Diarrhea:- Part 2 – Diarrhea Causative agents and Diagnosis
Diarrhea Causative Agents and Diagnosis
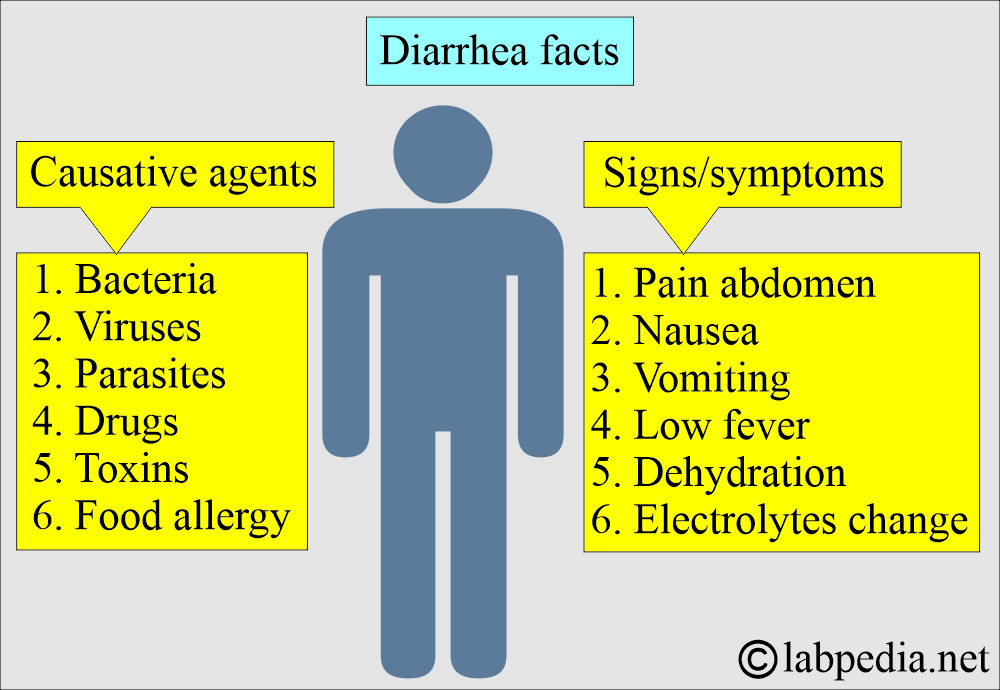
How will you define diarrhea?
- When there are loose motions, at least three per day.
- This may last for a few days and leads to:
- Dehydration.
- Decreased urination.
- Tachycardia.
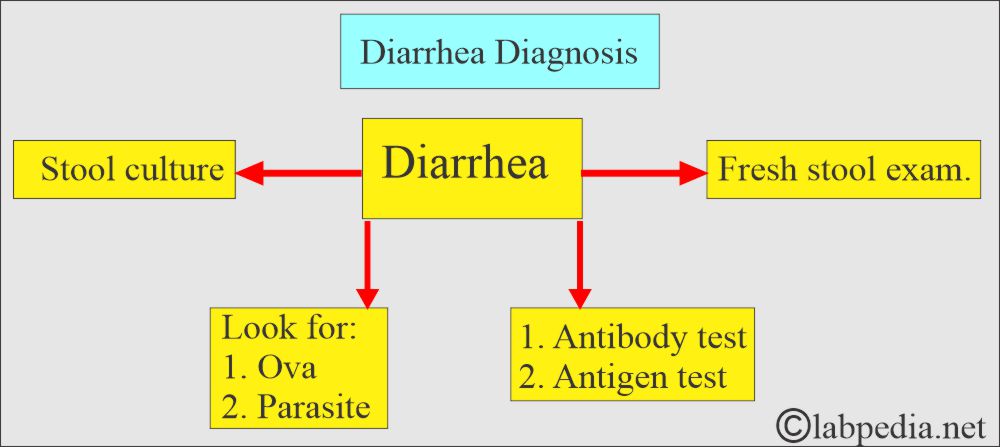
- A fresh stool sample is needed for the first culture, and then we can advise on additional tests.
- Fresh stool is required for ova and parasite detection.
