Diabetes Mellitus:- Part 6 – Complications of Diabetes Mellitus and Prevention
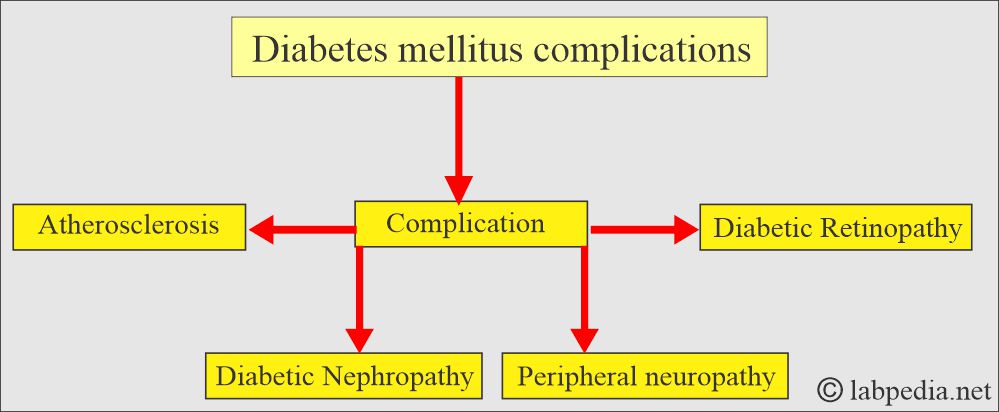
Complications of Diabetes Mellitus
- Diabetic patients need follow-up and proper control to prevent diabetic complications.
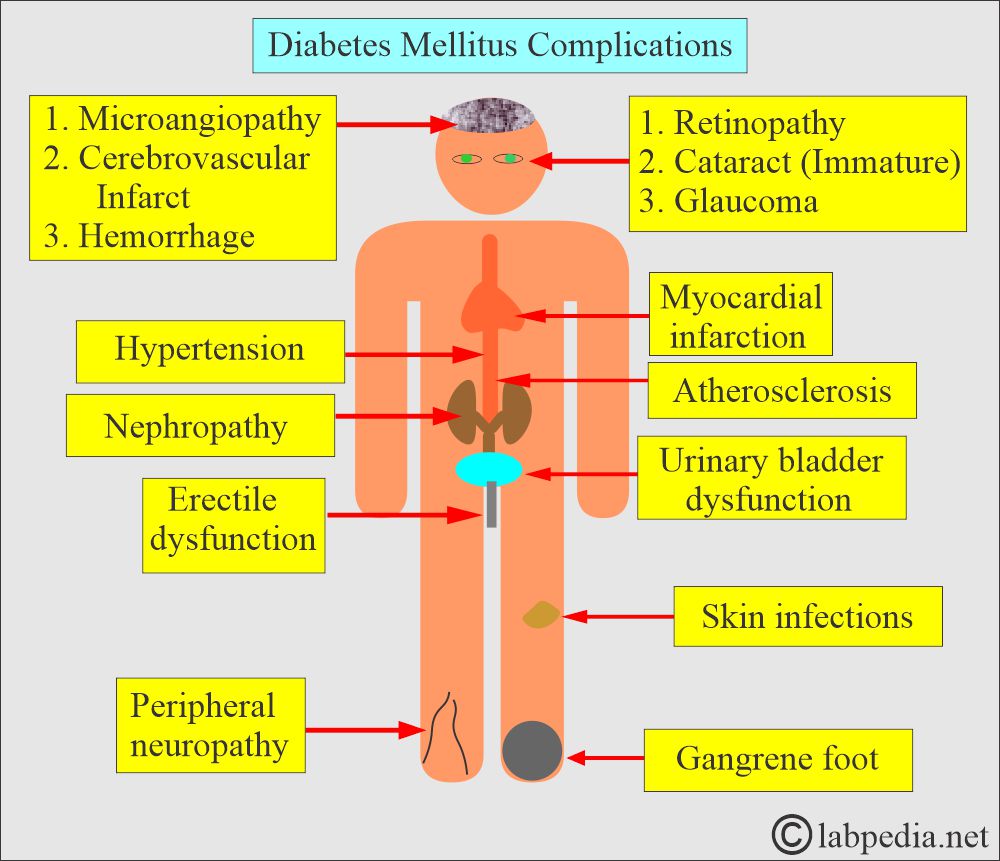
What are the complications due to diabetes mellitus?
