Diabetes Mellitus:- Part 8 – Diagnostic Criteria, Microalbumin/creatinine ratio
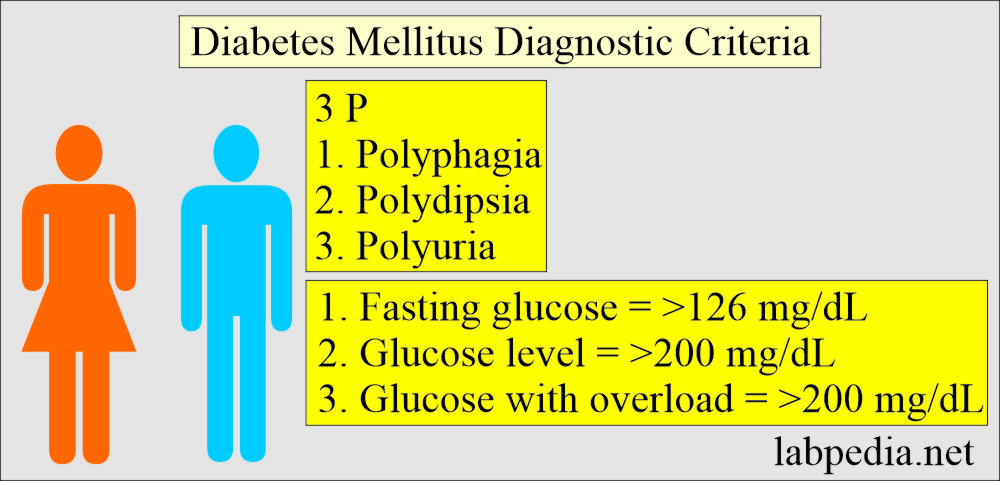
Diabetes Mellitus Diagnostic Criteria
What are the Diabetes Mellitus diagnostic criteria?
Any one of the following is needed to diagnose the diabetes mellitus:
- When there are classical signs and symptoms like polyphagia, polydipsia, and polyuria.
- With a glucose level of ≥200 mg/dL.
- Fasting glucose level is ≥126 mg/dL.
- 2-hour glucose level with overload is ≥200 mg/dL during the Oral glucose tolerance test.
Impaired fasting glucose (IFG) diagnostic criteria:
- When the fasting glucose level is 110 to 125 mg/dL.
Impaired glucose tolerance(IGT) diagnostic criteria:
- When Fasting glucose level <126 mg/dL.
- When 2-hour oral glucose tolerance is between 140 to 199 mg/dL.
How will you Manage the diabetes mellitus?
- The role of the lab is in the preclinical and for the management of diabetes mellitus.
- Regular check-ups of the glucose level and the urine.
- Regular lab workup will prevent complications from diabetes mellitus.
The preclinical workup of people prone to developing diabetes includes:
- This is advised in patients with a strong family history of diabetes mellitus.
- This will delay or may even prevent the onset of type 1 diabetes mellitus.
- American diabetes association recommends immune-related markers in the first-degree relatives of diabetics.
- Islet cell antibodies (ICA).
- Insulin autoantibodies.
- Glutamic acid decarboxylase antibodies.
- Protein tyrosine phosphatase antibodies.
- Genetic markers like HLA typing.
- Insulin secretion like:
- Fasting level.
- Pulses level.
- Response to a glucose challenge.
Clinical markers for the diagnosis of diabetes mellitus are:
- This mainly depends upon the presence of hyperglycemia.
- OGTT may help to classify diabetes mellitus.
- Insulin and C-peptide levels also help and assist in the classification of diabetes mellitus.
What are the clinical factors of diabetic patients?
- Blood glucose level.
- Oral glucose tolerance test.
- Presence of urine ketone bodies.
- Insulin level.
- Estimation of C-peptide level.
How will you Manage diabetes mellitus?
- The biochemical testing of the patient will help diagnose and monitor the therapy.
What are the management in the acute stage of diabetes mellitus?
- Diabetic ketoacidosis.
- Hypoglycemia.
- Hyperosmolar nonketotic coma.
How will you manage the chronic stage?
- This is to control blood glucose concentration to decrease chronic complications like:
- Nephropathy.
- Retinopathy.
- Vascular diseases.
- These complications can be controlled by:
- HbA1c.
- Urea.
- Creatinine.
- Urinary albumin excretion (microalbuminuria).
- Blood lipids level.
- Recommendations for the control of glycemic control are:
- HbA1c
- Normal = <6%
- The goal for diabetics = <7%
- Medical advise:
- If diabetes is unstable, then advise HbA1c quarterly.
- If diabetes is controlled, then advise HbA1c twice a year.
- HbA1c
- Microalbumin in the urine every year.
- This is the persistent microalbuminuria that is below the detection by the routine reagent methods.
- A lipid profile is advised yearly.
Microalbumin/creatinine ratio:
What are the Indications for the microalbumin/creatinine ratio?
- In the case of diabetes Mellitus.
- Patient with hypertension.
- Patients with heart disease.
- People over the age of 50 years.
- H/O smoking.
- In the case of obesity.
- A person with family H/O kidney diseases, hypertension, and diabetes mellitus.
