Diabetes Mellitus:- Part 1 – Carbohydrate (CHO) and Glucose Metabolism, Insulin and Glucagon
Carbohydrate (CHO) and Glucose Metabolism
What Sample for Glucose Estimation is needed?
- This test can be done on serum. The serum should be separated within 30 minutes of collection.
- The Serum can be stored at 25 °C for 8 hours and at 4 °C for 72 hours.
- Oxalated blood can also be used. Preservative sodium fluoride may be added.
- The plasma can be stored at 25 °C for 24 hours (with preservative sodium fluoride).
What are the factors for the Stability of the glucose level?
- One milliliter of blood in an anticoagulant containing fluoride will remain stable for 3 hours.
- Oxalate plasma is stable at 2 to 8 °C for 48 hours.
- Serum is mainly used; it is stable for 8 hours at 25 °C and 72 hours at 4 °C.
- A 6- to 8-hour fast is required for a fasting sample.
What are the Indications for glucose estimation?
- This test is done to diagnose diabetes mellitus.
- This test is also done to evaluate and monitor diabetes mellitus.
How will you discuss the pathophysiology of the Carbohydrates (CHO)?
- Carbohydrates are major dietary components and an essential energy source.
- Glucose is controlled by insulin and glucagon.
- Glucose is low in the fasting state.
- The glucose = C6H12O6 = C6 (H2O)6.
- Lactose = C12H22O11 = C12 (H2O)11.
- The capacity of the body to store carbohydrates is limited:
- The liver can store only 10% of its wet weight.
- Muscles can store 5% of their wet weight.
- This store amount is only sufficient for half a day.
- Carbohydrates include sugar and starch.
- The salivary gland enzyme converts starch and glycogen into dextrin and maltose.
- The acidic pH of the stomach inhibits salivary amylase.
- Pancreatic alkaline secretion of amylase acts mainly on maltose and the disaccharides.
- Maltose, lactose, and sucrose are converted into:
- Glucose.
- Galactose.
- Fructose.
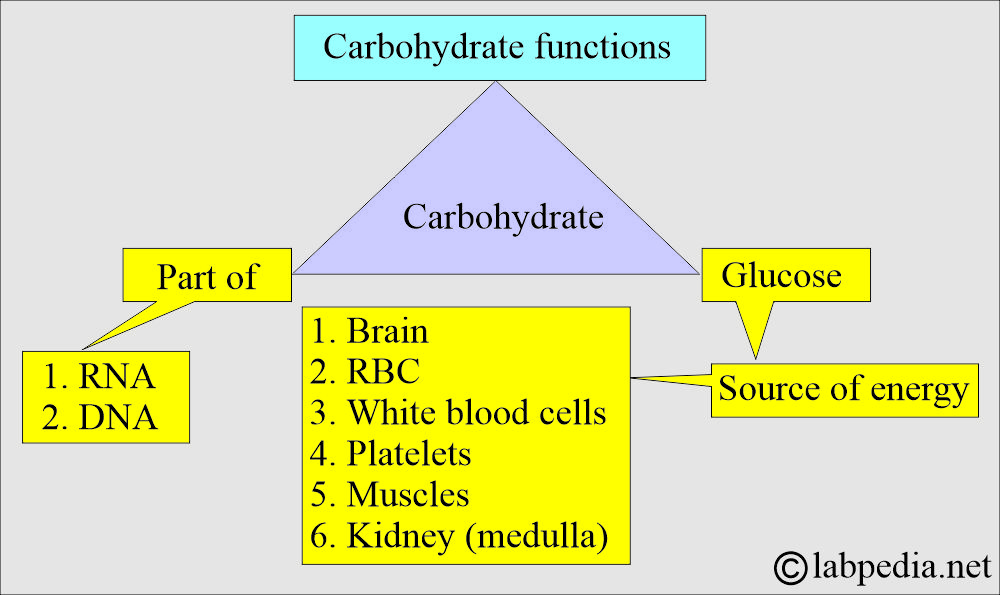
What are the functions of carbohydrates (CHO)?
- CHO is a component of RNA and DNA.
- CHO is the Source of energy, which is glucose.
- Under fasting conditions, the following organs depend only upon glucose as a source of energy:
- The brain is the main organ dependent on glucose.
- Red blood cells.
- White blood cells.
- Platelets.
- Kidney medulla.