- Infections caused by staphylococci.
- History of impotence.
- A history of polyneuropathy, which will present as tingling and numbness in the feet.
- Arterial disease results in acute myocardial infarction or gangrene of the foot.
- There is retinopathy, which is detected during an examination by an eye specialist.
What will be the presentation of the complications due to Diabetes Mellitus?
- There may be hypoglycemia.
- Patients with hyperglycemia of Type I, left uncontrolled, may develop life-threatening complications like diabetic Ketoacidosis.
- Without treatment, the patient may become acidotic and dehydrated and lose consciousness.
- Type II may develop hyperosmolar coma.
- Peripheral neuropathy.
- Diabetic retinopathy and cataract formation may lead to blindness.
- Cardiovascular microangiopathy:
- Coronary atherosclerosis.
- Myocardial infarction is 3 to 5 times more common in diabetic patients.
- AMI is the leading cause of death in diabetes mellitus type 2.
- Peripheral vascular diseases like ischemia of the lower extremities, erectile dysfunction, and intestinal ischemia.
- Gangrene of the foot.
- Diabetic kidney diseases, diabetic nephropathy.
- It may lead to renal failure.
- Chronic pyogenic skin infection.
- Candidal infection of the skin.
- The bones and joints show contracture.
- In the end, it may result in stroke, gangrene, and coronary artery disease.
- These patients may have gum and mouth diseases.
How will you categorize the complications of diabetes mellitus?
What are the Acute complications?
Hypoglycemia:
- In the case of excess insulin injection and excess intake of alcohol, especially with an empty stomach, it can lead to hypoglycemia.
- Increased hypoglycemia risk includes autonomic neuropathy, gastroparesis, and end-stage chronic kidney disease.
- Hypoglycemia occurs in impaired glucagon response, sympathoadrenal responses, and cortical deficiency.
- Hypoglycemia can be classified as:
- Reactive, seen after eating.
- Fasting hypoglycemia is seen due to organic diseases like the liver, kidneys, pancreas, and a deficiency of hormones.
- Combined, including reactive and fasting hypoglycemia.
Hyperglycemia:
- Patients with uncontrolled hyperglycemia of Type I diabetes mellitus may develop life-threatening complications like diabetic Ketoacidosis.
- Without treatment, the patient may become acidotic and dehydrated and lose consciousness.
- Type 2 diabetes mellitus may develop hyperosmolar coma.
- Hyperglycemia may be seen in:
- Diabetic ketoacidosis.
- Lactic acidosis.
- Alcoholic ketoacidosis.
- Hyperosmolar coma.
What are the Chronic complications?
- These lead to hypertension, end-stage chronic renal diseases, Blindness, autonomic and peripheral neuropathy, amputation of the lower limbs, myocardial infarction, and cerebrovascular accidents.
- Diabetic neuropathy:
- The most common is diabetic peripheral neuropathy, where the loss of function appears in a stocking-glove pattern and is due to an axonal neuropathic process.
- Foot motor and sensory nerve conduction are delayed in the peripheral nerves, and the ankle jerk may be absent.
- Isolated peripheral neuropathy involves the distribution of a single nerve. This is attributed to vascular ischemia or traumatic damage. Cranial and femoral nerves are more commonly involved.
- Autonomic neuropathy is seen in advanced and long-standing diabetes mellitus. This may involve visceral blood pressure, pulse, gastrointestinal activity, urinary bladder function, and erectile function.
- Peripheral neuropathy. There is the involvement of the cranial and peripheral nerves.
- Ocular complications:
- Premature cataracts occur in diabetics.
- There are two types of retinopathy:
- One is called nonproliferative retinopathy.
- The second is called proliferative retinopathy.
- Glaucoma occurs in 6% of diabetics.
- Vascular pathology:
- The involvement of small and large blood vessels.
- Cardiovascular microangiopathy may explain the etiology of congestive cardiomyopathy in people with diabetes who don’t have evident coronary artery disease.
