipitate in:
- Blood vessels leading to vasculitis.
- Kidneys glomeruli leading to nephritis.
- Synovial membrane leading to synovitis.
The site of the deposit of immune complexes partly depends upon the site of antigen and partly how these complexes deposit in the tissue and various organs.
Immune complexes (Ag+Ab) deposits in the various organs:
| Source of the antigens | Etiology | Site of the immune complex deposition | Diseases caused by the immune complexes |
| Molds, plant, animal source | Inhalation | Respiratory system (lungs) |
|
| Self-antigens | Autoimmune diseases | Skin, joints, arteries, and kidneys |
|
| Bacterial infection | Persistent infection | Infected organs, and kidneys |
|
The information about the Type III or immune-complex disease came from the experiment on the rabbit, where it was found that the disease may be localized or systemic.
- The acute immune complex disease is systemin disease is called acute serum sickness. Immune complexes are still present in the blood circulation.
- The chronic immune complex disease where the repeated antigen is given to the same animal.
The experimental model of type III, immune complex disease:- Serum sickness can be shown by the injection of the foreign antigen which will mimic the effect of persistent infection.
- The Arthus reaction is an example of local damage by the extrinsic antigen.
- The NZB/NZW mouse shows autoimmunity.
Types of Antigens:
- Exogenous Antigens:-
- Drugs:-Sulphonamides, Penicillin, and Cephalosporin.
- Bacteria:-Treponema palladium and mycobacterium leprae.
- Protozoa:-Malaria (Plasmodium falciparum)
- Viruses:- HBV, EBV, and parasites.
- Foreign proteins.
2. Endogenous Ag: – These are auto Ag and give rise to autoimmune diseases.
Characteristics of Antigens:
The Antigens are small soluble and the body fails to clear off. Monocytes, neutrophils, and macrophagic cells easily remove larger (Ag & Ab) complexes while these are inefficient if the complexes are smaller in size.
The antibody in Immune complex disease are:
- Mainly IgG and IgM while IgA can give this reaction through an alternative pathway.
- IgG immune complexes are bound by the RBCs and gradually removed from the circulation.
- While IgA complexes bind poorly to RBCs but disappear rapidly from the circulation, with increased deposition in the kidney, lungs, and brain.
These Antibodies are divided by some researchers as:-
- Precipitating Ab which gives a local reaction.
- Non-precipitating Ab which gives systemic disease.
The dose and route of Agntigen also determine the pathology.
| Route | Resulting disease | Site of Ag + Ab complex deposition |
| Intravenous (High dose) | Vasculitis | Blood vessel walls |
| Nephritis | Renal glomeruli | |
| Arthritis | Joint spaces | |
| Subcutaneous | Arthus reaction | Perivascular area |
| Inhaled | Farmer’s lung | Alveolar /capillary interface |
Table XIX – Dose and Route of Antigen
The immune complex disease is a three stages phenomenon.
Stage A
Combination of Ag and Ab (complex formation, Ag+Ab).
The antigen may be inhaled, or there is persistent infection or autoantigen.
Stage B
Deposition of immune complexes.
The Antigen and Antibody complexes are small in size and are not phagocytosed, the process of phagocytosis will fail, and these will deposit or bound to the vessel wall.