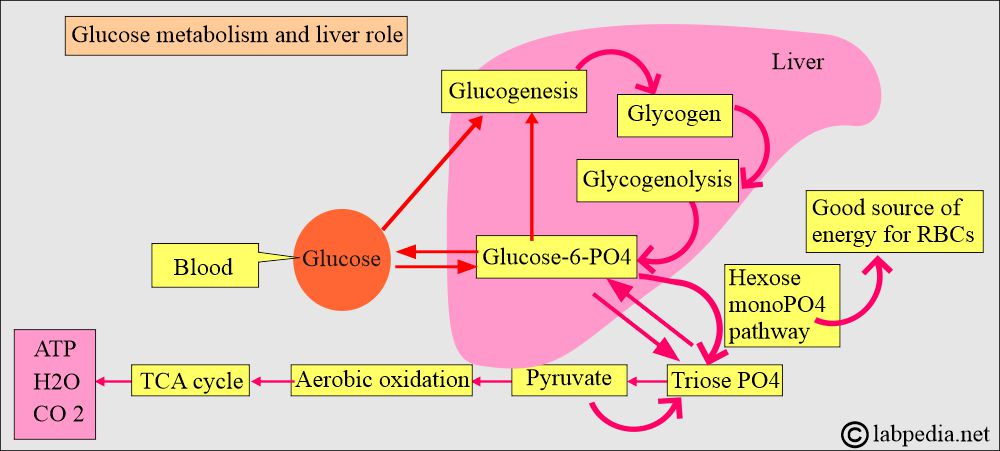
- Increased glucose level leads to its storage as glycogen in the liver.
- Decreased glucose level leads to glycogenolysis and forms glucose from the glycogen.
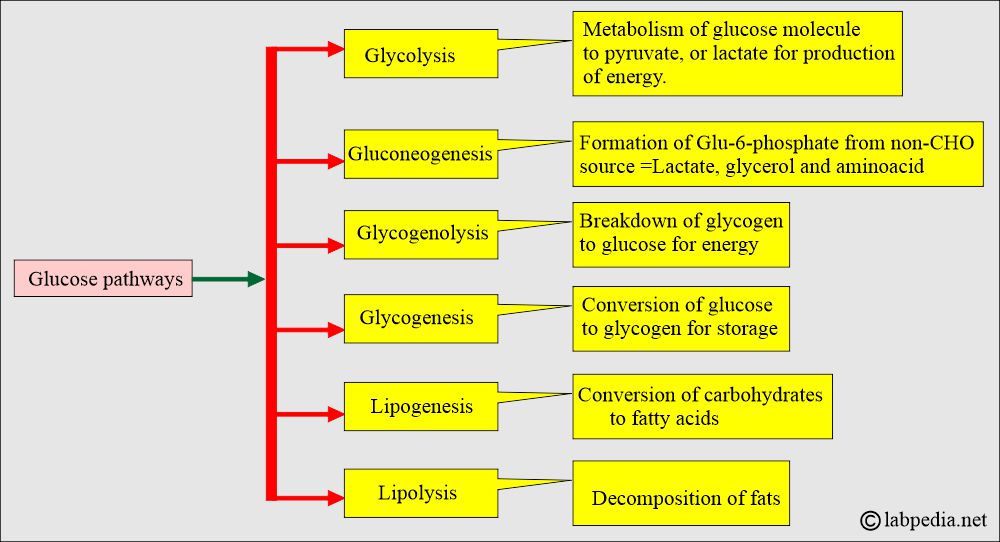
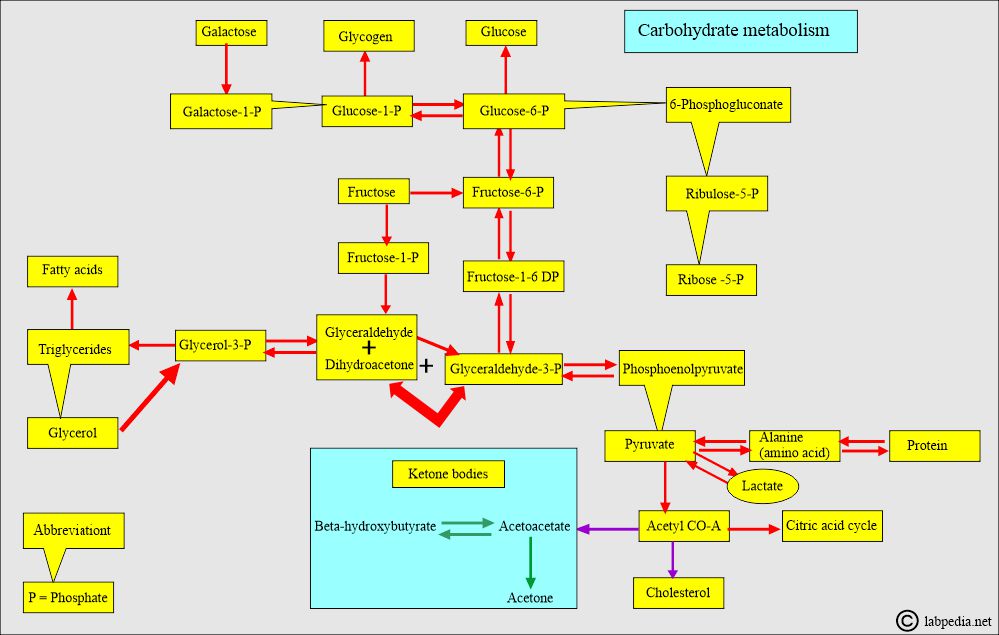
How will you discuss glucose metabolism?