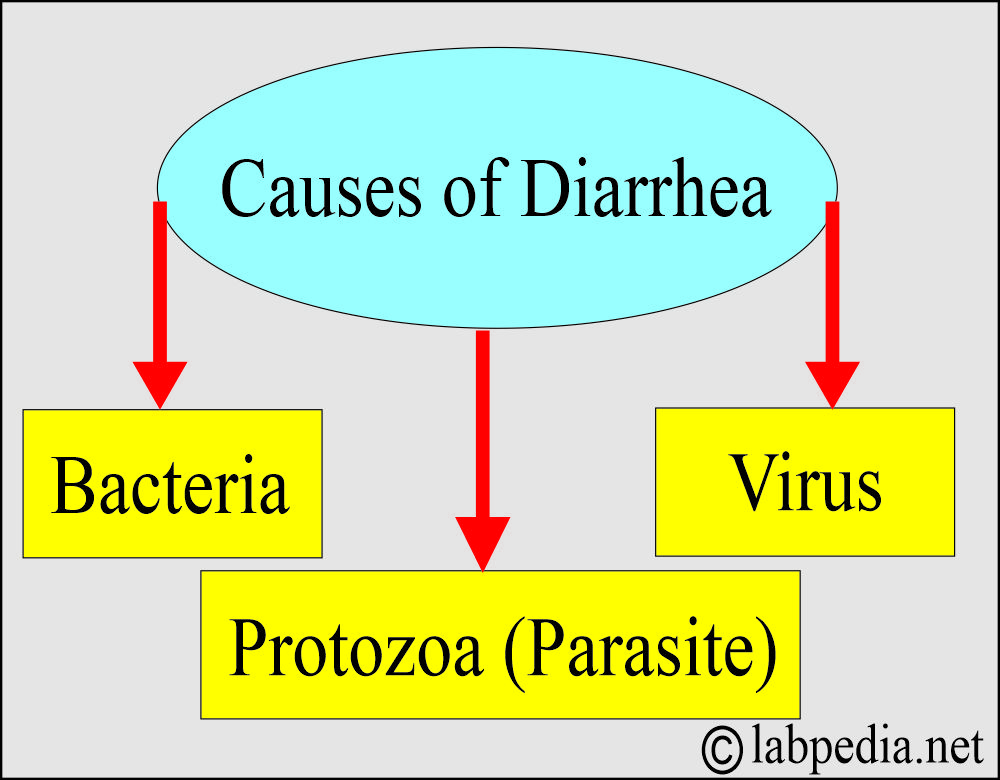
What microorganisms cause diarrhea?
- Viruses.
- Bacteria.
- Parasites.
What are the types of Diarrhea?
- Watery diarrhea.
- Bloody diarrhea.
- Another classification is:
- Acute diarrhea.
- Exudative diarrhea (There is inflammation of the intestinal mucosa).
- Chronic diarrhea.
- This diarrhea has been present for at least 4 weeks. This may be even longer, ranging from 6 to 8 weeks.
- Osmotic diarrhea (malabsorption).
- Secretory diarrhea (Due to abnormal electrolyte transport).
- Due to intestinal motility disturbances.
What are the causes of Acute infectious diarrhea?
| Traveler’s diarrhea (community-acquired diarrhea) | Persistent diarrhea = >7 days | After hospitalization = >3 days | Immunocompromised patients due to HIV |
|
|
|
|
What are the causes of Watery Diarrhoea?
- Bacteria, such as Escherichia coli, and others produce enterotoxin.
- Usually seen in travelers.
- Protozoa, Giardia lamblia, and others.
- This may be seen in travelers and contaminated water supply.
- In a child care center, this may be a chronic problem.
- Pre-formed enterotoxin by Staphylococcus aureus, Bacillus cereus, and Clostridium perfringens.
- This is due to food poisoning.
What are the causes of Bloody Diarrhoea or dysentery?
- Shigella and Salmonella.
- Campylobacter.
- Entamoeba histolytica.
- This may be common for travelers.
What are the common causes of diarrhea?
- Shigella.
- Salmonella.
- Esch. Coli.
- Staph. Aureus.
- Campylobacter.
- Cl.perfringens.
- V.cholerae.