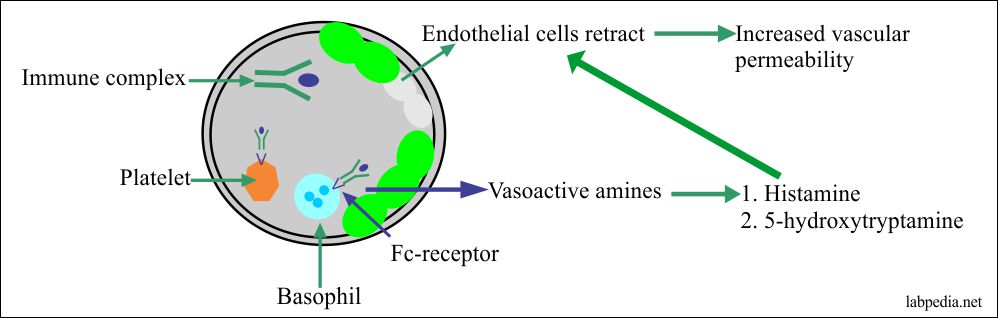
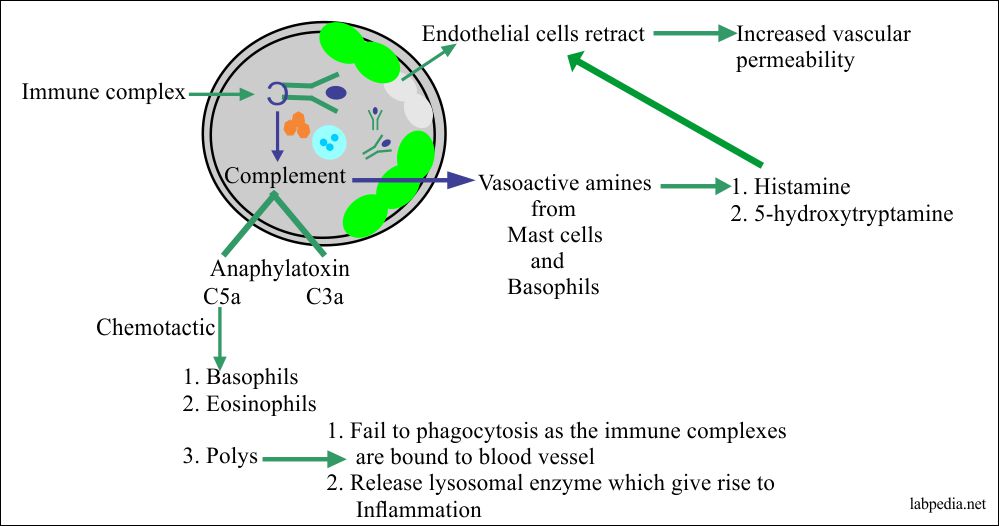
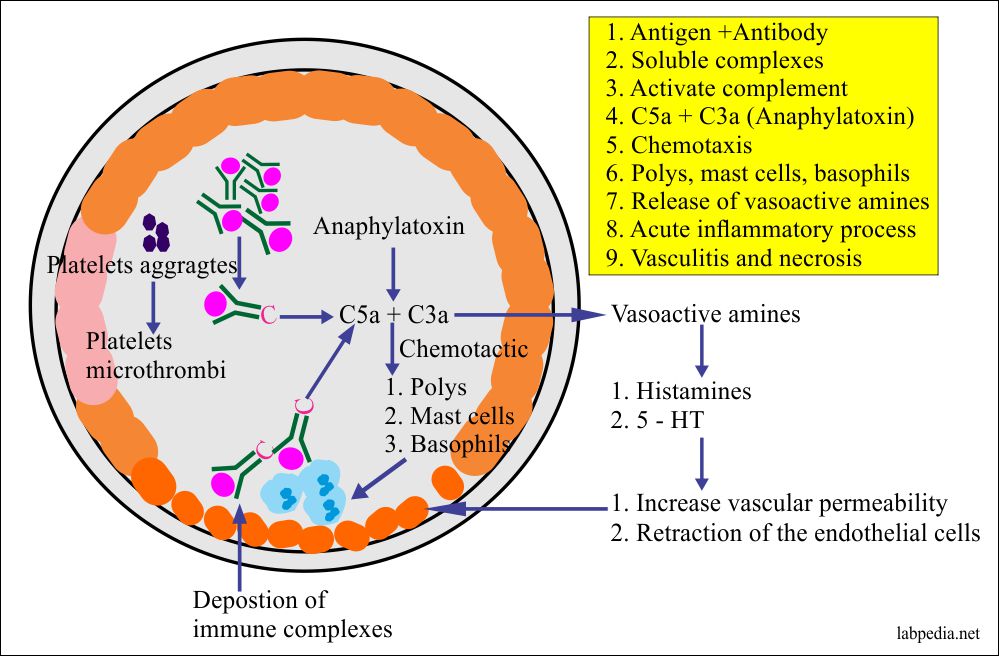
Vasoactive amines are released by the platelets, basophils, and mast cells cause endothelial cells retraction and thus increase vascular permeability, allowing the deposition of the immune complexes on the blood vessel wall. These deposited immune complexes keep on generating the C5a and C3a.
Stage C
Acute inflammatory response.
The cells bearing Fc-receptor for IgG and IgE are very important for the inflammatory process, with a complement that has a protective role.