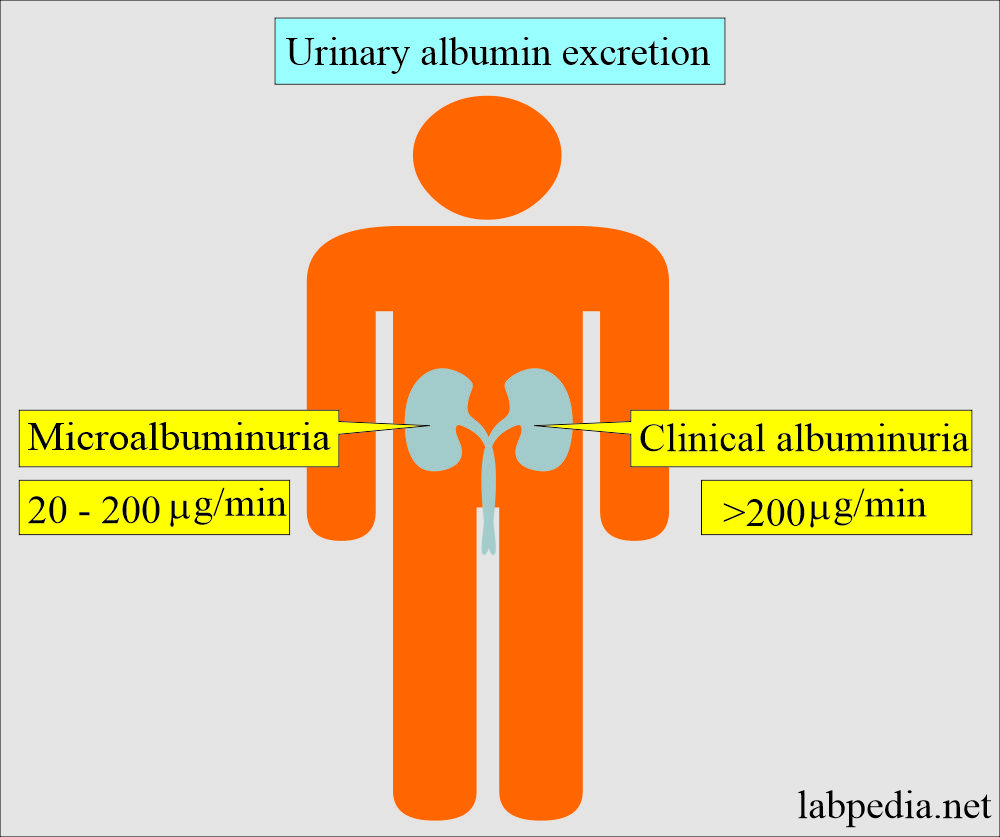
- >200 µg/min excretion in the urine indicates severe kidney disease (Nephropathy).
- Once diabetic nephropathy is diagnosed, then renal function deteriorates quickly.
- 30 to 300 mg/24 hours (20 to 200 µg/min) of urinary albumin is called microalbuminuria.
What is the mechanism of Urinary albumin excretion?
- Patients with diabetes mellitus are more prone to develop kidney diseases.
- Renal transplantation is needed in 1/3 of the patients with type 1 diabetes mellitus.
- Diabetes is the most common cause of end-stage kidney disease in the USA and Europe.
- Nephropathy is less common in type 2 diabetes.
- Early detection of diabetic kidney disease depends upon the detection of urinary albumin.
Urinary albumin excretion and interpretations:
| Clinical condition | Amount/minute | Amount/24 hours | Albumin mg/urine creatinine g (mg/g) |
| Normal | <20 µg/min | <30 mg/24 hours | <30 |
| Increased urinary albumin excretion | 20 200 µg/min | 30 to 300 mg/24 hours | 30 to 300 |
| Clinical albuminuria | >200 µg/min | >300 mg/24 hours | >300 |
What are the important facts about the Microalbumin/creatinine ratio?
- Patients with diabetes mellitus are tested yearly to check their kidney disease status.
- Albuminuria ≤0.3 g/day was detected only by the sensitive method.
- This is the random urine sample (spot urine) where albumin concentration in mg is divided by the creatinine in gram (mg/g).
- Albumin/creatinine ratio (mg/g) predicts overnight excretion rate >30 µg/minute.
- OR this is the ratio of albumin µg/L to creatinine mg/L; <30 is normal.
- A ratio of 30 to 300 indicates microalbuminuria.
- If this ratio is >300, it indicates macroalbuminuria.
- No doubt, 24-hour sampling is the gold standard method.
American diabetes association recommendations:
| Albumin excretion | Normal | Microalbuminuria | Clinical albuminuria |
| Albumin excretion | <20 mg/dL | 30 to 300 mg/dL | >300 mg/dL |
| Albumin/creatinine (g) | <30 | 30 to 300 | >300 |
Questions and answers:
Question 1: What is the most common complication of diabetes mellitus?
Question 2: How will you define diabetic nephropathy?

For “2-hours glucose level with overload is ≥200 ng/dL” isn’t that supposed to be mg/dL?
I am sure it is >200 mg/dL. It indicates diabetes mellitus.