Shigella
- Shigella causes bacillary dysentery.
- This is a worldwide problem and fatal in young children, especially in the third world.
- Shigella is a worldwide problem and an important cause of death in young children, especially in the third world.
- Shigella is of four types:
- Sh. dysenteriae (also known as Shigella Shiga). It has 13 serotypes.
- Sh. boydii. It has 18 serotypes.
- Sh. sonnei. It has only one serotype.
- Sh. flexneri. It has six serotypes.
- Epidemiology:
- The incubation period is 1 to 9 days.
- After an acute attack, the patient may continue to excrete the bacteria in their stool for several weeks or months.
- Patients during the acute stage are the primary source of spread because many bacteria are passed in the stool.
- The route of entry is the feco-oral, either direct spread or contaminated utensils, towels, and toilet seats.
- Shigella can remain viable for an extended period in a cool and moist environment.
- Contaminated water is a primary source of infection; other sources include flies, fomites, and contaminated food.
- The stool has blood and mucus.
- There may be pus in the stool.
How will you define Shigella dysentery?
- It is due to Sh. dysenteriae is severe and life-threatening and is seen in tropical countries.
- There is a fever and abdominal pain.
- There is diarrhea.
- This produces a potent neurotoxin.
- It also produces enterotoxin and cytotoxin.
- This is an invasive disease.
- This is a severe, life-threatening disease and is found in tropical countries.
- Sometimes, this may produce septicemia.
- While dysentery from other species is mild.
What are the signs and symptoms of Shigella groups?
- There is diarrhea with blood and mucus.
- Sometimes, may find pus.
- There may be a severe life-threatening disease or a mild or symptomless infection.
What do you know about Shigella sonnei?
- It is a common cause of dysentery in the UK. It may be seen throughout the world.
- It is common in young children.
- Its outbreaks are common in the nursery school.
- There are reports in the mental hospital that infection may be difficult to eradicate.
- Mostly, the disease is mild, and in a few cases, dehydration may occur, requiring emergency treatment.
What do you know about Shigella flexneri?
- It was also common in the UK.
- It was the common cause of dysentery in Glasgow.
- It is no longer seen in the UK.
- It is also seen in tropical countries.
What do you know about Shigella boydii?
- It is common in the Middle and Far East.
How will you diagnose Shigella dysentery?
- It can be diagnosed with a stool or rectal culture.
- Culture is performed on selective media, such as MacConkey, deoxycholate citrate agar, and XLD agar.
- There are pale, non-lactose-fermenting colonies.
- Shigella sonnei is a late fermenter of lactose.
- Do biochemical tests for identification.
- Serological identification can be made using specific antisera or polyvalent antisera.
How will you treat Shigella dysentery?
- Antibiotics are usually not needed.
- In a few cases, you may use Trimethoprim (the first line of treatment).
- Antibiotics may be needed for Shigella sonnei.
- In severe cases, systemic antibiotics are used.
How will you prevent Shigella infection?
- Shigella infection may be prevented by:
-
- This depends primarily on sanitation, access to safe water, and adequate sewage disposal.
- It isn’t easy to control in a nursery school.
Escherichia Coli
- This is common normal commensal gut flora.
- However, some of the strains lead to diarrhea.
- The E. coli 0157:H7 strain produces toxins that cause damage to the small intestinal lining.
- How will E. Coli spread?
- Coughing.
- Kissing.
- Every day, engage in social interactions with friends and family.
- It can spread through contaminated water. Then it spreads through the feco-oral route.
- It spreads through raw or uncooked ground meat, raw milk, and cheese.
- It also spreads through contaminated vegetables.
What is the presentation of E. Coli diarrhea?
- It starts with stomach pain and cramps.
- There is a loss of appetite and nausea.
- It is followed by vomiting.
- The patient may have a low fever of <101 °F. But this is not a standard feature.
- There may be watery diarrhea.
- Watery diarrhea may last for one day and then change into bloody diarrhea.
- This bloody diarrhea may last for 2 to 5 days.
- There may be 10 or more bowel movements per day.
- Most people recover without any treatment.
Hemorrhagic colitis and hemolytic uremic syndrome
How will you define hemorrhagic colitis and hemolytic syndrome?