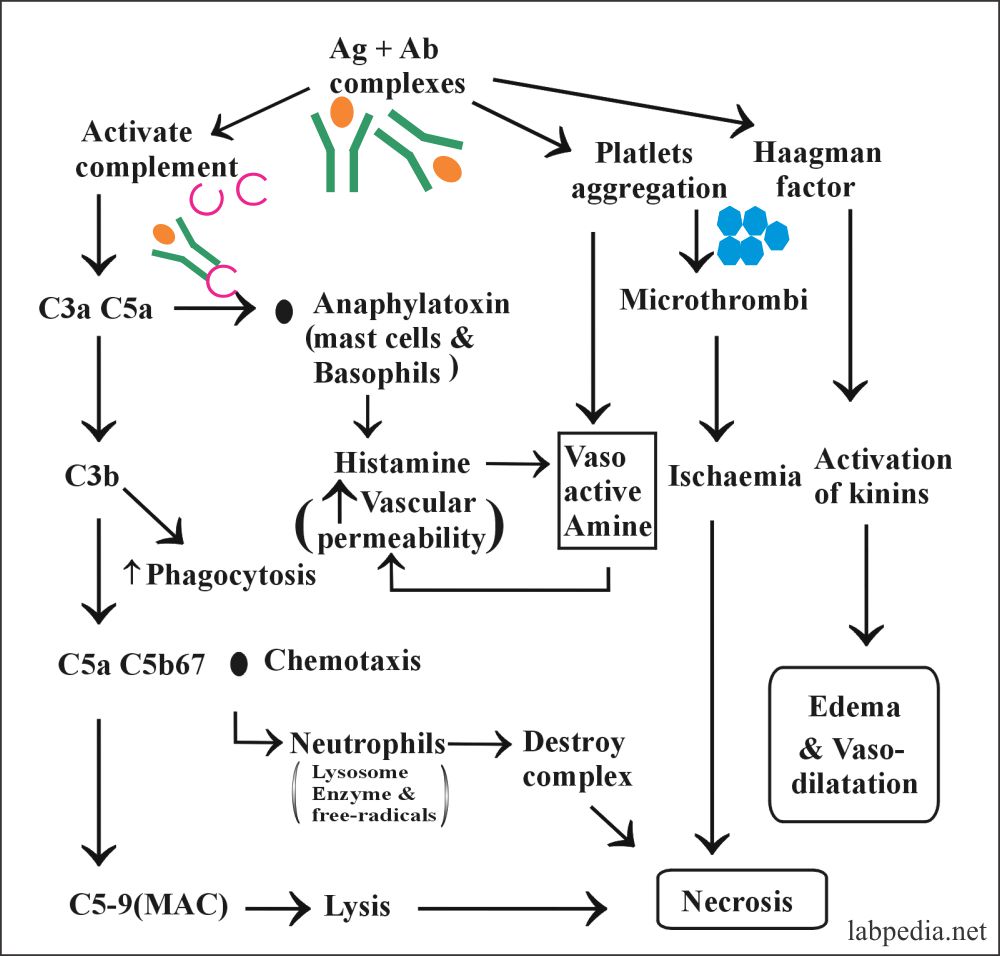
The immune complexes initiate a variety of inflammatory processes:
- Immune complex (Ag+Ab) interacts directly with basophils and platelets via Fc receptors and give rise to vasoactive amines.
- Macrphgic cells (Monocytes, polys) are stimulated to release cytokines, especially TNFα and IL-1, and these are very important in the process of inflammation.
- Immune complex (Ag+Ab) interact with the complement system to generate C5a and C3a, these are anaphylatoxin. These complements stimulate the release of vasoactive amines like histamine, 5-hydroxytryptamine, and also produce chemotactic factor from the mast cells and basophils. C5a is also chemotactic for the basophils, mast cells, and polys.
Deposition of Immune Complexes Depends Upon:
- Size of complexes.
- Mononuclear phagocytic status.
- Valency of antigen.
- The affinity of Ag to tissue.
- There is an initial miniature IgE reaction which leads to increased vascular permeability and helps in the deposition of immune complexes.
Deposition of Immune Complex:
In the immune-complex disease, the soluble complexes form in the soluble or fluid phase of the tissue or in the blood and develop unique biological functions such as interaction with complement and with cellular receptors.
Antigen + antibody (Ag+Ab) Complexes may deposit due to:
- Endothelial cells have phagocytic activity.
- There is increase adherence to endothelial cells.
- There may be trapping during filtration.
- Glomeruli and choroid plexus shows Fc receptor and C3b receptors.
Summary of Events in Type III
- Persistent Ag.