- The breakdown of the following sources forms glucose:
- Grains.
- Starchy vegetables.
- Legumes.
- The body stores glycogen.
- Endogenous proteins.
- Excess glucose is converted into fat by adipose cells and stored in the adipose tissue.
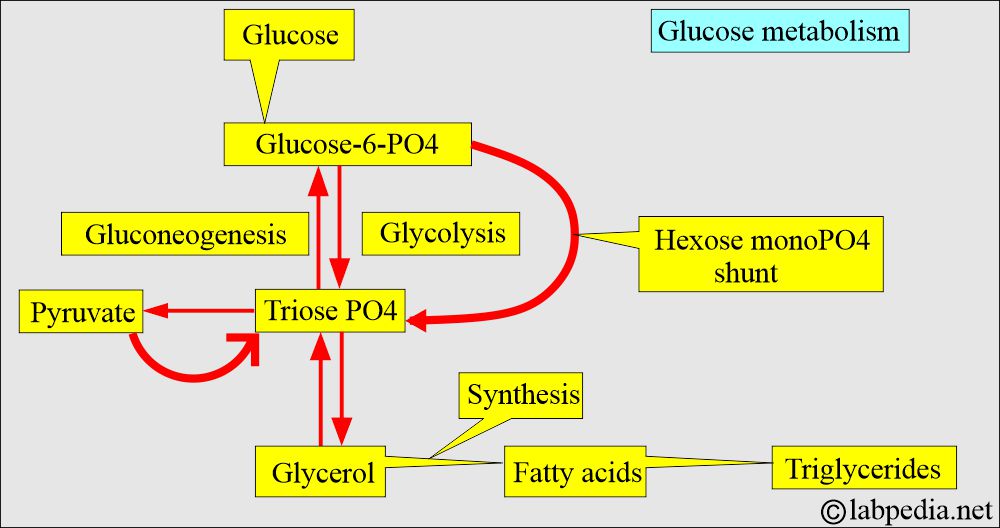
- The Triose pathway is the main junction where four pathways intersect and help maintain glucose levels.
- This is a complex enzymatic system, but glucose levels remain within the normal range.
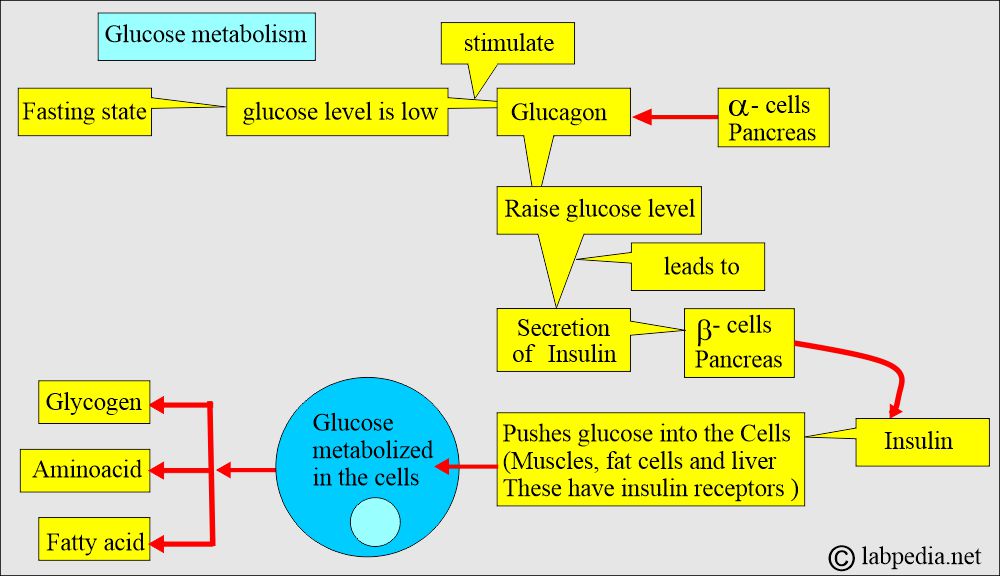
- The following diagrams illustrate that glucose metabolism is closely linked to the metabolism of fats and proteins.