- There may be a life-threatening syndrome with a bleeding tendency.
- This may be due to toxins that are cytopathic.
- Hemorrhagic colitis has been observed in both children and adults as a sporadic infection.
- There may be death in older patients.
- Hemolytic uremic syndrome is seen in children as an outbreak or sporadic case.
- This is usually seen with a serotype of 0157.
- There is diarrhea followed by uremia.
- There is thrombocytopenia.
- There is hemolytic anemia.
Traveler diarrhea (Turista)
How will you define traveler’s diarrhea?
- This has different names, like:
- Montezuma’s revenge.
- Delhi belly.
- Tokyo two-step.
- The serotype of traveler diarrhea:
- The strains of Escherichia cause this diarrhea, where E. coli produces enterotoxins, and the common ones are enterotoxigenic O6 and O78.
- This can spread through contaminated foods and drinks.
- There is diarrhea and abdominal pain.
- There may be vomiting.
- This is usually a self-limiting disease.
- Damage is due to heat-labile or heat-resistant toxins.
Infantile gastroenteritis
How will you define infantile gastroenteritis?
- Serotypes:
- These are caused by Esch. Coli by the enteropathogenic strains, serogroups 055 and 0111, and sometimes by enterotoxigenic strains, serogroups 06 and 078.
- The incubation period is 1 to 3 days.
- It is usually seen in babies under the age of 2 years.
What is the epidemiology of infantile gastroenteritis?
- There are sporadic cases in the community.
- This infection is common in the third world due to poor sanitation and hygiene.
- In the third world, the major cause of mortality is due to this disease. Flies may be the main reason.
- In nurseries and neonatal units, the infection spreads by direct contact, staff, or handling.
What is the pathogenesis of infantile gastroenteritis?
- The number of strains that produce enterotoxins and others produce Vero cytotoxin.
- Some of these bacteria attach to the epithelium, a crucial pathogenic mechanism.
What are the signs and symptoms of infantile gastroenteritis?
- There is acute diarrhea, which may lead to dehydration.
- There is an acid-base disturbance.
- There is hypernatremia (increased sodium).
- Culture from feces can be diagnosed.
How will you diagnose infantile gastroenteritis?
- Take a stool as a sample for culture.
- The stool is cultured on MacConkey media.
- There are pink-colored colonies (lactose-fermenting).
- Identified by the polyvalent sera.
How will you treat infantile gastroenteritis?
- Rehydration is needed to correct the acid-base imbalance.
- In severe cases, antibiotics may work. Otherwise, their use is doubtful.
How will you prevent infantile gastroenteritis?
- Strict hygiene measures are essential in neonatal units and nurseries.
- Examine all new cases for admission for these enteropathogenic strains.
- Isolate all positive cases.
- Check all the staff members for this infection.
- It can be controlled by providing access to clean water and promoting good hygiene.
Salmonella food poisoning
How will you define Salmonella food poisoning?
- Salmonella diarrhea is often referred to as food poisoning, but this term is misleading.
- S. enteritidis phage type 4 was common in the UK in 1980 and was the most common cause of incidents in poultry flocks.
- S. typhi, paratyphi A, B, and C mainly cause enteric fever, and in the late stages, these patients develop diarrhea.
- S.paratyphi causes enteric fever and diarrhea.
- The incubation period is typically short, ranging from 12 to 36 hours.
What is the mode of spread of Salmonella food poisoning?
- Food derived from domestic animals and poultry is the primary source.
- When these meats are not properly cooked and stored at room temperature, they can cause foodborne illness.
- The eggs may also be the source.
- Another source may be contaminated milk and sometimes cheese.
- Human carriers may also play a role in the spread.
What are the signs and symptoms of Salmonella food poisoning?
- Early symptoms are abdominal pain and diarrhea.
- There may be fever and vomiting.
- The patient may get dehydrated.
- In severe cases, septicemia may be seen.
How will you diagnose Salmonella food poisoning?
- For diagnosis, do a culture of the feces on MacConkey and selective media.
- The biochemical test on the culture material can confirm it.
How will you treat the Salmonella food poisoning?
- Treatment with antibiotics is contraindicated except in cases of septicemia.