- B-L makes Ab.
- Ag + Ab complexes form and circulate.
- Ag + Ab complexes deposit in tissue.
- Complement activation, platelet aggregation, and Hageman factor activation takes
- C3a and C5a are produced.
- Mast cell degranulation due to C3a and C5a gives histamine and cytokines.
- Neutrophil chemotaxes.
- Vasculitis and fibrinoid necrosis.
- End-stage- acute inflammatory response with the presence of necrosis.
Ag and Ab complexes give an acute inflammatory response. The sequences of events are as follows:
The outcome of Deposition of Complexes:
| Site of deposition | Out of the reaction |
| Blood vessel | Vasculitis |
| Kidney | Glomerulonephritis |
| Joints | Arthritis |
Examples of immune-complex diseases:
| Causative agents | Disease caused by these agents |
| Heroin | Glomerulonephritis |
| Malarial parasitic infection | Glomerulonephritis |
| HBV infection | Polyarteritis nodosa |
| Tumor antigens | Glomerulonephritis |
| Autoimmune diseases |
|
| Infectious diseases |
|
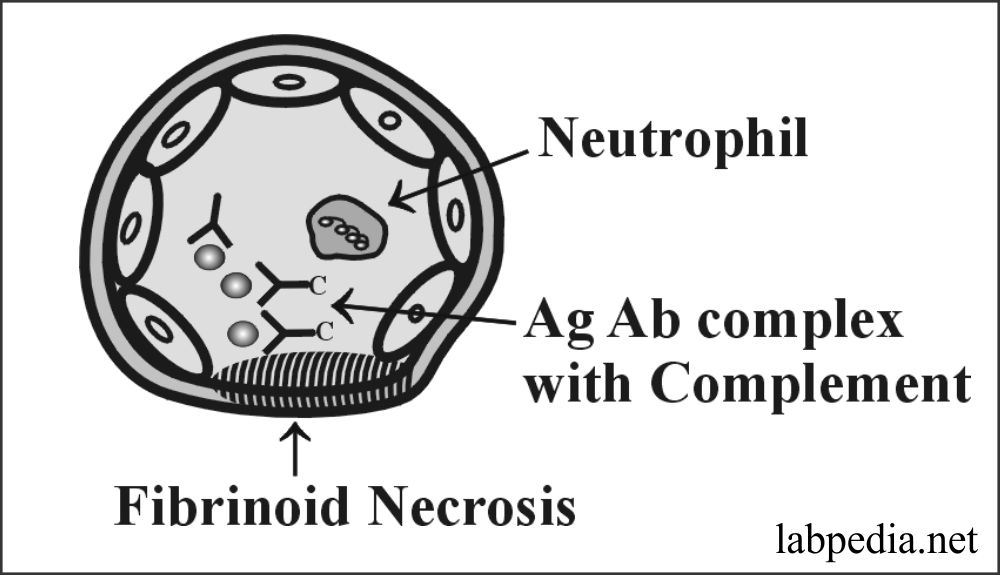
Microscopic Picture
There is an acute necrotizing vasculitis. There will be the presence of fibrinoid necrosis and neutrophil infiltration.
Within 12-24 hours there is the infiltration of neutrophils and later on replaced by macrophagic cells, which will degrade the complexes. There is an eosinophil infiltrate that produce histaminase enzyme. This enzyme histaminase will subside the inflammatory response and resolution takes place in a few days.
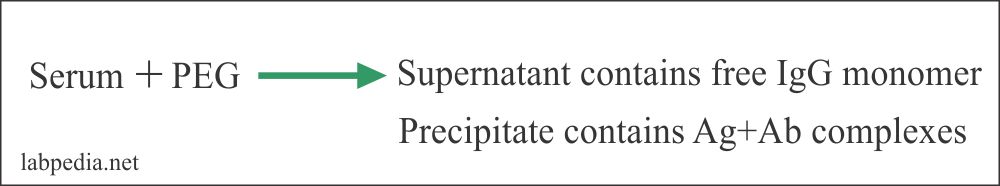
Detection of Immune Complexes:
- Detection of specific Ag is not possible.
- If Ag is a drug then it can be detected by its:-
- Physical character.
- The tendency to adhere to the cell membrane.
- Interact with some of the complements.
- The immunofluorescent technique can identify Immunoglobulin (Ig) and complement in the affected tissue. It shows deposits of Ig and Complement as lumpy or granular deposits.