- Glucose levels are controlled by insulin and glucagon.
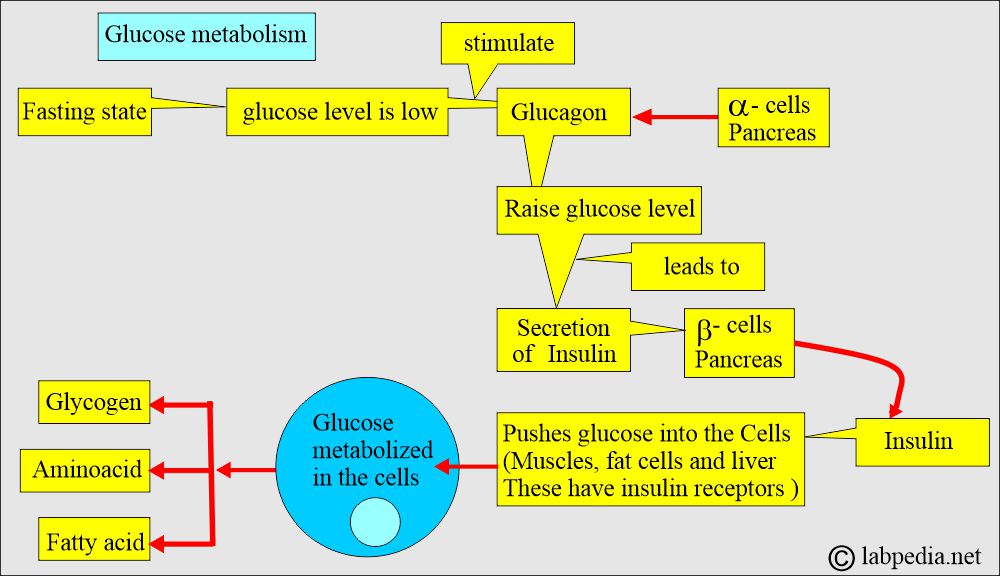
Pathophysiology of Glucagon and Insulin
Glucagon:
How will you define glucagon?