- Rehydration is necessary.
Campylobacter
How will you define Campylobacter infection?
- This is recognized as a major source of diarrhea.
- Campylobacter is a small vibrio-like organism.
- These are curved gram-negative bacilli.
- These have characteristic darting motility.
- These are oxidase reactions positive.
- The main cause of human infection is C. jejuni.
- Rarely caused by C. jejuni subspecies such as doylei, C. coli, and C.lari.
- The incubation period is 3 to 10 days.
What are the sources of Campylobacter?
- The main source of infection is poultry.
- Other sources are milk and water.
- Dogs and cats are also reported as the source.
- The mode of spread is the fecal-oral route, which occurs when contaminated food is eaten.
What are the signs and symptoms of Campylobacter?
- The main symptoms of Campylobacter are:
- Fever.
- A headache.
- A backache.
- Limb pain.
- Abdominal pain. This is a prominent feature of Campylobacter infection.
- After 24 hours or later, the patient develops diarrhea.
- Diarrhea sometimes is severe with mucus and blood.
- There may be up to 20 stools per day.
- In severe cases, you may see septicemia.
- Typically, there is enterocolitis, which involves the small intestine, the ileum.
- In some cases, there may be colitis.
How will you diagnose Campylobacter?
- Advise the stool culture on the selective media containing antibiotics at 43 °C.
How will you treat Campylobacter?
- Treatment: It is usually self-limiting.
- Erythromycin can reduce the duration of the disease, but should be reserved for severe cases.
- Another drug is ciprofloxacin.
Cholera
How will you define Cholera?
- This is caused by Vibrio cholerae.
- The causative agent is V.cholerae 01.
- In Bengal, the epidemic was due to type 139.
What is the source and transmission of Cholera?
- The incubation period ranges from 6 hours to 5 days, typically due to sewage water contamination.
- Sometimes, this may occur due to food contamination.
- Flies contaminate food.
- It can exist freely in the water.
- The spread is feco-oral. Human GIT is the reservoir.
- Symptomless carriers are common in epidemics.
What are the signs and symptoms of Cholera?
- The patient develops abdominal pain and diarrhea.
- Watery diarrhea like rice water.
- There may be mucous.
- The patient may have vomiting and dehydration.
- There is acidosis, and the patient may collapse.
- Cholera is seen in two forms:
- Classical cholera (severe).
- A mild form of cholera is associated with the El Tor biotype.
What is the pathogenesis of Cholera?
- Exotoxin: V. cholerae produces a potent protein exotoxin.
- Endotoxin: This is a lipopolysaccharide.
How will you diagnose Cholera?
- This can be diagnosed by:
- The culture of feces on selective media.
- There are typical colonies.
- This can be identified by slide agglutination with polyvalent antisera.
- Antigen capture test.
- Latex agglutination test.
How will you treat Cholera?
- This is treated by replacing the fluids.
- When tetracycline is given, the disease course may be short.
Staphylococcus aureus
How will you define Streptococcus aureus diarrhea?
- This is due to toxic food poisoning.
- This is due to enterotoxin contamination of the foods by Staph. Aureus.
- This is very rapid in onset due to the preformed toxin in the food.
What is the pathogenesis of Streptococcus aureus diarrhea?
- Staphylococcus produces about 40% of the five antigenically different types of enterotoxins.
- These are named Enterotoxin A, B, C, D, and E.
- The preformed toxins present in the contaminated foods have local action on the gut mucosa.
- Toxins are resistant to high temperatures, which will kill the bacteria.
- So, food contains toxins and no viable bacteria.
What are the signs and symptoms of Streptococcus aureus?
- Symptoms due to Staphylococcus aureus are:
- Acute onset of nausea and vomiting.
- This may be followed by diarrhea.
- This is a self-limiting disease.
How will you diagnose Streptococcus aureus diarrhea/dysentery?
- Diagnosis of diarrhea due to Staphylococcus aureus:
- Check the suspect’s food, vomit, or feces.
- Culture on ordinary media or mannitol salt agar.
- Perform a coagulase test.
- Also, it can do phage typing.
Clostridium perfringens (Cl. perfringens)
How will you define Clostridium perfronges infection?