- Coronary atherosclerosis gives 3 to 5 times more myocardial infection in diabetics and is the leading cause of death in type 2 diabetes mellitus.
- Type 1 diabetes mellitus has also increased the risk of coronary artery disease. It is lower than type 2 DM.
- AMI is the leading cause of death in diabetes mellitus type 2.
- Peripheral vascular diseases like ischemia of the lower extremities, erectile dysfunction, and intestinal ischemia.
- Gangrene of the foot.
- Diabetic nephropathy:
- 30% to 40% of type 1 diabetes Mellitus patients develop nephropathy over 20 years of diabetes.
- In type 2 diabetes, nephropathy is less common. Only 15% to 20% develop renal disease.
- Diabetic kidney disease (diabetic nephropathy) may lead to end-stage renal disease.
- Initially, there is proteinuria, followed by a decline in renal function, which leads to an increase in blood urea and creatinine.
- This renal disease can be assessed by microalbuminuria.
- Also, advise the albumin/creatinine ratio.
- The albumin/creatinine ratio <30 is normal.
- The ratio of 30 to 300 mcg/mg suggests the presence of abnormal microalbuminuria.
- Chronic renal disease is suspected when persistent albumin is excreted in more than 30 mcg/mg creatinine.
- Patients develop nephrotic syndrome with hypoalbuminemia, edema, increased LDL-cholesterol, and increased azotemia when inadequate treatment is used.
- Ultimately, there is end-stage renal disease.
- Chronic pyogenic skin infection:
- Candidal infection of the skin.
- Also, there is vulvovaginitis in a female with uncontrolled diabetes mellitus.
- In type 2 DM, poorly controlled diabetics have eruptive cutaneous xanthomas.
- The bones and joints show contracture.
- In chronic and long-standing diabetics, the hand’s progressive stiffness is secondary to the contracture and tightening of the skin over the joints (diabetic cheiroarthropathy).
- There may be frozen shoulders, also known as adhesive capsulitis.
- There may be carpal tunnel syndrome and Dupuytren’s contracture.
- There may be hyperuricemia, and tophaceous gout is more common in individuals with type 2 diabetes.
Can you summarize the Acute and chronic complications of diabetes mellitus?
| Acute complications | Chronic complications |
|
Vascular diseases
Nonvascular diseases
|
How will you prevent complications of Diabetes mellitus?
- Diet plan:
- It is better to take salad before your dinner and lunch. It can prevent spikes in glucose (based on personal experience).
- Try to decrease the carbohydrates. Wheat, in any form, provides a glucose spike.
- Try to eat a high-fiber diet, including vegetables, whole grains, and legumes.
- Try to keep the timings between two meals at least 3 to 4 hours. In between, do not eat anything except water.
- Regular exercise:
- It is recommended that you engage in brisk walking for at least 150 minutes per week. It means you need 22 22-minute brisk walks daily.
- Additionally, you can incorporate exercise into your daily routine.
- Blood pressure:
- Try to keep your blood pressure between <130/80 mmHg.
- Advise basic metabolic panel:
- Fasting glucose level.
- Try to keep it between 80 to 130 mg/dL.
- Postprandial glucose level.
- Try to keep your blood sugar level below 180 mg/dL.
- Microalbuminuria.
- BUN (urea).
- Creatinine.
- Electrolytes.
- Anion gap = (Sodium + potassium) — (Chloride + bicarbonate)
- HbA1c.
- Try to keep it <7%.
- Fasting glucose level.
- Lipid profile for cardiovascular system:
- Cholesterol.
- Triglycerides.
- HDL.
- LDL.
- Try to keep it <100 mg/dL.
- In high-risk patients, try to keep LDL <70 mg/dL.
- Check the urine of all diabetic patients regularly for microalbuminuria. The presence of proteinuria is the first sign of nephropathy.
- This can be slowed by antihypertensive therapy in case of hypertension.
- A renal biopsy may be done to evaluate kidney histology.
- Eye check-up:
- It is done to detect retinopathy.
How will you summarize the prevention of diabetic patients?
| Organs to be checked. | Preventive test | Organs involved (Disease) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Questions and answers:
Question 1: What is the reason for gangrene of the foot in diabetics?
Question 2: How can you find the involvement of the kidney in diabetics?