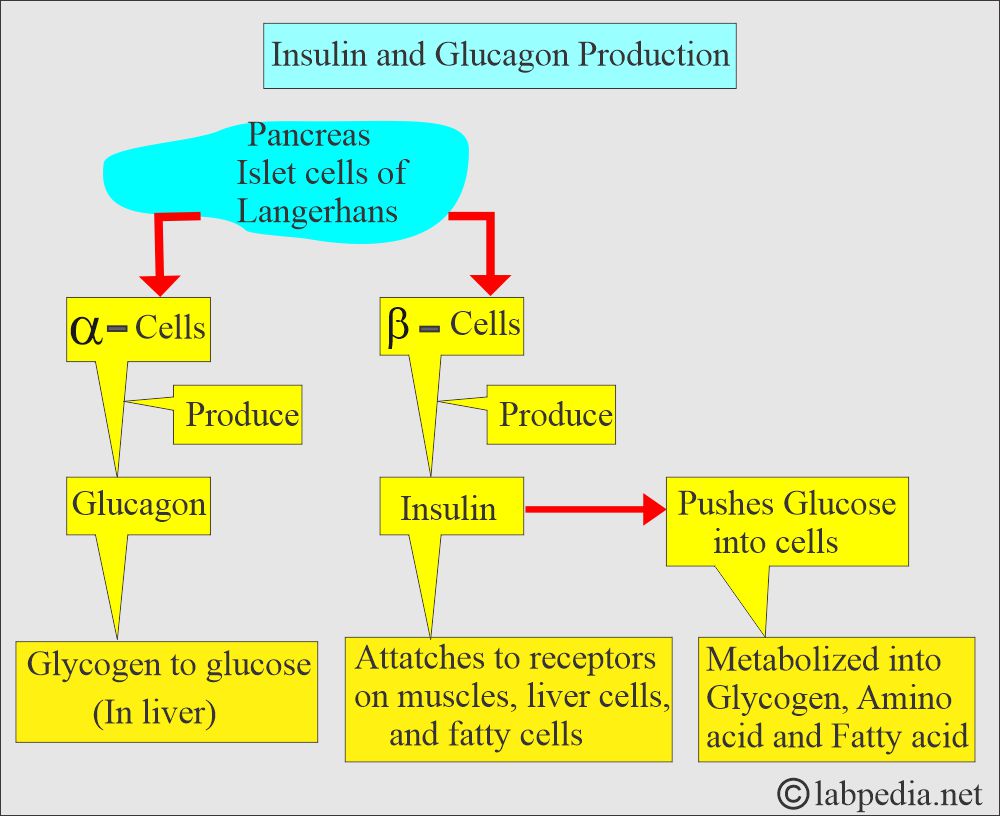
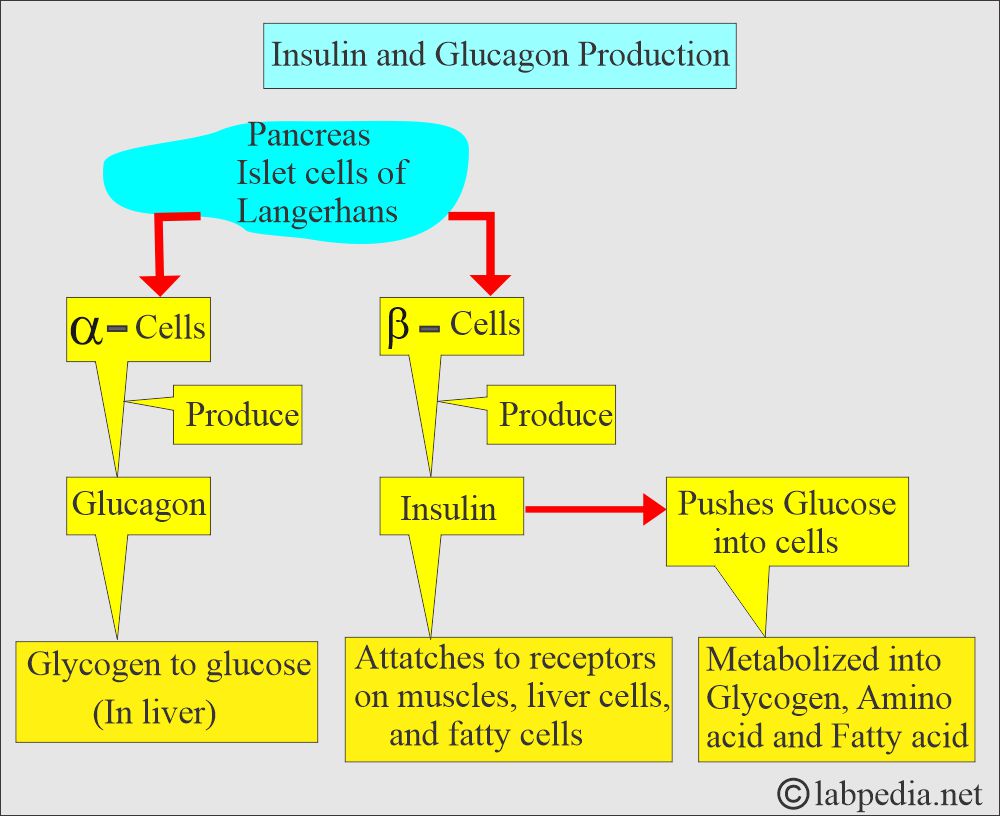
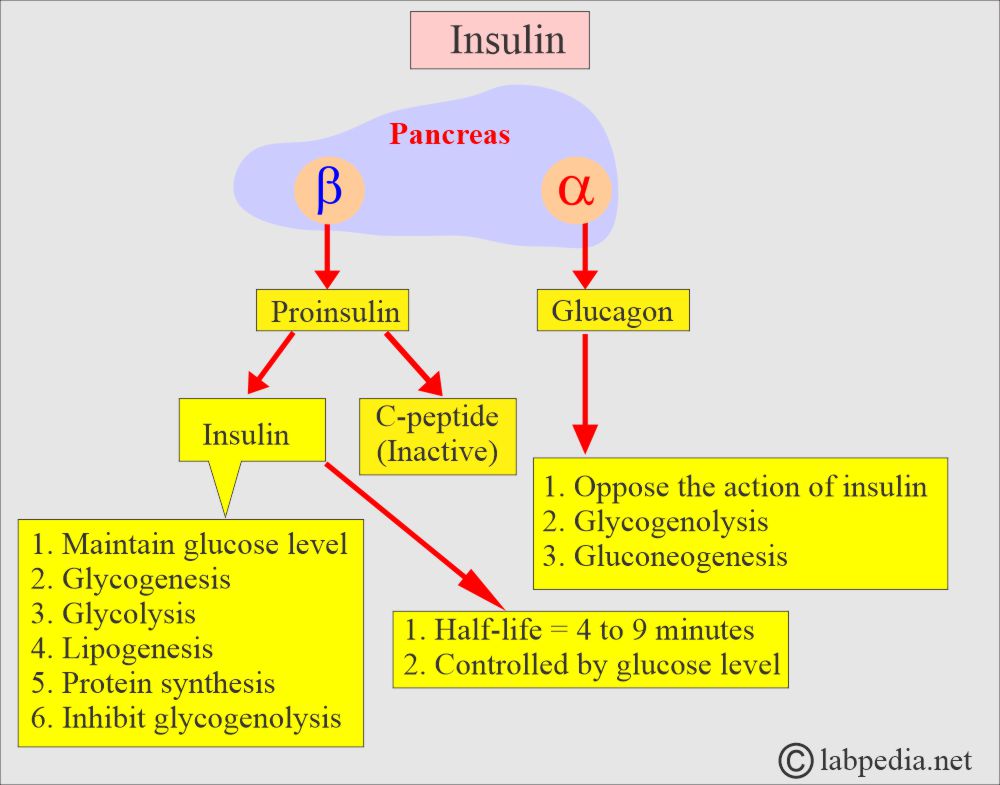
- Glucagon is produced by the Alpha (α) cells of the islets of Langerhans in the pancreas.