- Antibody (Ab, Ig) can be precipitated by PEG (polyethylene glycol).
Precipitate (Ag + Ab) complexes can be detected by the following methods:-
- Add radio-labeled C1q and this will binds to (Ag + Ab) complex, then this may be read by Gamma counter (RIA).
- Add platelet and mix. There is a platelet aggregation.
- Ig in (Ag & Ab) complexes can be redissolved and estimated.
- Electron microscope. This will show electron-dense deposits along the basement membrane.
The immune complex disease may give rise to:
- Systemic disease.
- Localized disease.
Systemic Immune Complex Disease
In this case, complexes are too small and antigens may be smaller and soluble. Some believe that this situation arises when there is an excess of Ag. Which gives rise to circulating Ag + Ab complexes.
Examples
- The best example is serum sickness which was seen in World War II When soldiers were given 200 ml horse serum for diphtheria.
- Post streptococcal glomerulonephritis.
- Lepromatous leprosy.
- Secondary syphilis.
- Reaction to some drugs.
- SLE.
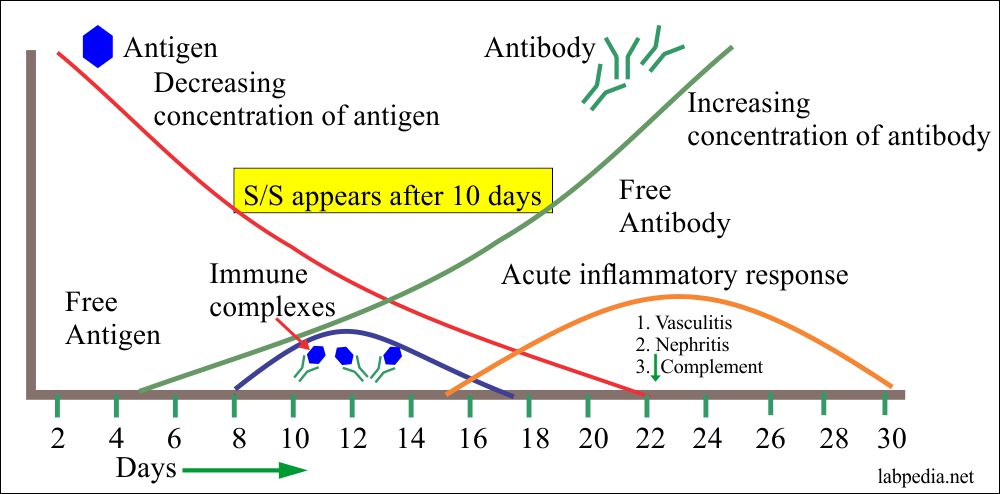
Serum Sickness
Serum Sickness needs to be discussing to get an idea about Immune-Complex disease.
Signs and symptoms appear 3 days to 3 weeks (average is 7-10 days) after exposure to Ag and patient will have:-
- Fever
- Urticaria and rashes.
- Generalized lymphadenopathy.
- Enlarged spleen.
- Arthritis.
- Proteinuria.
- Low complements level.
Affected organ Pathological lesion General signs and symptoms Malaise, weakness, and fever Lymph nodes Lymphadenopathy Joints Arthritis, and arthralgia Kidneys Glomerulonephritis Skin Urticaria, rash, and angioedema Blood vessels Vasculitis
Serum Sickness may be:
- Acute: It is seen in serum therapy due to the first exposure to an antigen.
- Chronic: When there is repeated exposure to Ag which gives rise to chronic disease and permanent damage.
- Examples are SLE, polyarthritis Nodosa, and membranous glomerulonephritis
Serum sickness can be induced by the large injection of the serum or foreign proteins. In this case, the circulating immune complexes deposit in the blood vessel wall, and tissue, leading to increased vascular permeability. Ultimately there is an inflammatory process in the form of glomerulonephritis and arthritis.