- This is fairly common and is due to the contamination of foods by Cl. perferingens.
- Clostridium perfringens is a spore-bearing, heat-resistant, and anaerobic organism.
- These are non-hemolytic strains.
- This bacterium can resist heat at 100 °C for 30 minutes.
- During cooking, spores germinate into vegetative form.
- If food is kept at room temperature, then these bacteria rapidly multiply.
- After ingesting the vegetative form, sporulation occurs in the small intestine, resulting in the release of enterotoxins.
- These toxins primarily affect the permeability of the small intestine’s membrane.
- Cl. perfringens may be present as commensals in the intestines of humans and animals.
- The incubation period is 8 to 24 hours after eating the contaminated food.
What are the signs and symptoms due to Clastridium perfronges infection?
- Abdominal pain.
- Diarrhea.
- Rarely, there may be vomiting.
- This is a self-limiting disease.
How will you diagnose Clastridium perfronges infection?
- Take a sample of the feces and suspected food.
- Culture the sample on blood agar under anaerobic conditions.
- Colonies are typically β-hemolytic or non-hemolytic.
- The Nagler reaction can identify it.
- Can do serotyping by slide agglutination.
- Can detect enterotoxin in the stool by ELIZA.
How will you treat Clastridium perfronges infection?
- Treatment is symptomatic by rehydration.
- Antibiotic therapy is not needed.
What are the common Signs and Symptoms of various types of diarrhea?
- Watery diarrhea may be seen in travelers due to contaminated water and food-related poisoning.
- Bloody diarrhea may also be seen in travelers.
- There may be fever and abdominal cramps.
- Sometimes, there may be vomiting.
How will you diagnose Diarrhea?
- Stool examination:
- Children and infants can get rectal swabs.
- Stool examination for the presence of WBCs and RBCs.
- Fresh stool for ova and parasites.
- Suspected food sample:
- Try your best to get a suspected food sample. Because sometimes it is discarded or eaten.
- Vomitus can be used.
- A blood culture:
- This may be necessary in severe cases, especially in very young and elderly individuals.
- Serology:
- There is a Giardia lamblia rapid antigen detection test.
- E. Histolytica can be seen by microscopy or antigen detection.
- The serum antibody test for an amoebic liver abscess.
- In outbreak areas;
- Take the sample from the kitchen area.
- Take the fecal samples from the food handlers (kitchen workers).
What is the Prevention of Diarrheal Disease?
- It depends mainly upon sanitation.
- Adequate disposal of sewage.
- Supply clean foods.
- Try your best to get a safe water supply.
- Advise good personal hygiene.
- Washing of the hands after defecation should be mandatory; wash hands at least three times.
- The above measures will prevent the feco-oral spread of diarrheal diseases.
Diarrhea causes and diagnosis:
| Causative agent | Source | A common source of infection | Diagnosis |
| Salmonella species | Animals and humans | Milk, eggs, meat, and poultry | The specimen is feces, cultured on selective media. |
| Shigella species | Humans | Food, fomites, and the feco-oral route | Stool and rectal swab on MacConkey and selective media |
| Escherichia coli | Humans | Food, water, fomites, and the feco-oral route | Feces culture on MacConkey medium |
| Bacillus species | Soil | Rice | Suspected food, vomitus, and stool culture on ordinary media |
| Staphylococcus aureus | Septic lesion on food handlers | Dairy products and cooked meat | Suspected food, vomitus, or feces are cultures on ordinary media |
| Campylobacter species | Animals | Meat, milk, and poultry | Feces culture on selective medium |
| Clostridium perfringens | Animal | Meat pies and stews | Feces and suspected food on aminoglycoside blood agar anaerobically |
| Clostridium difficle | Humans | Feco-oral and overgrowth of strains in the colon | Direct detection of toxins and isolation on selective media |
| Vibrio cholerae | Humans | Food and water | Feces on selective medium (TCBS agar). |
| Yersinia species | Animal | Food and water | Isolation from feces or blood or rising antibody titer |
Questions and answers:
Question 1: How will you diagnose diarrhea?
Question 2: What are the causes of infantile gastroenteritis?
Question 2: What is Delhi bellies?

Awesome,thank you a lot
Thanks.