- Glucagon is a 29-amino acid polypeptide.
What is the role of Glucagon?
- The major target organ is the liver, which binds to a specific receptor and increases intracellular adenosine-5-monophosphate and calcium.
- Glucagon stimulates the production of glucose in the liver by glycogenolysis and gluconeogenesis.
- It also increases hepatic ketogenesis.
- The minor target organ is fat, which causes lipolysis.
- Glucagon secretion is controlled by glucose level.
- A low glucose level is stimulatory.
- A high glucose level is inhibitory.
- During fasting, protein and fat are broken down into glucose under the influence of Glucagon.
- In the case of long-standing diabetes mellitus, it impairs the glucagon response to hypoglycemia, leading to increased chances of hypoglycemia episodes.
- Insulin inhibits glucagon secretion from the pancreas.
Insulin:
How will you define Insulin and its action?
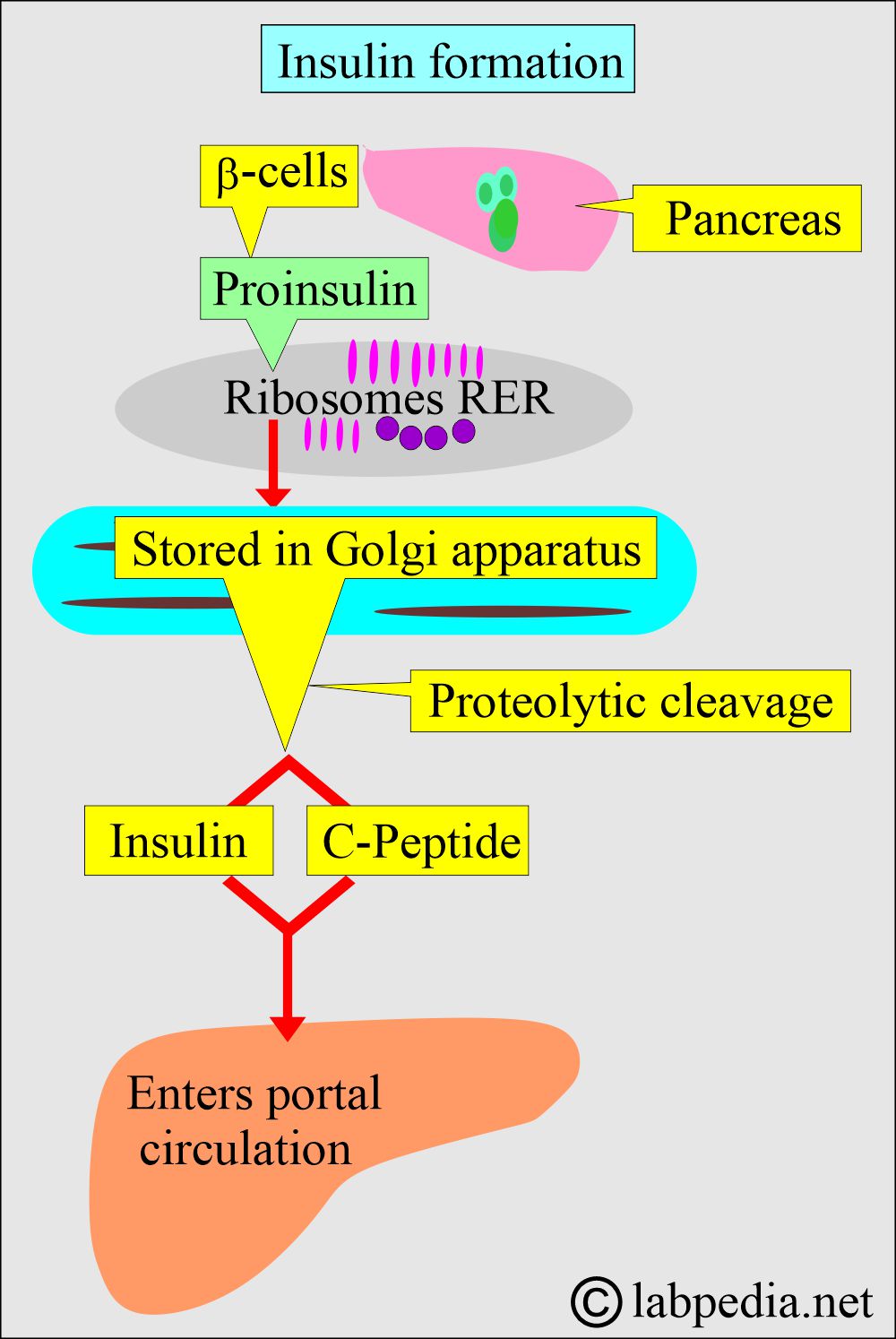
- Insulin is produced by the beta cells of the islets of Langerhans in the pancreas.
- Insulin is an anabolic hormone.
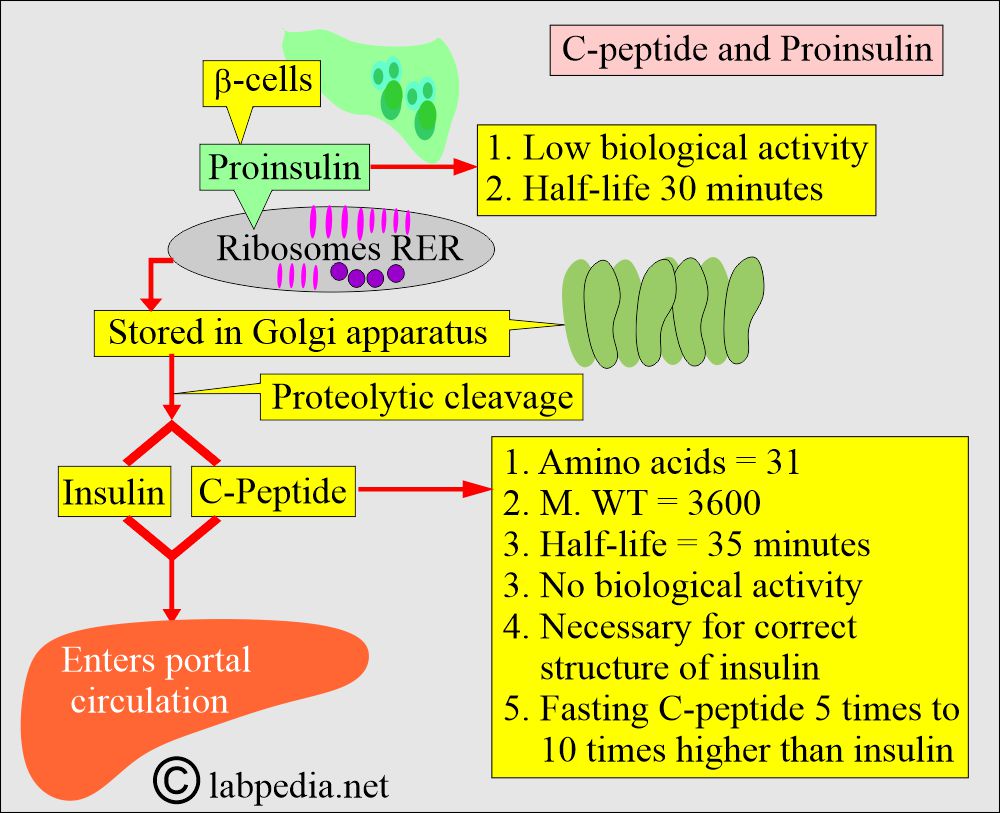
- First, proinsulin is formed in the ribosomes of the rough endoplasmic reticulum.
- Later on, stored in the Golgi apparatus.
- Proteolytic cleavage forms Insulin and C-peptide.
What is the role of Insulin and Diabetes Mellitus?
- It results from the abnormality in the production or use of insulin.
- β-cells of the pancreas produce insulin, and the abnormality of these Β-cells leads to diabetes mellitus:
- β-cells’ insulin production is deficient.