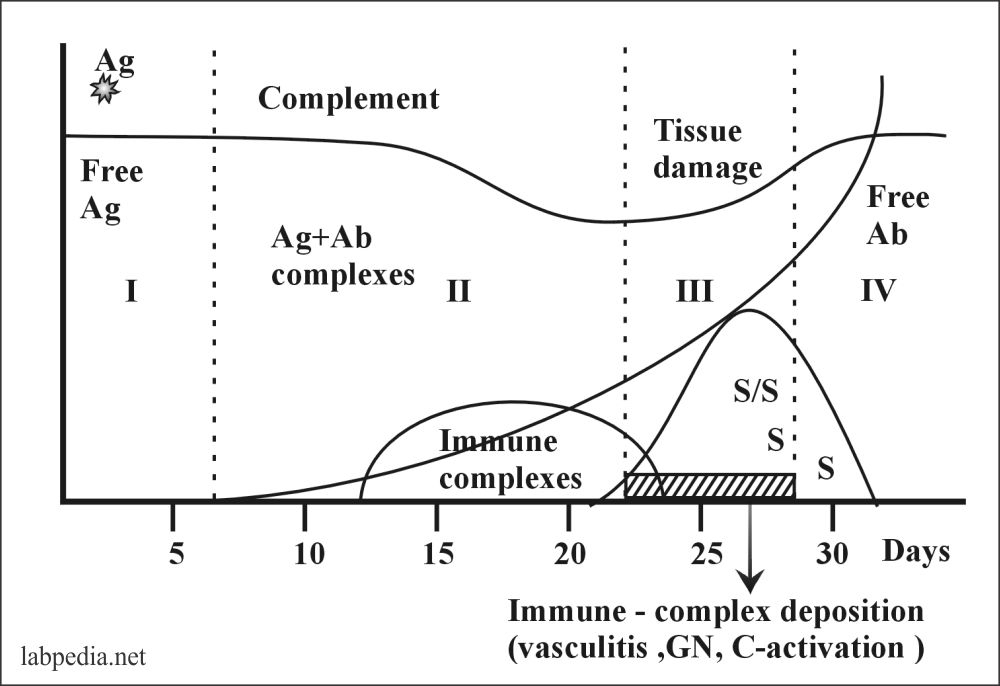
Serum Sickness takes place in four stages:
- Free Ag
- Ag+Ab complex formation and their deposition
- Because of Immune complex formation, S/S appears.
- No Ag is left and there is free Ab.
The above diagram shows that this is a self-limited disease. After the deposition of complexes, the patient develops S/S and ultimately there are no complexes and no Ag, so the patient starts recovering. If there is repeated Ag challenge patient will develop permanent damage to various tissues.
Local Arthus Reaction
Maurice Arthus described localized (Ag + Ab) immune complex disease in 1903. He did an experiment on Rabbit and injected Ag subcutaneously. The Rabbit was already immunized for that Ag. The following reactions were seen in the Rabbit.
1 to 2 hours = Local swelling erythema, pain, red, and hot.
4 to 8 hours =This is a peak period and there is vasculitis, which leads to hemorrhage, necrosis, and local ulcer.
12 to 48 hours = Neutrophils are replaced by mononuclear phagocytic cells. These will lead to phagocytosis of complexes and degrade these complexes. Later on, eosinophils appear, these cells produce antihistamines enzyme. The antihistamines enzyme will subside the inflammatory process.
The mechanism is just like a systemic disease.
Examples are:
- Rheumatoid arthritis = Antigen is IgG
- Farmer lung disease = Antigens are thermophilic actinomycetes.
- Pigeon fancier disease = Antigen is a protein in feces.
- Furrier lung disease = Antigen is Fox Furr protein.
- Repeated injection of insulin.
Antigens and antibodies complexes deposits and give rise to the acute inflammatory response.
Treatment
- Reduction of inflammation by means of aspirin, anti-histamine, and corticosteroids.
- Suppression of the immune response by corticosteroids and cytotoxic immunosuppressive drugs like cyclophosphamide and azathioprine.
- Removal of offending complexes by plasmapheresis.
The Hypersensitivity reactions and summary of their immunologic mechanism:Hypersensitivity reaction Type of reaction Time of development Type of Antibody Type of cells involved Role of complement Example of the disease Type 1 IgE dependent reaction Immediate IgE Mast cells No - Allergic rhinitis
- Anaphylactic reaction
- Drug sensitivity
Type II - Tissue-specific reaction
- Cytotoxic
- ADCC
Immediate IgG and IgM Macrophagic cells Frequently involved - Hemolytic disease of the newborn
- Grave’s disease
- ITP
- Autoimmune hemolytic anemia
Type III Immune-complex mediated reaction Immediate IgG and IgM Neutrophils Yes - SLE
Type IV Cell-mediated reaction Delayed None - Macrophages
- Lymphocytes
None - Chronic inflammatory diseases like TB
- Contact sensitivity to poison ivy and metals
Go Back to Elementary Immunology