- Normal synthesis but abnormal release.
- Extra-pancreatic factors, such as peripheral tissue cell receptor dysfunction, can lead to resistance to insulin’s cellular action.
- Non-pancreatic hormones will affect insulin secretion or blood glucose metabolism.
- C-peptide has no biological activity and has a longer life than insulin.
-
- Fasting C-peptide concentration is fivefold to 10fold higher than insulin.
-
What is the action of Insulin on the cells?
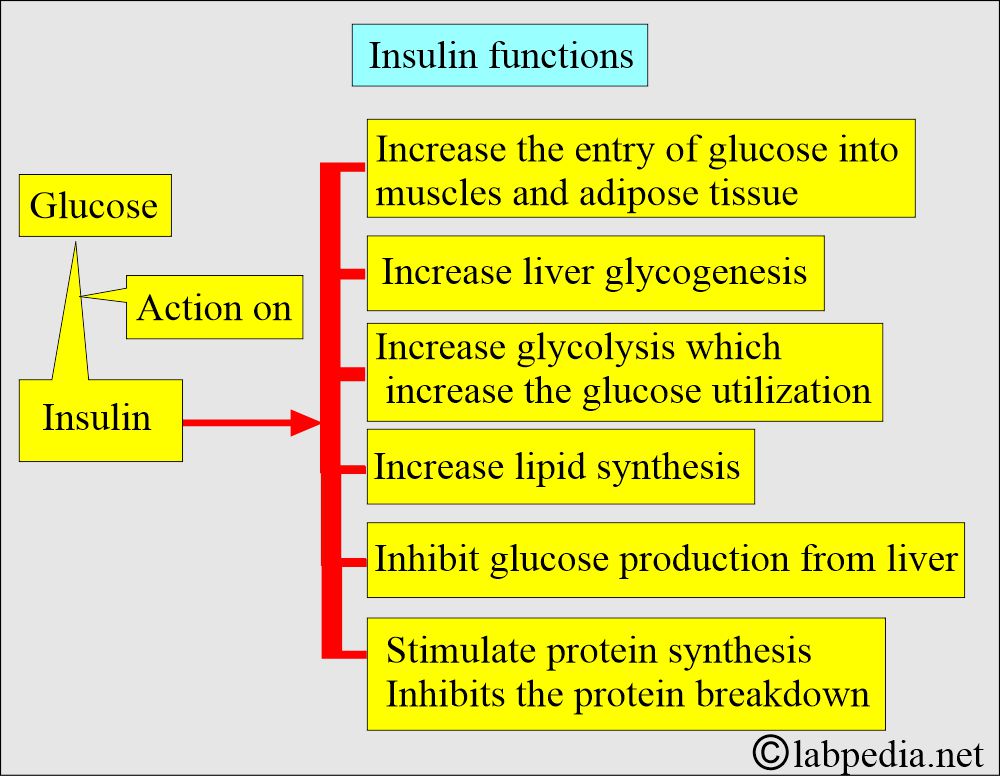
- Insulin binds to insulin receptors in muscle, liver, and fat cells.
- Insulin facilitates the uptake of glucose into cells, where it is metabolized into glycogen, amino acids, and fatty acids.
- Insulin lowers the plasma glucose level.
- Increased insulin lowers blood glucose levels, and a deficiency increases glucose levels.
- Other hormones, such as adrenocorticosteroids, ACTH, epinephrine, and thyroxine, can also affect glucose metabolism.
- The above hormones increase the plasma glucose level.
- Serum glucose levels are dependent on the time and relation to food intake.
- The glucose level is low in the fasting state.
- Glucose goes to the normal state after 2 hours of food intake.
- The concentration of glucose is higher in arterial blood than in venous blood.
- When fasting glucose is around 126 mg/dl, try to estimate the glucose level after an oral 75-gram glucose load.
- Now check the one-hour and two-hour samples.
- This oral glucose test will identify cases of Impaired Glucose Tolerance, allowing you to prevent the development of Diabetes Mellitus.
- The fasting level is between 100 to 126 mg/dl, which is called fasting hyperglycemia.
- The glucose level of 135 mg/dL is abnormal in the fasting state but returns to normal one hour after the meal.
What are the Lab findings in hyperglycemia (Diabetes mellitus)?
- Increased blood glucose.
- Increased urine-specific gravity.
- Decreased blood and urine pH values (acidosis).
- Increased blood and urine osmolality.
- Electrolyte disturbance.
- Ketones in the blood and urine.
Questions and answers:
Question 1: What is the source of the insulin?
Question 2: Does C-peptide have any activity in the control of glucose?
Question 3: What are the functions of glucagon?